 PEOPLEIMAGES/ISTOCK/GETTY IMAGES PLUS, ANULLA/ISTOCK/GETTY IMAGES PLUS
PEOPLEIMAGES/ISTOCK/GETTY IMAGES PLUS, ANULLA/ISTOCK/GETTY IMAGES PLUS
Treating Dry Mouth
Dry mouth/xerostomia are common conditions that need a multifaceted approach to mitigate symptoms.
This course was published in the July 2018 issue and expires July 31, 2021. The author has no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Define the role of saliva in the oral cavity.
- Identify the signs and symptoms of dry mouth.
- Discuss the etiology of xerostomia.
- List the treatments for dry mouth.
THE AMERICAN ACADEMY OF PERIODONTOLOGY
INTRODUCTION
Saliva is critical for the maintenance of good oral health and it is integral to successful communication and healthy nutrition. A lack in saliva’s quantity and quality, known as hyposalivation, can significantly alter quality of life. Oral health professionals can expect to encounter patients with xerostomia with increased frequency. Patients often subjectively feel they have dry mouth when clinically salivary flow seems normal, leading clinicians to underestimate the impact and severity of xerostomia. To help patients with xerostomia, clinicians should be proactive in asking patients if they have symptoms of dry mouth, especially if risk factors are present.
We hope you find this article interesting, valuable to your clinical practice, and beneficial to your patients, as the author has reviewed signs and symptoms, etiology, and treatment designed to help patients find temporary relief from xerostomia and reduce their risk of dental caries.
The Colgate-Palmolive Company is delighted to have provided an unrestricted educational grant to support this continuing article series in collaboration with the American Academy of Periodontology.
—Matilde Hernandez, DDS, MS, MBA
Scientific Affairs Manager
Colgate Oral Pharmaceuticals
Oral health professionals need to be prepared to help patients with dry mouth/xerostomia relieve symptoms and reduce related oral disease risks.
FROM THE AMERICAN ACADEMY OF PERIODONTOLOGY
Dry mouth, or xerostomia, is a common side effect of medications, chemotherapy treatment, and several ailments. Dry mouth may initially seem inconsequential to many patients; however, because saliva is key to the removal of food debris and plaque bacteria, a reduction in its flow can trigger the development of dental caries and, in some instances, the onset of periodontal disease. For oral health professionals, an understanding of xerostomia’s causes and treatments is essential to knowing a patient’s risk factors for oral complications. In this article, educator and American Academy of Periodontology (AAP) member periodontist Hana Gadalla, BDS, MSc, provides an overview of xerostomia and its impact on oral health and how the dental team can ease dry mouth symptoms. Once again, the AAP is proud to work with Dimensions of Dental Hygiene and Colgate-Palmolive to help ensure patient health and wellness.
—Steven R. Daniel, DDS
President, American Academy of Periodontology
Saliva plays an important role in protecting the oral cavity, supporting health, and maintaining balance in the oral environment.1 Secreted by major and minor salivary glands,saliva is composed of 99% water and 1% organic and inorganic molecules.2 The right quantity and quality of saliva are important to the proper lubrication of the oral cavity.3,4 Saliva also assists in cleaning the oral cavity, balancing the demineralization/remineralization process, and improving taste and digestion.5 Reduction in the quantity of the salivary flow leads to dry mouth, while xerostomia refers to the perception of dry mouth with or without an actual decrease in salivary flow levels.
