Treating Patients with Immune Thrombocytopenic Purpura
This autoimmune blood disorder can have significant effects on oral health and the provision of professional dental care.
This course was published in the August 2011 issue and expires August 20194 The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Define immune thrombocytopenic purpura (ITP).
- Understand the etiology, symptoms, diagnosis, and treatment options of ITP
- Describe how ITP can affect oral health.
- Identify medications used in the treatment of ITP and how they can negatively impact oral health.
- Recognize when dental treatment may be contraindicated for patients with ITP.
Immune thrombocytopenic purpura (ITP) is an autoimmune blood disorder that causes low blood platelet counts, which increases the risk of bleeding of the mucous membranes and skin (mucocutaneous bleeding).1 ITP is a rare condition that affects approximately 23 out of every 100,000 people in the United States.2 However, ITP does not always cause noticeable symptoms, which impedes formal diagnosis. As a result, the total number of cases may be under-reported.3 Because ITP can significantly affect oral health, dental hygienists should be aware of its etiology, symptoms, diagnosis, and treatment options.
A normal platelet count in the human body falls between 150,000 platelets to 400,000 platelets per microliter (mcL) of blood.4-6 Thrombocytopenia occurs when an individual’s platelet count falls below 150,000/mcL.6 Many factors can induce thrombocytopenia including: acute or chro nic alcohol exposure; use of specific medications such as heparin, sulfonamides, quinidine, and aspirin; and chronic liver disease.7 Other conditions such as leukemia, human immunodeficiency virus (HIV), and systemic lupus erythematosus can induce secondary forms of ITP.1Immune thrombocytopenic purpura may be acute, chronic, or refractory.8 Acute ITP predominantly occurs in children.8 In the majority of acute cases, ITP occurs after a viral infection or vaccination and usually resolves on its own without treatment within 6 months.1,8
Chronic ITP is most common among adults and affects more women than men, at a ratio of 3:1.9 Chronic ITP is frequently idiopathic.8,10 The incidence of chronic ITP also increases with age and is the most common type experienced by older adults.3,6 Refractory ITP is a form of chronic ITP that does not respond to clinical treatment.8
ETIOLOGY
Although the complete etiology of ITP is not entirely known, the autoimmune blood disorder is caused by platelet antibodies that cause an increase in platelet destruction and a decrease in platelet production.11 Membrane proteins found on the surface of the platelets are recognized as foreign by the body, which causes the immune system to make autoantibodies and cytotoxic T-cells to fend off the perceived invaders.7 What causes the autoantibodies to form initially is not understood, but environmental and genetic factors may be involved.9,12 The autoantibodies then coat specific glycoproteins that are found on circulating platelets.7 These coated platelets are subsequently removed by the reticuloendothelial system, which includes the spleen and liver.7 Thrombocytopenia results when the coated platelets are removed from the body faster than platelets can be produced.12 While a normal platelet has a lifespan of 7 days, a platelet in an individual with ITP lives less than 2 days.13
Thrombocytopenia is also caused by a decrease in platelet production. Thrombopoietin is a protein made in the liver that circulates through the blood stream to trigger the cells within the bone marrow to make more platelets.14 These platelet-producing cells are called megakaryocytes.14 In ITP, the anti-platelet antibodies and cytotoxic T-cells not only cause the platelets to be rapidly destroyed, but they may also disrupt thrombopoiesis and prevent megakaryocytes from producing enough platelets to replace those lost.12 This decrease in platelet production in combination with the rapid destruction of platelets can cause dangerously low platelet counts.12
