Treating Patients With Coronary Stents
As the number of patients receiving stents continues to rise, it becomes increasingly important for oral health professionals to possess a deep understanding of coronary heart disease, the role of stents in its management, and related dental considerations.
This course was published in the November/December 2023 issue and expires December 2026. The author has no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
AGD Subject Code: 149
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Identify the prevalence of coronary artery disease in the United States.
- Note the etiology and pathophysiology of coronary atherosclerosis.
- Explain the evolution of percutaneous interventions, including balloon angioplasty and stents.
- Discuss the use of dual antiplatelet therapy.
- State the dental considerations in patients presenting with cardiovascular stents.
Cardiovascular disease refers to several types of heart conditions, with coronary artery disease (CAD) being the most common in the US. Recent advances in therapies and pharmaceuticals have decreased morbidity and increased survival rates. As a result, the prevalence of CAD is expected to increase. The treatment of CAD has been transformed by the introduction of percutaneous coronary intervention, including the placement of coronary stents.2
CAD is the leading health problem in the US and the world.2 Characterized by the development of atherosclerotic plaques inside the coronary vessels, CAD derives initially from arterial injury, and then continues on the following path:
- Chronic endothelial injury. Atherosclerosis is an inflammatory disorder of the cellular lining of the arteries initiated in response to chronic injury.
- Endothelial dysfunction. Monocytes adhere to an area of injured endothelium. The monocytes then migrate into the intima of the vessel and become macrophages. Lipids derived from plasma low-density lipoproteins also enter through the injured endothelium, forming extracellular deposits.
- Smooth muscle emigration from media to intima , with macrophage activation.
- Macrophages and smooth muscle cells then engulf lipid molecules to become foam cells, which are characteristic features of the fatty streak.
- The arrival of the smooth muscle cells triggers a coalescence of the foam cells and small extracellular pools of lipid into a larger pool or lipid core.3
- Plaques (atheromas) may grow outwardly away from the lumen of the artery or inwardly toward the lumen. With inward proliferation, the size of the lumen is progressively reduced.3
A number of risk factors are associated with atherosclerosis, including male gender (until female menopause), age 75 and older, a family history of cardiovascular disease, hyperlipidemia, hypertension, cigarette smoking (as the single most contributing modifiable risk factor), physical inactivity, obesity, insulin resistance and diabetes mellitus, stress, and depression.3,4
Treatment
Medications, coronary artery bypass grafting, and nonsurgical angioplasty followed by placement of a coronary stent are all ways to treat CAD. Also referred to as ischemic heart disease, CAD is commonly treated with drugs, such as nitroglycerine, which is used to treat angina as well as prevent an acute attack. Aspirin and other anti-platelet and anticoagulant medications (antithrombotic agents) may be used as blood thinners to prevent blood clots in the coronary arteries. Angiotensin-converting enzyme inhibitors, beta blockers, calcium channel blockers to treat hypertension, and statins to lower cholesterol are also common interventions.5,6
When the root of the problem is narrowed or occluded lumen, physical intervention may be required. The use of percutaneous coronary intervention is one of the most common procedures in the treatment of CAD. It includes revascularization procedures and devices used to restore patency to blocked or occluded arteries.
Coronary artery bypass grafting surgery involves harvesting a segment of donor artery or vein, and grafting the segment to the segment of the coronary artery affected; thus providing revascularization by means of “bypassing” the occluded portion of the artery.
Angioplasty is a procedure used to restore patency (state of openness) to blocked or occluded coronary arteries caused by CAD. Angioplasty is an older form of percutaneous coronary intervention. The intervention uses a balloon catheter that is inserted into the partially blocked artery. The balloon is then inflated, which compresses the atheromatous plaque against the vessel wall, gaining greater luminal diameter.
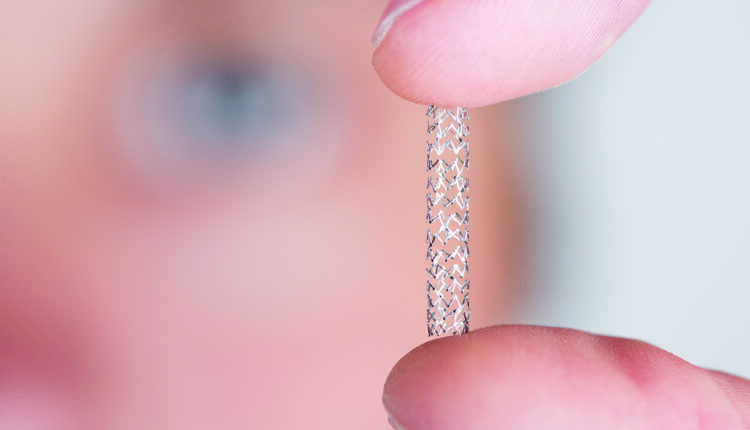
More than 600,000 coronary stents are implanted during percutaneous coronary interventions annually in the US.7 A coronary artery stent is a small, metal mesh tube that expands inside the artery. A stent is often placed during or immediately after angioplasty to restore openness of the coronary artery. The majority of individuals undergoing angioplasty have a coronary stent placed as evidence shows that stent placement yields the most effective results in ensuring patency.8,9
Percutaneous Interventions: Stenting
Stents are placed in a coronary artery for two reasons: to restore blood flow and vessel patency following a myocardial infarction and to treat atherosclerotic plaque buildup by restoring vessel patency. A stent encompasses a solid scaffold that prevents vessel closure due to elastic recoil or vessel occlusion. The polymers required in stent application must be biocompatible and noninflammatory. Coatings should also facilitate controlled and predictable drug loading and release without altering the activity of the drug.8 Currently, three types of stents are used: bare-metal, drug-eluting, and bioresorbable.
