The Varicella Zoster Virus
Oral health professionals should be prepared to note the signs and symptoms of shingles as it has implications for the provision of care.
This course was published in the March 2020 issue and expires March 2023. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Describe the epidemiology of a herpes zoster (shingles) infection.
- Identify risk factors for the development of shingles.
- Recognize the signs and symptoms of shingles.
- Know the current vaccine recommendations for the prevention of shingles.
Shingles is a viral infection caused by reactivation of the varicella zoster virus (VZV). Approximately 1 million cases of shingles are diagnosed each year in the United States, and these numbers continue to rise. The US Centers for Disease Control and Prevention (CDC) estimates that nearly one out of three people in the US will develop shingles in their lifetime.1 This condition typically affects individuals older than age 50. Symptoms may be extremely painful and can significantly interfere with daily activities. Oral health professionals may encounter an individual with shingles or be afflicted themselves and thus must be prepared to recognize the signs and symptoms of shingles, especially those appearing in and around the oral cavity.
VZV is associated with chickenpox and shingles (Figure 1). Initial exposure to the virus results in chickenpox (varicella zoster). Chickenpox is a highly contagious childhood disease. Upon exposure, VZV is contracted via airborne or direct contact transmission, resulting in a rash that typically lasts 3 days to 4 days. The rash presents as pus-filled blisters appearing anywhere on the body. The vesicles will rupture and scab prior to healing (Figure 2).1
The varicella vaccine has significantly reduced the incidence of chickenpox in the US. Prior to widespread vaccination programs, more than 90% of those younger than 17 experienced primary exposure to the varicella virus.2 The American Academy of Pediatrics currently recommends two doses of the chickenpox vaccine. The first dose is given at 12 months to 15 months and the second between the ages of 4 and 6. Two doses of the vaccine are also recommended for adults who have never had chickenpox.3
Once the signs and symptoms of chickenpox have subsided, VZV remains dormant within the nervous system.2 Shingles results when the inactive virus resumes replication in the nerves (Figure 3). The mechanisms responsible for reactivation are not fully understood; however, a number of risk factors are thought to trigger a shingles outbreak. According to the CDC, advanced age, stress, cancer, organ transplantation, human immunodeficiency virus, and immunosuppressive medications may increase susceptibility to herpes zoster, more commonly known as shingles.1 Exposure to an individual with active shingles lesions will not result in shingles infection. Shingles is a disease process resulting from reactivation of VZV already present in the body. It is not possible to get shingles from another person. However, the VZV present during active shingles can be spread through direct contact or airborne secretions. Therefore, pregnant women who have never had chickenpox or the vaccine, immunocompromised individuals, and those not previously exposed to varicella are at high risk of developing chickenpox from a person with active shingles. The virus that causes chickenpox and shingles is not the same virus responsible for cold sores, or sexually transmitted infections such as genital herpes.
SIGNS AND SYMPTOMS
The early signs and symptoms of shingles may include pain, itching, and burning prior to the appearance of the characteristic rash. When the rash appears, it begins as red spots and progresses to fluid-filled blisters. The virus follows nerve fibers that stem from the spinal column and affects the associated dermatome (the area of skin supplied by the nerve), resulting in a distribution of blisters on one side of the body.2 The rash usually progresses from the spine around to the front of the abdomen or chest, but may also involve the face, eyes, mouth, and ears. New blisters may continue to erupt over 3 days to 5 days. Scabbing of the blisters is an indication of healing and may occur within 2 weeks to 4 weeks.2
Most cases of shingles resolve without long-term complications. However, some individuals experience long-term pain after the blisters disappear. Postherpetic neuralgia is a significant complication characterized by lingering pain after disappearance of the rash.4 It is unclear why the pain of post-herpetic neuralgia persists. The persistent pain, although not due to ongoing infection, is believed to be a consequence of residual damage or inflammation in the nerve following resolution of the infection. Post-herpetic neuralgia can range from mild discomfort to a severe debilitating condition, resulting in diminished activity and subsequent clinical depression.5 Although most people experience one occurrence of shingles, it may reoccur.1
ORAL IMPLICATIONS
The trigeminal nerve innervates the teeth and other facial structures. Reactivation of VZV along this nerve presents a unique concern for oral health professionals because the lesions caused by a shingles outbreak may appear in the face and neck regions. Any of the three branches of the trigeminal nerve (maxillary, mandibular, or ophthalmic) may be affected during an occurrence of shingles.6


The virus tends to follow the path of one of the three branches. Oral lesions occur when the maxillary and mandibular branches are affected. Lesions on the forehead and around the eye occur when the ophthalmic branch is involved. Like the skin lesions on other areas of the body, oral lesions will also occur unilaterally. If any branch of the trigeminal nerve is affected, tooth pain may occur.7 Prodromal symptoms, such as fever, fatigue, or tooth pain unrelated to a dental infection, may precede the appearance of the rash and can interfere with an accurate dental diagnosis.7
Dental hygienists should be aware of the appearance of shingles on the face and neck, as they are often the first to meet the patient during a dental visit. Patients with shingles should be rescheduled to protect patients and staff from exposure to the virus. A comprehensive medical history at each dental visit is necessary to identify patients with a shingles outbreak or those who may be at high risk.