SYMPTOMS
Symptoms of ITP fall into two categories: dry purpura and wet purpura.15 Purpura is the appearance of purple or reddish-blue spots that occur within the skin or mucosa caused by spontaneous hemorrhages of blood (Figures 1-4).4 The spots are circumferential in shape and range from 0.1 cm to 5.0 cm in diameter.16 Dry purpura occurs on the skin, and appears as bruising and petechiae (small red spots on the skin caused by small hemorrhages).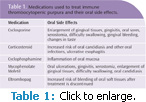 4
4
Wet purpura manifests as bleeding of the mucous membranes, such as the mouth and eyes.15 An individual with ITP may also have spots of petechiae.4 Other symptoms of ITP include nose bleeds, heavy menstrual cycles, bleeding of the oral mucosa, gastrointestinal bleeding, and intracranial hemorrhage.7 People with ITP may also bruise very easily and have blood in their urine.4 The presence and extent of bleeding usually depends on the severity of the thrombocytopenia.11 Individuals who are at greatest risk of serious bleeding have a platelet count less than 10,000/mcL.8 However, there are many people with ITP who do not exhibit noticeable symptoms.3
Table 2. Symptoms of adrenal crisis.23
• Fatigue
• Weakness
• Headache
• Confusion
• Nausea and vomiting
• Fever
• Abdominal pain
• Tachycardia
• Hypotension
• Sweating
• Dehydration
TREATMENT
The key goal of treating ITP is to help people achieve a safe (not necessarily normal) platelet count in order to prevent bleeding.10 Because there is no cure for chronic ITP, treatment decisions are based on the severity of the disease and patient-related factors.10 When determining treatment and management options, clinicians need to consider the extent and risk of bleeding, complications that can occur with therapy, possible side effects, lifestyle factors, access to care, and patient expectations.17 Multiple treatment options are available that target different aspects of the immune response.12 Many of the medications that help increase platelet count have oral side effects (Table 1).4
Fortunately, the overall mortality rate for ITP is less than 1%.18 Often, the morbidity and mortality caused by ITP treatment are worse than those caused by the disease itself.18 ITP patients who have persistent severe thrombocytopenia that does not respond within the first 2 years of treatment are at a much higher risk of complications than those whose ITP is more responsive to or does not require treatment.19
IMPLICATIONS FOR DENTAL PROFESSIONALS
Dental professionals need to take special precautions when treating patients with ITP. Obtaining a detailed medical and dental history, including the patient’s current and past history of treatment and medication use, as well as the patient’s current platelet count, is crucial to providing safe and effective treatment.20
There are several oral manifestations that can present in patients with ITP, including spontaneous gingival bleeding, petechiae, and purpura.4 Petechiae and hemorrhages can occur on the palate, tonsil area, and buccal mucosa (Figures 1-4).21 The gingiva may be edematous, soft, and friable.23 Gingival bleeding during dental treatment may be difficult to control.21
Patients’ platelet counts should be above 50,000/mcL to safely perform routine dental treatments.20 Dental surgery and any other procedures that could cause bleeding, including periodontal debridement, are contraindicated in patients who have a platelet count below 50,000/mcL.20 Dental treatment should be postponed until laboratory results show improvement in patients’ platelet counts and decreased risk of bleeding.4 Patients may need to have a platelet transfusion, corticosteroid treatment, or other therapies to increase their platelet count to an acceptable level for oral surgery.20
Medications that induce an anti-coagulant or anti-platelet effect (including aspirin ibuprofen, warfarin, and heparin) should be avoided, and patients should be instructed to avoid these medications at home.20 As noted in Table 1, medications used in the treatment of ITP may produce oral side effects.