Daily saliva secretion rates range between 500 mL and 700 mL.6 Dry mouth is usually associated with a reduction in salivary flow due to salivary gland hypofunction.7 Severity of dry mouth symptoms range from oral discomfort to significant oral disease.7 The main symptoms associated with xerostomia are frequent thirst; difficulty eating, swallowing, and speaking; oral irritation; pain; and burning sensation in oral mucosa.8 Diminished salivary flow is common among older adults.9 Approximately, 30% of patients age 65 and older have been diagnosed with dry mouth.10 Xerostomia is also more common among women than men.11
SIGNS AND SYMPTOMS

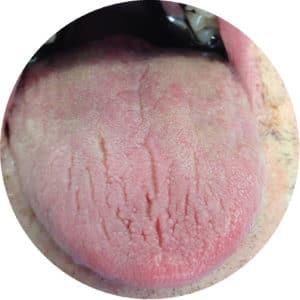
A detailed medical and dental health history is essential to early detection of dry mouth and identification of potential underlying causes.7 When performing an oral examination on those complaining of dry mouth symptoms, dry and friable oral mucosa and dry and fissured tongue may be present.7 However, patients may experience a 50% loss in protective saliva before they notice dry mouth symptoms.12 Such symptoms include:10,13,14
- Thick ropey saliva
- Dry mucosa in which the gloves stick to the mucosal surface during clinical examination (Figure 1)
- Fissured tongue
- Atrophy of the filiform papillae (Figure 2)
- Oral malodor
- Dysgeusia
- Glossodynia
- Cracking and fissuring of the oral mucosa
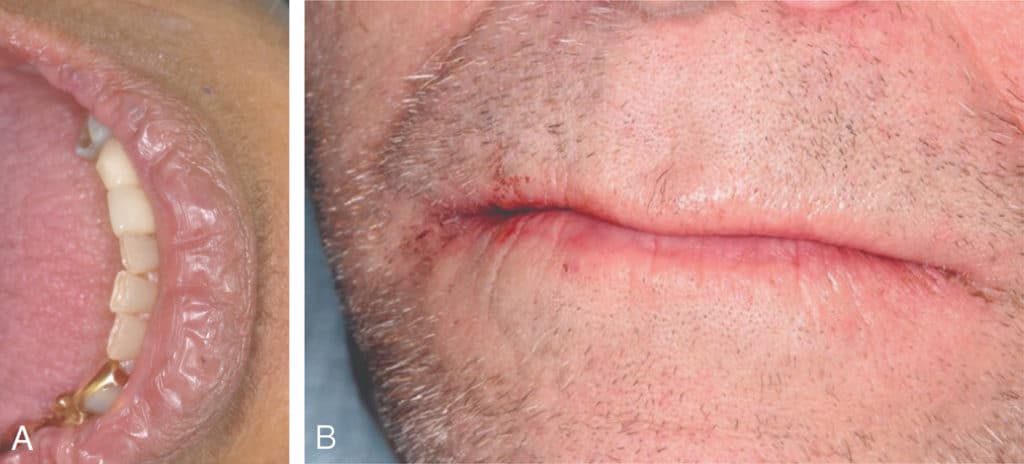
- Cracked, peeled, or atrophic lips (Figure 3)
- Angular cheilitis (Figure 4)
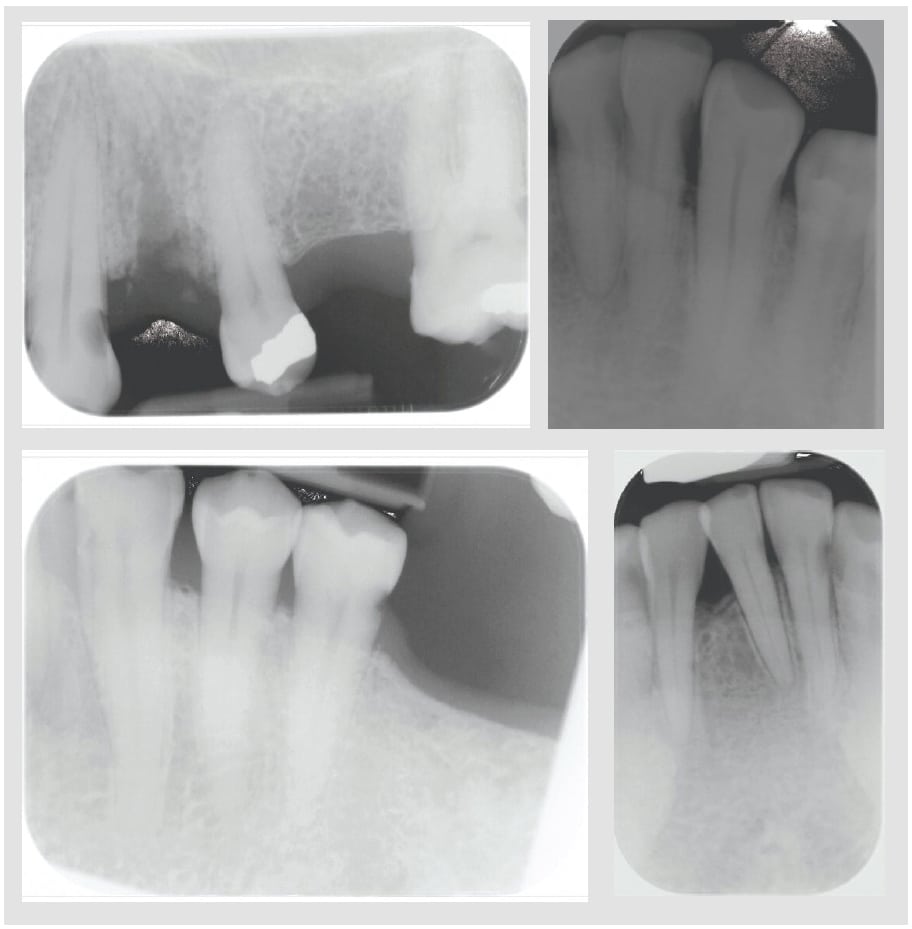
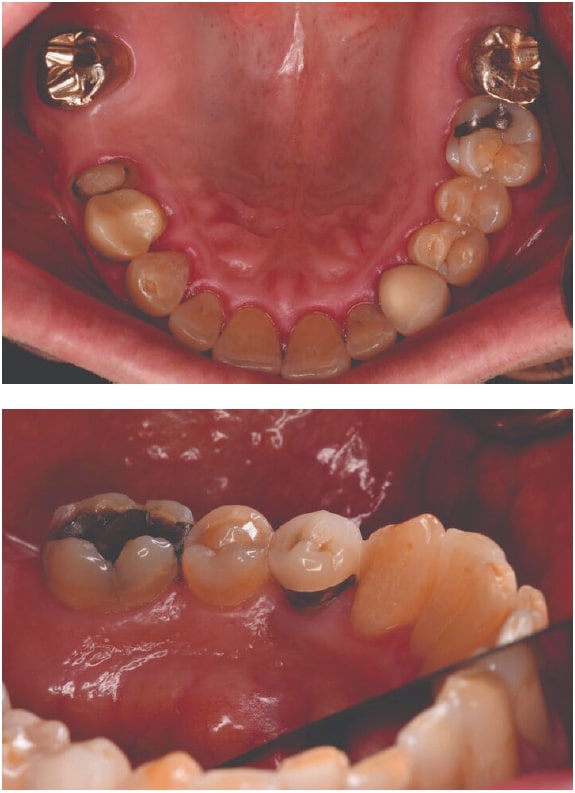
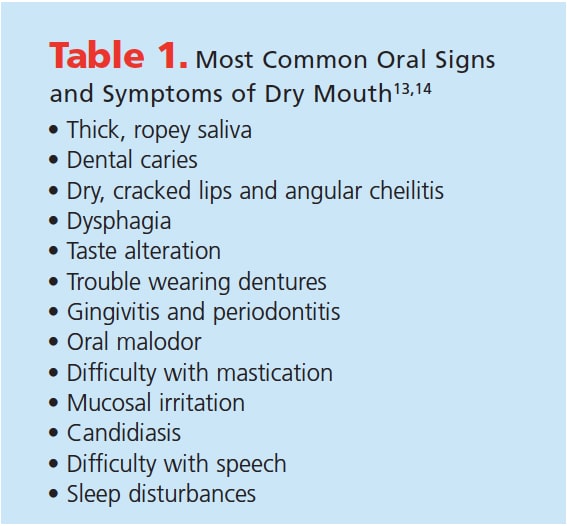
Increased incidence of oral candida infection is noted in patients with dry mouth due to a reduction in the antimicrobial activity of saliva.1 Patients with xerostomia also experience increased caries risk, especially for root caries (Figure 5).15,16 Xerostomia also raises the risk of dentinal hypersensitivity and enamel demineralization.17,18 Some patients may also be unable to wear dentures or have poorly fitting removable prostheses.7 Xerostomia can lead to plaque accumulation, periodontal diseases (Figure 6), and sleep problems.18,19 Table 1 lists the most common oral signs and symptoms of dry mouth.13,14

ETIOLOGY OF XEROSTOMIA
