 PRUDKOV/ ISTOCK/GETTY IMAGES PLUS
PRUDKOV/ ISTOCK/GETTY IMAGES PLUS
Tobacco Trends
While tobacco use continues to decline in adults, its prevalence is growing among young people, emphasizing the need for effective prevention and intervention strategies.
This course was published in the February 2017 issue and expires February 2020. The author has no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Explain the various alternative tobacco products and prevalence of use.
- Describe the health effects of tobacco use.
- Discuss the “5 A’s” of tobacco cessation and the approach to addressing these with patients.
- Summarize resources available to assist with tobacco intervention.
Cigarettes are the most commonly used form of tobacco use in adults.3 The prevalence of tobacco use among adults and youth in the US is measured by national surveys, which revealed 17% of adults, 9% of high school students, and 2% of middle school students were current cigarette smokers, defined as smoking >1 cigarette per day in the past 30 days.3,4 This is misleading, however, because young people tend to favor ATPs.3.4 The overall prevalence for tobacco use in general was approximately 7% of middle school students, 25% of high school students, and 21% of adults.5
ATPs include smoked and smokeless items, such as cigars, snus, dissolvables, e-cigarettes, water pipes/hookahs, chewing tobacco, to name a few.6,7 Electronic nicotine delivery systems (ENDS) heat liquid containing nicotine to an aerosol that is inhaled.8ENDS include vaporizers, vape pens, hookah pens, e-pipes, and e-cigarettes. According to the US Surgeon General, these delivery systems can also be used for cannabinoids and other drugs.9,10
The increase in the use of ENDS by youth is more rapid than in adults, with national surveys showing 1% to 5% of adults using ENDS compared to 14% to 16% of high school students.4,5,11 From 2011 to 2015, the use of ENDS among high school students increased from 1.5% to 16%. In middle school students, the reported use increased from < 1% to more than 5% between 2011 and 2015.5 Even more alarming is that approximately 10% of high school and 8% of middle school students reported daily use of ENDS.4 Of those using e-cigarettes, 63% reported using flavored ENDS products, suggesting this enhances their appeal to adolescents.4,9 ENDS usage is also associated with the utilization of other tobacco products among youth and young adults.9,11
The Tobacco Products and Risk Perceptions Survey found that 1% of adults who had never smoked reported using ENDS in the past 30 days, with almost 5% of those who had never smoked using these products at some point.12 It is concerning that people who identify as nonsmokers are using ENDS, suggesting a widespread belief they are less harmful than other tobacco products.9 The survey also found nearly 21% of current smokers reported using ENDS.12 Systematic reviews of ENDS to reduce the harmful health effects of cigarette smoking and aid in decreasing smoking frequency suggest ENDS may be helpful in tobacco cessation.13,14However, the long-term safety and health effects of ENDS use are unknown. Additionally, the evidence about the ability of ENDS to reduce smoking is of low quality.13,14 Oral health professionals need to monitor emerging information on this topic and beware of e-cigarette vendors wanting to advertise their products in the dental office.
Hookah tobacco is known by a number of names, including water pipe tobacco, maassel, shisha, narghile, and argileh. A water pipe (hookah) is used to smoke it.15 The water pipe is made of a head, body, bowl, and a hose containing a mouthpiece. The hookah tends to be used socially at parties, cafes, and lounges.16 Flavor enhancers may also be added, and almost 79% of youth who used a hookah reported choosing it because of the flavors available.17 Hookah use has been a part of Middle Eastern culture for centuries, but has only recently become popular among young adults and youth in the US.16 Many users believe water pipe smoking is less harmful than cigarettes, but evidence suggests the health outcomes and addiction issues are similar.18 Water pipe smoking sessions tend to last 30 minutes to 90 minutes. A systematic review and meta-analysis found one session of water pipe smoking resulted in 74.1 liters of smoke inhalation vs 0.6 liters for smoking a single cigarette.19 Higher levels of carbon monoxide, nicotine, and tar are also released during a session of water pipe smoking.
The prevalence of water pipe use among adults is approximately 4%.3 Conversely, the use of hookahs in youth is higher—about 7% of high school students, increasing from 4% in 2011.5 In middle school students, hookah use prevalence increased from 1% in 2011 to 2% in 2015.5
Smokeless tobacco products include chewing tobacco (also known as spit tobacco), dry snuff, and moist snuff or snus. The tobacco in these products may be loose leaf, powdered, or in pouches. These products contain high-intensity sweeteners, such as sucralose, in higher concentrations than is found in candy and soda.20 Sweeteners mask the unpleasant taste of tobacco and make it more appealing, especially to youth.20 In 2014, 59% of youth who used smokeless tobacco reported choosing a flavored variety.21
About 2.5% of adults reported using smokeless tobacco products.3 However, 6% of high school students and almost 2% of middle school students reported using smokeless tobacco.5 The percentage of youth using smokeless tobacco decreased about 1% from 2011 to 2015.5 Despite this decrease, frequent use (> 20 days in the last 30 days) of smokeless tobacco was most prevalent among high school students (42%) and middle school students (29.2%).4
Dissolvable tobacco products come in strips (placed on the tongue to dissolve), sticks (similar to large toothpicks), and lozenges or orbs (like a breath mint or candy).22 The nicotine content varies, but they can contain as much or more than a typical cigarette. Data on the prevalence of dissolvable tobacco use are not available because it is typically combined with smokeless tobacco in national surveys.