| Intraoral photographs of a 35-year-old man with immune thrombocytopenic purpura who presented for dental hygiene care with a blood platelet count of 60,000 platelets per microliter of blood. | |
 |
 |
 |
 |
Patients with ITP should have restorative and endodontic treatment when possible versus extraction and surgical procedures due to their increased risk of bleeding and infection.20 Patients must also be educated about proper dental plaque control to prevent inflammation, bleeding, and infection.22 Caries management programs should be implemented in patients with increased risk and may include dietary recommendations, fluoride, and placement of pit and fissure sealants.20
Corticosteroids are commonly administered to patients who suffer from ITP, and they can cause adrenal insufficiency and adrenal crisis. Adrenal glands are part of the endocrine system and appear at the top of the kidneys, while the adrenal cortex is part of the adrenal gland that makes specific hormones, such as cortisone and aldosterone.23 When patients take systemic corticosteroids, their bodies may stop producing these hormones naturally in the adrenal cortex, resulting in suppression of the adrenal gland (adrenal insufficiency).24 Adrenal insufficiency occurs when patients with ITP have been taking corticosteroids for a long period or if they are not properly tapered off of the medication.24 Adrenal insufficiency becomes problematic in the dental setting when patients are exposed to very stressful events, including dental procedures and dental surgeries.24 When the body reacts to stress, it requires increased production of the cortisol hormone from the adrenal cortex to properly deal with the stress.23 Patients who take corticosteroids for an extended period do not produce as much adrenocorticotropic hormone and their adrenal cortex may atrophy.23 If a dental procedure causes a heightened level of stress, they may go into adrenal crisis—a lifethreatening condition.23
Dental professionals need to know whether a patient is taking systemic corticosteroids and the dosage. They must also be able to assess whether a dental procedure will be considered stressful. Dental professionals should also be able to recognize the symptoms of adrenal crisis and be prepared to respond to this medical emergency (Table 2).23 Acting quickly is imperative if a patient exhibits signs of adrenal crisis. The patient should be placed in a supine position, his or her airway, breathing, pulse, and blood pressure need to be assessed, and emergency medical services must be called.23 While waiting for medical services to arrive, the patient’s vital signs should be monitored, he or she should be provided with emotional support, and oxygen should be administered at 2 L to 5 L per minute via a nasal canula.23
To prevent adrenal crisis from occurring, dental professionals must take a detailed medical history of the patient, understand the procedures the patient will undergo, and asses the patient’s feelings about dental treatment. The patient’s physician should be contacted prior to performing dental surgery.24 A patient with ITP may need to increase his or her dose of steroids prior to the dental procedure. Dental professionals should also confirm that the patient took the recommended dose of the steroid medication within 2 hours of the dental procedure.24
SUMMARY
ITP is a complex disorder that can be difficult to diagnose and treat. Researchers are trying to discover the true etiology of this disorder in order to find better treatment options and a possible cure. ITP can occur in people of different genders, ages, and ethnicities. While some may not exhibit any symptoms, others may be plagued with noticeable signs, such as purpura and excessive bleeding. Dental professionals should be aware of the symptoms of this disorder, understand its oral health implications, and recognize when dental treatment is contraindicated in order to provide patients with the best care possible and to prevent any adverse events from occurring during the dental appointment.
REFERENCES
- Cines DB, Blanchette VS. Immune thrombocytopenic purpura. New Engl J Med. 2002;346:995-1008.
- Feudjo-Tepie MA, Robinson NJ, Bennett D. Prevalence of diagnosed chronic immune thrombocytopenic purpura in the US: analysis of a large US claim database: a rebuttal. J Thromb Haemost. 2008;6:711-712.
- Abrahamson PE, Hall SA, Feudjo-Tepie M, Mitrani-Gold FS, Logie J. The incidence of idiopathic thrombocytopenic purpura among adults: a population-based study and literature review. Eur J Haematol. 2009;83:83-89.
- Ibsen OAC, Phelan JA, Vernillo AT. Oral manifestations of systemic diseases. In: Ibsen OAC, Phelan JA, eds. Oral Pathology for the Dental Hygienist. 5th ed. St. Louis: Saunders Elsevier; 2009:286-319.
- National Board of Medical Examiners. Laboratory values. Available at: www.nbme.org/PDF/SubjectExams/LabReferenceValues.pdf. Accessed July 23, 2011.