Bare-metal stents are composed of metal mesh tubing that functions as a permanent scaffold to help maintain mechanical patency of the vessel; however, bare-metal stents do not prevent endothelial proliferation that results in restenosis.3
Drug-eluting stents were initially composed of stainless steel platforms with thick struts that were then coated with a drug-eluting polymer.10 Second-generation drug-eluting stents were developed to overcome the problem of stent thrombosis.10 Improved platforms were made of cobalt-chromium or platinum chromium, allowing for thinner strut design.
This new generation of stents used polymers that were more biocompatible. New coating drugs were also used in second-generation stents, enhancing endothelial coverage in the healing process. The –limus drugs (zotarolimus, everolimus, and novolimus) were eluted from the polymer for approximately 1 month.2 Second-generation drug-eluting stents significantly reduce rates of myocardial infarction and target lesion revascularization and stent thrombosis compared with first-generation versions.
Concerns regarding the risk of late and very late stent thrombosis and the need for prolonged dual antiplatelet therapy (DAPT) remained.11 To address the hypersensitivity reaction to the durable polymers used in second-generation drug-eluding stents, new nonpolymer third-generation drug-eluting stents using biodegradable polymers and a semisynthetic analog of sirolimus were developed. These biodegradable polymer-based stents received approval from the US Food and Drug Administration in 2015.2
Fourth generation drug-eluting stents are made of fully bioresorbable scaffolds. This generation of drug-eluting stents is designed to deliver antiproliferative drugs through elution over a period of time following percutaneous coronary intervention, with full resorption over time.12 The aim of ongoing research lies in the development of stents that improve the outcomes of CAD.

Dual Antiplatelet Therapy
DAPT refers to a drug regimen used following drug-eluting stent implantation to prevent stent thrombosis and ischemic events and is prescribed to 1.2 million patients each year.13,14 DAPT is following stent implantation.13 The therapy combines aspirin and a novel oral antiplatelet P2Y12 receptor inhibitor (platelet aggregate inhibitor). This class of drugs includes clopidogrel, prasugrel, and ticagrelor.
Current guidelines recommend DAPT combining long-term, low-dose aspirin (75 to 100 mg/day) and a P2Y12 receptor inhibitor therapy (clopidogrel, ticagrelor, or prasugrel) for at least 12 months in patients with acute coronary syndrome undergoing percutaneous coronary intervention, regardless of stent type.15
DAPT remains integral to preventing thrombotic complications and restenosis with percutaneous coronary intervention. According to the current American Heart Association/American College of Cardiology guidelines, recommendations for DAPT following percutaneous coronary intervention are as follows:15
- In patients with stable ischemic heart disease (SIHD) treated with DAPT after bare-metal stent implantation, P2Y12 inhibitor therapy (clopidogrel) should be given for a minimum of 1 month.
- In patients with SIHD treated with DAPT after drug-eluting stent implantation, P2Y12 inhibitor therapy (clopidogrel) be given for at least 6 months.
- In patients with SIHD treated with DAPT after bare-metal stent or drug-eluting stent implantation who have tolerated DAPT without a bleeding complication and who are not at high bleeding risk, continuation of DAPT with clopidogrel for longer than 1 month in patients treated with bare-metal stent or longer than 6 months in patients treated with drug-eluting stents may be reasonable.
- In patients treated with DAPT, a daily aspirin dose of 81 mg (range of 75 mg to 100 mg).
- In patients with acute coronary syndrome treated with DAPT after bare-metal stent or drug-eluting stent implantation, P2Y12 inhibitor therapy (clopidogrel, prasugrel, or ticagrelor) should be given for at least 12 months. In patients treated with DAPT, a daily aspirin dose of 81 mg (range of 75 mg to 100 mg).
Considerations for Dental Management
Oral health professionals should be knowledgeable about cardiovascular stents and the use of antiplatelet therapy in stent maintenance. A thorough health history is the first step. This is an opportunity to assess risks associated with a potential bleeding event. Clinicians must consider all aspects of patient care, including existing comorbidities, stability of presenting conditions (such as stable angina or controlled hypertension), and the magnitude of the proposed dental procedure. The patient’s medication regimen should be ascertained prior to consulting with the patient’s prescribing physician to discuss changes to antiplatelet therapy.