Medication usage. More than 500 drugs from 42 drug categories and 56 subcategories can cause xerostomia (Table 2).7,13,20–22These drug classes include: antihistamines, decongestants, tricyclic antidepressants, antihypertensives, anticholinergics, pain medications, diuretics, muscle relaxants, and antidepressants.23 Patients taking more than four daily prescription medications are at high risk for xerostomia.24 If dry mouth is diagnosed in a patient who is taking one of or more of these medications, consultation with his or her physician is necessary to see if the drug can be substituted. Drug substitution may help reduce the intensity of dry mouth effects (eg, selective serotonin-reuptake inhibitor antidepressants may cause less salivary hyposalivation than tricyclic antidepressants).21,25 Patients taking anticholinergic medications may see a reduction in dry mouth symptoms if they are taken during the day, rather than at night, and in divided doses, rather than one large single dose.19
Age. It was previously thought that age in and of itself was a risk factor for salivary gland hypofunction or xerostomia.19 However, it is now known that the high rate of xerostomia in older adults is caused by their use of medications that cause dry mouth.19,22 Dry mouth may also be caused by chronic diseases such as diabetes, Alzheimer’s disease, and Parkinson’s disease.24,26,27
Cancer chemotherapy or head and neck cancer radiotherapy. These cancer treatments can cause many oral complications, including damage to salivary gland tissue, disfunction, and reduced salivary flow.19,28 In severe cases, this damage results in total loss of salivary output.28 Generally, chemotherapy causes acute toxicity, which resolves following discontinuation of therapy and healing of damaged tissue. On the other hand, radiation therapy can cause acute oral toxicity, as well as induce permanent tissue damage that puts patients at lifelong risk of dry mouth.19,29 Chemotherapy/radiotherapy can also cause an infection of the salivary glands, or sialadenitis.30 The use of radioactive iodine to treat some thyroid cancers can damage salivary glands (primarily the parotid glands).31 Dry mouth may also occur following hematopoietic stem-cell transplantation.32

Sjögren syndrome. This is a chronic, systemic autoimmune disorder that involves the salivary and lacrimal glands.33 Sjögren syndrome causes chronic inflammation and dysfunction of salivary tissue, resulting in salivary gland damage.33 It affects mostly middle-aged and older adults, 80% to 90% of whom are women. The principal oral symptom of Sjögren syndrome is dry mouth.22