- Terranova L, Gerli G, Cattaneo M. Platelet disorders in the elderly. In: Balducci L, Ershler W, de Gaetano G, eds. Blood Disorders in the Elderly. Cambridge, UK: Cambridge University Press; 2008:420-433.
- Pruemer J. Epidemiology, pathophysiology, and initial management of chronic immune thrombocytopenic purpura. Am J Health-Syst Pharm. 2009;66:S4-S10.
- Provan D, Newland AC. Acquired disorders affecting megakaryocytes and platelets. In: Wickramasingher SN, McCullough J, eds. Blood and Bone Marrow Pathology. London: Elsevier Science Limited; 2003:525-555.
- Warkentin TE, Kelton JG. Platelet life cycle: qualitative disorders. In: Handin RI, Lux SE, Stossel TP, eds. Blood: Principles and Practice of Hematology. 2nd ed. Philadelphia: Lippincott Williams & Wilkins; 2003:983-1047.
- Stasi R, Provan D. Management of immune thrombocytopenic purpura in adults. Mayo Clin Proc. 2004;79:504-522.
- Cines DB, Bussel JB, Liebman HA, Luning Prak ET. The ITP syndrome: pathogenic and clinical diversity. Blood. 2009;113:6511-6521.
- Zhou B, Zhao H, Yang RC, Han ZC. Multidysfunctional pathophysiology in ITP. Crit Rev Oncol Hemat. 2004;54:107-116.
- Fogarty PF, Dunar CE. Thrombocytopenia. In: Rodgers G, Young N, eds. The Bethesda Handbook of Clinical Hematology. 2nd ed. Philadelphia: Lippincott Williams & Wilkins; 2010:250-251.
- Platelet Disorder Support Association. Disease details. Available at: www.pdsa.org/about-itp/disease-details.html. Accessed July 23, 2011.
- Provan D. Characteristics of immune thrombocytopenic purpura: a guide for clinical practice. Eur J Haematol. 2009;82:8-12.
- Mirowski GW, Rozycki TW. Common skin lesions of the head and neck. In: Regezi JA, Sciubba JJ, Jordan RCK, eds. Oral Pathology: Clinical Pathologic Correlations. 4th ed. St. Louis: Saunders Elsevier; 2003:285-407.
- Provan D, Stasi R, Newland AC, et al. International consensus report on the investigation and management of primary immune thrombocytopenia. Blood. 2010;115:168-186.
- Newland A. Emerging strategies to treat chronic immune thrombocytopenic purpura. Eur J Haematol. 2007;80:27-33.
- Portielje JEA, Westendorp RGJ, Kluin- Nelemans HC, Brand A. Morbidity and mortality in adults with idiopathic thrombocytopenic purpura. Blood. 2001;91:2549-2554.
- Vaisman B, Medina AC, Ramirez G. Dental treatment for children with chronic idiopathic thrombocytopenic purpura: a report of two cases. Int J Paediat Dent. 2004;14:355-362.
- Klokkevold PR, Mealey BL. Influence of systemic disorders and stress on the periodontium. In: Newman MG, Takei HH, Klokkevold PR, Carranza FA. Carranza’s Clinical Periodontology. 10th ed. St. Louis: Saunders Elsevier; 2006:284-311.
- Guzeldemir E. The role of oral hygiene in a patient with idiopathic thrombocytopenic purpura. Int J Dent Hygiene. 2009;7:289-293.
- Grimes EB. Adrenal insufficiency and crisis. In: Medical Emergencies: Essentials for the Dental Professional. Upper Saddle River, NJ: Pearson Prentice Hall; 2009:197-204.
- Weinberg MA, Westphal C, Fine JB. Endocrine and hormonal drugs. In: Oral Pharmacology for the Dental Hygienist. Upper Saddle River, NJ: Pearson Prentice Hall; 2008:371-404.
From Dimensions of Dental Hygiene. August 2011; 9(8): 20-23.