RAMSAY HUNT SYNDROME
A rare condition known as Ramsay Hunt syndrome (herpes zoster oticus) occurs when a shingles outbreak affects the facial nerve near the ear.8 In rare cases, reactivation of the VZV following dental treatment or orofacial surgery has been reported.9 The clinical appearance of Ramsay Hunt syndrome includes a vesicular rash around the ear or in the oral mucosa. In addition to the painful lesions occurring on ear, face or oral cavity, Ramsay Hunt syndrome can cause facial paralysis, and hearing loss in the affected ear.
According to the Mayo Clinic, the two major signs of this condition are:
- Fluid-filled blistered rash in and around one ear
- Paralysis or facial weakness on the same side as the affected ear10
Ramsay Hunt syndrome, which is caused by infection with herpes zoster, presents with vesicular lesions, dysfunction of the vestibulocochlear nerve, and facial paralysis.8 While Ramsay Hunt can affect all ages, those older than 60 who have already had chickenpox are at greatest risk. Dental treatment should be postponed until lesions have healed.
TREATMENT
Shingles affects each individual differently. There is no cure, but treatments are available to shorten the duration of the condition and lessen the risk of complications. Prescription antiviral drugs, including acyclovir and valacyclovir, are frequently prescribed and should be administered as soon as possible.11
Shingles can cause severe pain. Pain management options include several oral medications and over-the-counter analgesic treatments, including:
- Capsaicin topical patch
- Anticonvulsants, such as gabapentin
- Tricyclic antidepressants, such as amitriptyline
- Numbing agents, such as lidocaine, delivered via a cream, gel, spray, or skin patch
- Medications that contain narcotics (eg, codeine)
- Injections of corticosteroids and local anesthetics11
VACCINE INFORMATION
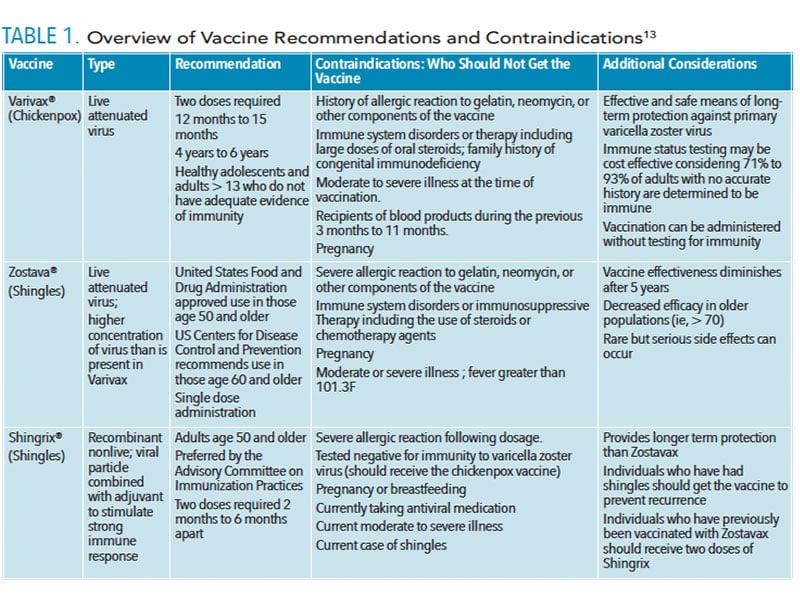
Two vaccines are used to prevent shingles: Shingrix® and Zostavax®. Zostavax was introduced in 2006 and is administered as a single dose. The vaccine is composed of a live but weakened (attenuated) form of the herpes zoster virus. Administration of this weak form is designed to trigger immune response and subsequent protection without producing disease.12 The use of attenuated virus approximates the natural immune response resulting in long-term immunity. However, the consequence of utilizing a live virus includes the remote possibility the vaccination may result in disease. For this reason, Zostavax is contraindicated in those who are immunocompromised.13
While Zostavax was originally recommended for those between the ages of 60 and 69, the range of use has been extended to include individuals between the ages of 50 and 69.14 The vaccine has been shown to provide effective short-term protection, however, the immune protection significantly declines after 5 years.12 Zostavax is not recommended for use during pregnancy or in those with immune system dysfunction.13
Shingrix® was approved by the US Food and Drug Administration in 2017. It is a nonliving recombinant formulation and given in a two-dose series.15 Recombinant vaccines are produced using only a portion of the virus rather than the entire structure. The viral component is combined with an adjuvant designed to stimulate the immune response and provide protection as if the entire virus were introduced.16 Using only a portion of the virus reduces the consequences associated with possible mutation and lowers the incidence of severe adverse reaction.16