Cigars, little cigars, and cigarillos, as well as tobacco wrapped in a tobacco leaf are additional forms of tobacco use.23 One cigar contains as much tobacco as a pack of cigarettes.23 The little cigars and cigarillos may be flavored to enhance appeal, especially to youth and young adults. Adolescents reported using cigars because they liked the flavors (73.8%) and were more affordable (58.2%).17 Approximately 9% of high school students and 5% of adults reported using cigars in the past 30 days.5
HEALTH EFFECTS
In addition to the well-known negative health effects of tobacco use, nicotine exposure significantly harms the developing adolescent brain.9 The fact that the use of ATPs among youth is increasing emphasizes the need for effective prevention and cessation programs.
Like traditional cigarette smoking, water pipe smoking harms cardiovascular and respiratory health by increasing blood pressure, decreasing immunity, and raising the risk for chronic obstructive pulmonary disease.18,24 A systematic literature review found five studies that evaluated the association between periodontal diseases and water pipe smoking.24 Of these studies, four were with the same participants, limiting the sample size. This led Waziry et al24 to suggest that it is unclear whether an association exists between water pipe smoking and periodontal diseases. The health effects of heated and aerosolized components of e-cigarette liquids (eg, nicotine, solvents, flavoring, toxicants, etc) are unknown at this time.9
Another emerging tobacco trend is polytobacco use, or the use of more than one type of tobacco product. This is a growing trend among those who use ATPs and is associated with increased risk of nicotine addiction.25,26 This addiction leads to more problems with tobacco dependence and can hinder the success of tobacco cessation.25,26 The long-term health effects of polytobacco use warrant further research.
PREVENTION AND CESSATION
Tobacco prevention and cessation programs have been focused on smoking, leaving few resources to address ATPs. According to the US Preventive Services Task Force’s (USPSTF) guidelines for children and adolescents, efforts should focus on assessing risk, interventions to prevent tobacco use, and tobacco cessation.27 Risk assessment should include exposure to parental smoking, access to tobacco products, peers who use tobacco, and exposure to tobacco advertising.27
Oral health professionals can provide preventive messages related to both oral and general health. Messages need to be meaningful for youth in order to make a difference. Highlighting the short-term effects of tobacco use, such as staining of teeth and breath malodor or shortness of breath, which may impact endurance during athletic events, may be more effective for young tobacco users. According to the USPSTF, there is limited evidence related to the most effective approach to tobacco cessation in youth, and there are no pharmaceutical agents approved for this age group.27
The most current USPSTF guidelines for adults continue to recommend the “5 A’s” framework for tobacco intervention: asking about tobacco use; advising tobacco users to quit; assessing readiness to quit; assisting with quit attempt; and arranging follow-up.28 A modified version focused on ask, advise, and refer has also been proposed for oral health professionals, but research suggests patients are more successful in quit attempts when using the “5 A’s” approach.29
Screening patients for tobacco use, including ATPs, may be more challenging than for more traditional cigarette or smokeless tobacco use, because these products are not normally included on the medical history. As individuals who report never using tobacco may in fact use ENDS, there is a need to approach gathering this information more comprehensively.

Ask. The health history should list the actual types of ATPs to prompt questions by the oral health professional about the various types of tobacco products and frequency of use. Table 1 provides a sample of the information needed for tobacco use assessment.
Advise. Oral health professionals must advise patients to quit tobacco use to support oral and overall health. Patients should be educated on quitting in clear language that is personalized for each individual’s need at every appointment.30 Expect ambivalence (conflicted feelings about tobacco use) and listen nonjudgmentally to the patient’s concerns about tobacco cessation.
Assess. Oral health professionals need to assess patients’ readiness to quit tobacco use. This readiness to change behavior is a component of the Transtheoretical Model of Behavior Change, which is foundational for motivational interviewing and is widely used to help people quit smoking.31 In motivational interviewing, oral health professionals act as guides to assist patients in choosing to change behavior and support self-efficacy. An in-depth discussion of motivational interviewing is beyond the scope of this article, but many credible resources related to the topic are available.