The primary concern related to dental management is the possibility of a bleeding event with DAPT. While DAPT addresses the problem of restenosis following stent placement, there is a risk for significant postoperative bleeding. A meta-analysis of studies on the dental management of patients on DAPT concluded that while postoperative bleeding is exacerbated with DAPT, the risk can be managed with proper local hemostasis measures.16
Patients using aspirin (as single-anticoagulant therapy or DAPT) should avoid taking nonsteroidal anti-inflammatory drugs, as this may exacerbate gastrointestinal bleeding.3,6 Any alteration in antiplatelet therapy should be done in consultation with the prescribing physician.
The interruption of antiplatelet and anticoagulant therapy increases the risk of bleeding and ischemic events, particularly in patients with stent implantation. Early discontinuation of DAPT is not recommended. Elective procedures should be postponed for 1 year following stent placement.17 In the event that postponement is not possible, single-anticoagulant therapy in the form of aspirin should be continued during the perioperative period to prevent stent thrombosis.
Antibiotic prophylaxis is not recommended prior to invasive dental procedures for patients with a coronary artery stent; however, there is still uncertainty surrounding this issue.18 This is considered a secondary prophylaxis, and would be recommended for patients with these devices if they undergo incision and drainage of infection at other sites, such as a dental abscess, or replacement of an infected device.18
Conclusion
As the prevalence of cardiovascular stents as a treatment for CAD continue to grow, oral health professionals will likely encounter patients presenting with a history of cardiovascular stent placement. As such, oral health professionals should be knowledgeable about CAD, the risk of bleeding events related to treatments, and possible modifications to dental care.
References
- Heidenreich PA, Trogdon JG, Khavjou OA. AHA policy statement: forecasting the future of cardiovascular disease in the United States. Circulation. 2011;123:933–944.
- Canfield J, Totary-Jain H. 40 Years of percutaneous coronary intervention: history and future directionsJ J Pers Med. 2018;3:2-9.
- Little J, Falace D, Miller C, Rhodus N. Dental Management of the Medically Compromised Patient. 8th ed. St Louis: Elsevier; 2018.
- Johns Hopkins Medicine. Atherosclerosis. Available at: hopkinsmedicine.o/g/health/conditions-and-diseases/atherosclerosis. Accessed October 17, 2023.
- Driver M. Coatings for Biomedical Applications. Philadelphia: Woodhead Publishing; 2012; 223–250.
- Haveles E. Applied Pharmacology for the Dental Hygienist. 8th ed. St. Louis: Elsevier; 2020.
- Kaplan J. Kaplan’s Essentials of Cardiac Anesthesia. 2nd ed. St. Louis: Elsevier. 2017.
- Serruys PW, Morice MC, Kappetein AP, et al. Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. N Engl J Med. 2009;360:961-972.
- Dhruva SS, Parzynski CS, Gamble GM, et al. Attribution of adverse events following coronary stent placement identified using administrative claims data. J Am Heart Assoc. 2020;18;9:e013606.
- Ho M, Chen C, Wang C, Chang S, Hsieh M. The development of coronary artery stents: from bare-metal to bio-resorbable types. Metals. 2016:6:1-15.
- Garg S, Serruys PW. Cardiac stents. J Am Coll Cardiol. 2010;56:S1–42.
- Toyota T, Morimoto T, Shiomi H, et al. Coronary stents current status. J Am Coll of Cadiol. 2010;56:10S.
- Zahid M, Memon M, Tappiti M, et al. Duration of dual antiplatelet therapy after stent implantation, still an enigma: systematic review of randomized clinical trials. Cureus. 2021;11:e19549.
- Husted S. Antithrombotic therapy for long-term secondary prevention of acute coronary syndrome in high-risk patients. Ther Clin Risk Manag. 2015;11:263–277.
- Levine GN, Bates ER, Bittl JA, et al. ACC/AHA guideline focused update on duration of dual antiplatelet therapy in patients with coronary artery disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2016;134:e123–e155.
- Li L, Zhang W, Yang Y, Zhao L, Zhou X, Zhang J. Dental management of patient with dual antiplatelet therapy: a meta-analysis. Clin Oral Investig. 2019;23:1615-1623.
- Grines CL, Bonow RO, Casey Jr DE, et al. Prevention of premature discontinuation of dual antiplatelet therapy in patients with coronary artery stents: A science advisory from the American Heart Association, American College of Cardiology, Society for Cardiovascular Angiography and Interventions, American College of Surgeons, and American Dental Association, with representation from the American College of Physicians. J Am Dent Assoc. 2007:138:652–655.
- Wilson WR, Gewitz M, Lockhart PB, et al. Prevention of viridans group streptococcal infective endocarditis. A scientific statement from the American Heart Association. Circulation. 2021;143:e963–e978.
From Dimensions in Dental Hygiene. November/December 2023; 21(10):28-31