Shingrix is considered safe and effective, and is recommended by the Advisory Committee on Immunization Practices for healthy adults age 50 and older.15–17 Shingrix should not be administered during pregnancy or breastfeeding or if the patient has experienced a previous severe allergic reaction to any of the components specifically gelatin and neomycin.15 Common side effects occur in one out of six people who get the vaccine and include soreness at the site of injection, fatigue, muscle pain, headache, and nausea. While side effects may be severe enough to interfere with normal activity, they resolve on their own within 2 days to 3 days. In clinical trials, serious adverse side effects were extremely rare.15
Chickenpox and shingles are two distinct consequences of the same virus. The clinical manifestations differ between children and adults due to differences in immune system function of each age group. The variance in the function and cells of the immune systems advise the need for different approaches to prevention in these populations.
Zostavax and Shingrix are shingles vaccines and should not be confused with Varivax, the vaccine for primary chickenpox. Varivax is administered in two doses for children 12 months and older. The vaccine is composed of live attenuated virus although in a much lower concentration than that of Zostavax. Varivax is effective in providing long-term immunity for children.16,17 Table 1 provides additional information on vaccines.13
![A table of vaccines and their schedule]() DENTAL HYGIENE CONSIDERATIONS
DENTAL HYGIENE CONSIDERATIONS
Oral health professionals may encounter patients with shingles. Patients identified with active lesions should not be treated in the dental office. Those with shingles should not be seen until all lesions have healed. Using an ultrasonic scaler or other aerosol-producing procedure could spread the virus to staff and other patients. A patient who presents with a blistering lesion whether on the body or in the oral region and is unaware of the cause should be referred to a physician for evaluation and treatment. Health care professionals with active chickenpox or shingles infection should discuss transmission risk with their health care provider. Recommendations may include avoiding contact with premature or low birthweight infants, immunocompromised individuals, or pregnant women with unknown immune status to VZV. Pregnant oral health professionals should consult with their physicians regarding a recommendation to avoid contact with patients who present with active VZV infection. The CDC provides comprehensive guidelines on preventing VZV transmission from herpes zoster in health care settings.18
CONCLUSION
Oral health professionals should be familiar with shingles and its oral and physical manifestations. Dental treatment for patients with active lesions should be rescheduled until all lesions have healed. Patients who present with undiagnosed lesions on the face, torso, or extremities should be referred to a medical provider for a definitive diagnosis and treatment. Oral health professionals can be a valuable resource for patients by providing information and education concerning the causes, treatments, and prevention of shingles.