Other conditions. Poorly controlled diabetes, sarcoidosis, hormonal changes (eg, pregnancy or menopause), salivary gland agenesis or aplasia, uncontrolled hypertension, hepatitis C virus infection, graft-vs-host disease, cystic fibrosis, human immunodeficiency virus/acquired immunodeficiency syndrome, lymphoma, nerve damage from a head or neck injury, surgical removal of salivary gland, psychogenic disorders, stroke, smoking, impaired fluid intake, vomiting, diarrhea, decreased mastication, and mouth breathing can all cause dry mouth.7
TREATMENTS DESIGNED TO ALLEVIATE DRY MOUTH/XEROSTOMIA SYMPTOMS
The first line of defense in the treatment of dry mouth is patient education on lifestyle modifications. Patients should be encouraged to sip water throughout the day, suck on ice chips, use lip lubricants every few hours, and suck on sugar-free candy or chew sugar-gree gum.7 Individuals with xerostomia should be advised to avoid caffeine, alcohol, tobacco, sugar-containing foods, salty or spicy foods, and dry, difficult-to-chew foods.7,13 The use of a humidifier at night to add moisture to the air may also be helpful.13 Patients with xerostomia should be advised to seek professional oral health care at more frequent intervals due to their increased risk for dental caries and periodontal diseases.15,18
Secretagogues, such as pilocarpine and cevimeline, may help stimulate salivary function.13,34,35 However, the use of pilocarpine has some significant side effects, including increased heart rate, high blood pressure, sweating, cutaneous vasodilation, nausea, vomiting, diarrhea, increased urinary frequency, bronchoconstriction, and vision problems.13 Both pilocarpine and cevimeline are contraindicated in patients with narrow-angle glaucoma.22 For patients experiencing dry mouth due to cancer chemotherapy or head and neck cancer radiotherapy, the prescription medication amifostine has been shown to help prevent damage of the salivary glands.36,37 Amifostine is administered intravenously 15 minutes to 30 minutes prior to radiation therapy.36
 Dry mouth treatment usually includes the use of artificial saliva to increase patient comfort. Adding toothpastes, gels, and mouthrinses with a neutral pH and those containing carboxymethylcellulose to a patient’s oral hygiene regimen may also help mitigate symptoms. Toothpastes and mouthrinses with plant-based ingredients, such as coconut oil, can also help soothe dry mouth symptoms.39 Caries prevention is key among those with xerostomia, and prescription-strength fluoride dentifrices and mouthrinses should be recommended, in addition to the use of professionally applied fluoride.38 Recommending sugarless candy and sugar-free gum