Patients may be in various stages of quitting, including precontemplation (not interested in quitting), contemplation (thinking about quitting), preparation (planning to quit in next 30 days), action (quitting successfully for up to 6 months), and maintenance (quitting successfully for more than 6 months). The stage of readiness to quit should also be recorded in the patient record.
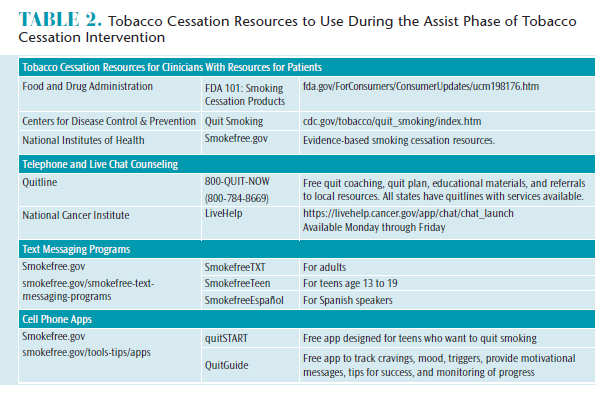
Assist. Table 2 provides a sampling of tobacco resources available to clinicians and patients. The resources for clinicians provide information on behavioral and pharmacologic approaches to assist patients in tobacco cessation. If the office or clinic has a website, links can be provided for tobacco cessation resources. An electronic record template may include a prompt to record the resources provided to patients so monitoring may occur over time. Ideally, collaboration by an interprofessional team to assist patients in successfully quitting tobacco is the preferred approach given the time constraints and expertise of the dental team. The interprofessional team may include the patient’s physician, nurse practitioner, physician assistant, pharmacist, and/or substance abuse counselor, as well as others. Oral health professionals need to remember that even individuals who smoke only one cigarette per day still have a 64% higher risk of early death, primarily from lung cancer, than never smokers.32
Arrange. Oral health professionals need to follow up with patients 1 week after a planned quit date and at each recare appointment to re-assess or provide support for another quit attempt or relapse prevention.30 In 2006, approximately 44% of adults reported a quit attempt in the past year, yet 95% to 98% resumed tobacco use without formal treatment. This underscores the need for oral health professionals to be actively involved in relapse prevention.33
Relapse prevention involves patients learning strategies to avoid or recover from lapses or relapses. Avoiding blame and guilt for a relapse is essential because negative emotions reduce the chances of success.33 Patients should be encouraged to examine the relapse to identify the trigger(s) and find approaches to avoid or overcome those trigger(s).33
REFERENCES
- US Department of Health & Human Services. The Health Consequences of Smoking: 50 Years of Progress. A Report of the Surgeon General. Available at: surgeongeneral.gov/library/reports/50-years-of-progress. Accessed January 24, 2017.
- Amrock SM, Weitzman M. Alternative tobacco products as a second front in the war on tobacco. JAMA. 2015;314:1507–1508.
- Hu SS, Neff L, Agaku IT, et al. Tobacco product use among adults—United States, 2013-2014. MMWR Morb Mortal Wkly Rep. 2016;65:685–691.
- Neff LJ, Arrazola RA, Caraballo RS, et al. Frequency of tobacco use among middle and high school students–United States, 2014. MMWR Morb Mortal Wkly Rep. 2015;64:1061–1065.
- Singh T, Arrazola RA, Corey CG, et al. Tobacco use among middle and high school students–United States, 2011-2015. MMWR Morb Mortal Wkly Rep. 2016;65:361–367.
- Lauterstein D, Hoshino R, Gordon T, Watkins BX, Weitzman M, Zelikoff J. The changing face of tobacco use among United States youth. Curr Drug Abuse Rev. 2014;7:29–43.
- McMillen R, Maduka J, Winickoff J. Use of emerging tobacco products in the United States. J Environ Public Health.2012;2012:989474.
- Food & Drug Administration. Vaporizers, E-Cigarettes, and other Electronic Nicotine Delivery Systems (ENDS). 2016. Available at: fda.gov/ TobaccoProducts/Labeling/ProductsIngredientsComponents/ucm456610.htm. Accessed Accessed January 24, 2017.
- US Department of Health & Human Services. E-cigarette Use Among Youth and Young Adults: A Report of the Surgeon General—Executive Summary. Atlanta; 2016.
- Morean ME, Kong G, Camenga DR, Cavallo DA, Krishnan-Sarin S. High school students’ use of electronic cigarettes to vaporize cannabis. Pediatrics. 2015;136:611–616.
- Gilreath TD, Leventhal A, Barrington-Trimis JL, et al. Patterns of alternative tobacco product use: Emergence of hookah and e-cigarettes as preferred products amongst youth. J Adolesc Health. 2016;58:181–185.