REFERENCES
- United States Centers for Disease Control and Prevention. About Shingles—Herpes Zoster. Available at: cdc.gov/shingles/about/index.html. Accessed February 25, 2020.
- Eshleman E, Shahzad A, Cohrs RJ. Varicella zoster virus latency. Future Virol. 2011;6:341–355.
- American Academy of Pediatrics. Clinical Report. Prevention of varicella: recommendations for use of varicella vaccines in children, including a recommendation for routine 2-dose varicella immunization schedule. Pediatrics. 2007;120:221–231.
- Johnson RW, Rice AS. Clinical practice. Postherpetic neuralgia. N Engl J Med. 2014;371:1526–33.
- Schmader KE, Dworkin RH. The epidemiology and natural history of herpes zoster and postherpetic neuralgia. In: Herpes Zoster: Postherpetic -Neuralgia and Other Complications. In: Watson C, Gershon A, Oxman M, eds. Herpes Zoster: Postherpetic Neuralgia and Other Complications. London, Germany: Adis, Cham; 2017.
- Ibsen O, Andersen Phelan J. Oral Pathology for the Dental Hygienist. 7th ed. St. Louis: Elsevier; 2018:130.
- Thakur I, Shilpa B, Satheesha R, Koppula S. Herpes zoster infection of maxillary nerve: A case report. Journal of Indian Academy of Oral Medicine and Radiology. 2017;29:156–158.
- Singh G, Subhalakshmi V, Balasubramanian S, Patidar M, Ealla KR. Ramsay hunt syndrome: A diagnostic challenge for general dental practitioners. Contemp Clin Dent. 2017;8:337–339.
- Furuta Y, Ohtan F, Fukuda S, Inuyama Y, Nagashima K. Reactivation of varicella-zoster virus in delayed facial palsy after dental treatment and oro-facial surgery. J Med Virol. 2000;62:42–45.
- Mayo Clinic. Ramsay-Hunt Syndrome– Symptoms and Causes. Available at mayoclinic.org/diseases-conditions/ramsay-hunt-syndrome/symptoms-causes/syc-20351783. Accessed February 24, 2020.
- Mayo Clinic. Shingles—Symptoms and Causes—Diagnosis and Treatment. Available at: mayoclinic.org/diseases-conditions/shingles/diagnosis-treatment/drc-20353060. Accessed February 24, 2020.
- Immunization Action Coalition. Available at: immunize.org/askexperts/experts_zos.asp. Accessed February 24, 2020.
- US Centers for Disease Control and Prevention. Recommendations and Vaccine Specifics for Healthcare Professionals. Available at: cdc.gov/vaccines/vpd/shingles/hcp/Zostavax® /hcp-vax-recs.html. Accessed February 24, 2020.
- Leung J, Harpaz R, Molinari NA, Jumaan A, Zhou F. Herpes zoster incidence among insured persons in the United States, 1993-2006: evaluation of impact of varicella vaccination. Clin Infect Dis. 2011;52:332–340.
- US Centers for Disease Control and Prevention. What Everyone Should Know About Shingles Vaccine. Available at: cdc.gov/vaccines/vpd/shingles/public/index.html. Accessed February 24, 2020.
- Wang L, Zhu L, Zhu H. Efficacy of varicella (VZV) vaccination: an update for the clinician. Ther Adv Vaccines. 2016;4:20–31.
- Dooling KL, Guo A, Patel M, et al. Recommendations of the Advisory Committee on Immunization Practices for use of herpes zoster vaccines. MMWR Morb Mortal Wkly Rep. 2018;67:103–108.
- Centers for Disease Control and Prevention. Shingles (Herpes Zoster) Preventing Varicella-Zoster Virus (VZV) Transmission from Herpes Zoster in Healthcare Settings. Available at: cdc.gov/shingles/hcp/hc-settings.html Accessed February 24, 2020.
From Dimensions of Dental Hygiene. March 2020;18(3):32–35.