with xylitol may also help reduce caries risk. Modalities containing arginine bicarbonate and calcium carbonate may also help patients with xerostomia maintain a neutral pH in the oral cavity and support healthy enamel.40 Products with amorphous calcium phosphate (ACP), casein phosphopeptide-ACP (Recaldent®), calcium sodium phosphosilicate (NovaMin®), and tricalcium phosphate may also support remineralization and reduce caries risk.39 Incorporating a chlorhexidine mouthrinse in to the oral hygiene routine can help minimize dental plaque accumulation.22
Dry mouth treatment usually includes the use of artificial saliva to increase patient comfort. Adding toothpastes, gels, and mouthrinses with a neutral pH and those containing carboxymethylcellulose to a patient’s oral hygiene regimen may also help mitigate symptoms. Toothpastes and mouthrinses with plant-based ingredients, such as coconut oil, can also help soothe dry mouth symptoms.39 Caries prevention is key among those with xerostomia, and prescription-strength fluoride dentifrices and mouthrinses should be recommended, in addition to the use of professionally applied fluoride.38 Recommending sugarless candy and sugar-free gum with xylitol may also help reduce caries risk. Modalities containing arginine bicarbonate and calcium carbonate may also help patients with xerostomia maintain a neutral pH in the oral cavity and support healthy enamel.40 Products with amorphous calcium phosphate (ACP), casein phosphopeptide-ACP (Recaldent®), calcium sodium phosphosilicate (NovaMin®), and tricalcium phosphate may also support remineralization and reduce caries risk.39 Incorporating a chlorhexidine mouthrinse in to the oral hygiene routine can help minimize dental plaque accumulation.22
![]() SUMMARY
SUMMARY
Identifying the underlying possible cause(s), relieving discomfort, and preventing complications are the main goals of treating patients with dry mouth/xerostomia. More frequent dental visits should be considered because those with xerostomia are at increased risk for dental caries and periodontal infections.15,18 Increased incidence of dental caries is anticipated, especially root and cervical caries. As such, yearly bitewing radiograph exposure is highly recommended. Plaque accumulation, gingivitis, and/or periodontitis are common, so oral hygiene measures should be reinforced at every dental visit.19 Oral health professionals should be well versed in the lifestyle modifications and products available to help relieve the symptoms of dry mouth.