- Weaver SR, Majeed BA, Pechacek TF, Nyman AL, Gregory KR, Eriksen MP. Use of electronic nicotine delivery systems and other tobacco products among USA adults, 2014: Results from a national survey. Int J Public Health. 2016;61:177–188.
- Hartmann-Boyce J, McRobbie H, Bullen C, Begh R, Stead LF, Hajek P. Electronic cigarettes for smoking cessation. Cochrane Database Syst Rev. 2016;9:CD010216.
- Glasser AM, Collins L, Pearson JL, et al. Overview of electronic nicotine delivery systems: A systematic review. Am J Prev Med. 2016;52:e33–e66.
- United States Food and Drug Administration. Hookah tobacco (Shisha or Waterpipe Tobacco). Available at: fda.gov/TobaccoProducts/Labeling/ ProductsIngredientsComponents/ucm482575.htm. Accessed January 24, 2017.
- Maziak W, Taleb ZB, Bahelah R, et al. The global epidemiology of waterpipe smoking. Tob Control. 2015;24(Suppl 1):i3-i12.
- Ambrose BK, Day HR, Rostron B, et al. Flavored tobacco product use among US youth aged 12-17 Years, 2013-2014. JAMA. 2015;314:1871–1873.
- Haddad L, Kelly DL, Weglicki LS, Barnett TE, Ferrell AV, Ghadban R. A systematic review of effects of waterpipe smoking on cardiovascular and respiratory health outcomes. Tob Use Insights. 2016;9:13–28.
- Primack BA, Carroll MV, Weiss PM, et al. Systematic review and meta-analysis of inhaled toxicants from waterpipe and cigarette smoking. Public Health Rep. 2016;131:76–85.
- Miao S, Beach ES, Sommer TJ, Zimmerman JB, Jordt SE. High-intensity sweeteners in alternative tobacco products. Nicotine Tob Res. 2016;18:2169–2173.
- Corey CG, Ambrose BK, Apelberg BJ, King BA. Flavored tobacco product use among middle and high school students—United States, 2014. MMWR Morb Mortal Wkly Rep. 2015;64:1066–1070.
- United States Food and Drug Administration. Tobacco Products: Dissolvable tobacco products. Available at: fda.gov/TobaccoProducts/Labeling/ ProductsIngredientsComponents/ucm482569.htm. Accessed January 24, 2017.
- United States Food and Drug Administration. Tobacco Products: Cigars, cigarillos, little filtered cigars. Available at: fda.gov/TobaccoProducts/ Labeling/ProductsIngredientsComponents/ucm482562.htm Accessed January 24, 2017.
- Waziry R, Jawad M, Ballout RA, Al Akel M, Akl EA. The effects of waterpipe tobacco smoking on health outcomes: an updated systematic review and meta-analysis. Int J Epidemiol. 2016. Epub ahead of print.
- Sung HY, Wang Y, Yao T, Lightwood J, Max W. Polytobacco use of cigarettes, cigars, chewing tobacco, and snuff among US adults. Nicotine Tob Res. 2016;18:817–826.
- Butler KM, Ickes MJ, Rayens MK, Wiggins AT, Hahn EJ. Polytobacco use among college students. Nicotine Tob Res. 2016;18:163–169.
- Moyer VA, US Preventive Services Task Force. Primary care interventions to prevent tobacco use in children and adolescents: US Preventive Services Task Force recommendation statement. Ann Intern Med. 2013;159:552–557.
- Siu AL, US Preventive Services Task Force. Behavioral and pharmacotherapy interventions for tobacco smoking cessation in adults, including pregnant women: US Preventive Services Task Force Recommendation Statement. Ann Intern Med. 2015;163:622–634.
- Gordon JS, Andrews JA, Crews KM, Payne TJ, Severson HH. The 5A’s vs 3A’s plus proactive quitline referral in private practice dental offices: preliminary results. Tob Control. 2007;16:285–288.
- Black JH 3rd. Evidence base and strategies for successful smoking cessation. J Vasc Surg. 2010;51:1529–1537.
- Lindson-Hawley N, Thompson TP, Begh R. Motivational interviewing for smoking cessation. Cochrane Database Syst Rev.2015:Cd006936.
- Inoue-Choi M, Liao LM, Reyes-Guzman C, Hartge P, Caporaso N, Freedman ND. Association of long-term, low-intensity smoking with all-cause and cause-specific mortality in the National Institutes of Health-AARP Diet and Health Study. JAMA Intern Med. 2017;177:87–95.
- Collins SE, Witkiewitz K, Kirouac M, Marlatt GA. Preventing relapse following smoking cessation. Curr Cardiovasc Risk Rep. 2010;4:421–428.
From Dimensions of Dental Hygiene. February 2017;15(2):50-53.