REFERENCES
- Nadig SD, Ashwathappa DT, Manjunath M, Krishna S, Annaji AG, Shivaprakash PK. A relationship between salivary flow rates and candida counts in patients with xerostomia. J Oral Maxillofac Pathol. 2017;21:316.
- de Paula F, Teshima THN, Hsieh R, Souza MM, Nico MMS, Lourenco SV. Overview of human salivary glands: Highlights of morphology and developing processes. Anat Rec. 2017;300:1180–1188.
- Lima DP, Diniz DG, Moimaz SA, Sumida DH, Okamoto AC. Saliva: reflection of the body. Int J Infect Dis. 2010;14:e184–188.
- Hemadi AS, Huang R, Zhou Y, Zou J. Salivary proteins and microbiota as biomarkers for early childhood caries risk assessment. Int J Oral Sci. 2017;9:e1.
- Dawes C, Pedersen AM, Villa A, et al. The functions of human saliva: A review sponsored by the world workshop on oral medicine VI. Arch Oral Biol. 2015;60:863–874.
- Sultan Z, Haq Choudary J, Khan R, Mirza M, Zafar MS, Najeeb S. Human Saliva and its Role in Oral & Systemic Health. Journal of Pakistan Dental Association. 2017(25):170–174.
- Plemons JM, Al-Hashimi I, Marek CL, American Dental Association Council on Scientific Affairs. Managing xerostomia and salivary gland hypofunction: Executive summary of a report from the american dental association council on scientific affairs. J Am Dent Assoc. 2014;145:867–873.
- Riley P, Glenny AM, Hua F, Worthington HV. Pharmacological interventions for preventing dry mouth and salivary gland dysfunction following radiotherapy. Cochrane Database Syst Rev. 2017;7: CD012744..
- Sukumaran A, Sajith V, Mohamed H, Preethanath RS, Shankargouda P, Samaranayake LP. Xerostomia in geriatric patients: A burgeoning global concern. J Invest Clin Dent. 2016;7:5–12.
- Baer AN, Walitt B. Sjögren syndrome and other causes of sicca in the older adult. Clin
- Bakke M, Larsen SL, Lautrup C, Karlsborg M. Orofacial function and oral health in patients with Parkinson’s disease. Eur J Oral Sci. 2011;119:27–32.Geriatr Med. 2017;33:87–103.
- Guggenheimer J, Moore PA. Xerostomia: Etiology, recognition and treatment. J Am Dent Assoc. 2003;134:61–69.
- Villa A, Connell CL, Abati S. Diagnosis and management of xerostomia and hyposalivation. Ther Clin Risk Manag. 2015;11:45–51.
- Saleh J, Figueiredo MA, Cherubini K, Salum FG. Salivary hypofunction: An update on aetiology, diagnosis and therapeutics. Arch Oral Biol. 2015;60:242–255.
- Hayes M, Da Mata C, Cole M, McKenna G, Burke F, Allen PF. Risk indicators associated with root caries in independently living older adults. J Dent. 2016;51:8–14.
- Papas AS, Joshi A, MacDonald SL, Maravelis-Splagounias L, Pretara-Spanedda P, Curro FA. Caries prevalence in xerostomic individuals. J Can Dent Assoc. 1993;59:171–179.
- Delgado AJ, Olafsson VG. Acidic oral moisturizers with pH below 6.7 may be harmful to teeth depending on formulation: A short report. Clin Cosmet Investig Dent. 2017;9:81–83.
- Ouanounou A. Xerostomia in the geriatric patient: causes, oral manifestations, and treatment. Compend Contin Educ Dent. 2016;37:306–312.
- Turner MD, Ship JA. Dry mouth and its effects on the oral health of elderly people. J Am Dent Assoc. 2007;138:S15–S20.
- Sreebny LM, Vissink A. Dry Mouth: The Malevolent Symptom: A Clinical Guide. Ames, Iowa: Wiley-Blackwell; 2010:245.
- Sreebny Leo M. Saliva in health and disease: an appraisal and update. Int Dent J. 2011;50:140–161.
- Neville BW, Damm DD, Allen CM, Chi AC. Oral and Maxillofacial Pathology. 4th ed. St. Louis: Elsevier; 2016:912.
- Shetty SR, Bhowmick S, Castelino R, Babu S. Drug induced xerostomia in elderly individuals: an institutional study. Contemp Clin Dent. 2012;3:173–175.
- Yellowitz JA, Schneiderman MT. Elder’s oral health crisis. J Evid Based Dent Pract. 2014;14(Suppl):191–200.
- Daly C. Oral and dental effects of antidepressants. Aust Prescr. 2016;39:84.
- Stein P, Aalboe J. Dental care in the frail older adult: Special considerations and recommendations. J Calif Dent Assoc. 2015;43:363–368.
- Jablonski RY, Barber MW. Restorative dentistry for the older patient cohort. Br Dent J. 2015;218:337–342.
- Sroussi HY, Epstein JB, Bensadoun R, et al. Common oral complications of head and neck cancer radiation therapy: Mucositis, infections, saliva change, fibrosis, sensory dysfunctions, dental caries, periodontal disease, and osteoradionecrosis. Cancer Med. 2017;6:2918–31.
- Chaveli-López B. Oral toxicity produced by chemotherapy: A systematic review. J Clin Exp Dent. 2014;6:e81–e90.
- Epstein JB, Thariat J, Bensadoun RJ, et al. Oral complications of cancer and cancer therapy. CA Cancer J Clin.2012;62:400–422.
- Klein Hesselink EN, Brouwers AH, de Jong JR, et al. Effects of radioiodine treatment on salivary gland function in patients with differentiated thyroid carcinoma: A prospective study. J Nucl Med. 2016;57:1685–1691.
- Majhail NS. Long-term complications after hematopoietic cell transplantation. Hematol Oncol Stem Cell Ther. 2017;10:220–227.
- Zero DT, Brennan MT, Daniels TE, et al. Clinical practice guidelines for oral management of sjogren disease: Dental caries prevention. J Am Dent Assoc. 2016;147:295–305.
- Miranda-Rius J, Brunet-Llobet L, Lahor-Soler E, Farré M. Salivary secretory disorders, inducing drugs, and clinical management. Int J Med Sci. 2015;12:811–824.
- Villa A, Connell CL, Abati S. Diagnosis and management of xerostomia and hyposalivation. Ther Clin Risk Manag.2014;11:45–51.
- Gu J, Zhu S, Li X, Wu H, Li Y, Hua F. Effect of amifostine in head and neck cancer patients treated with radiotherapy: A systematic review and meta-analysis based on randomized controlled trials. PLoS One. 2014;9:e95968.
- Varghese JJ, Schmale IL, Mickelsen D, et al. Localized delivery of amifostine enhances salivary gland radioprotection. J Dent Res. 2018:22034518767408.
- Baysan A, Lynch E, Ellwood R, Davies R, Petersson L, Borsboom P. Reversal of primary root caries using dentifrices containing 5,000 and 1,100 ppm fluoride. Caries Res. 2001;35:41–46.
- Trushkowsky R. Xerostomia management. Dimensions of Dental Hygiene. 2014;12(3):3–39.
- Cantore R, Petrou I, Lavender S, et al. In situ clinical effects of new dentifrices containing 1.5% arginine and fluoride on enamel de- and remineralization and plaque metabolism. J Clin Dent. 2013;24(Spec No A):A32–A44.
From Dimensions of Dental Hygiene. July 2018;16(7):25-30.


 SUMMARY
SUMMARY

[…] H. Treating dry mouth. Dimensions of Dental Hygiene. July […]