TIPPING THE SCALES TOWARD CARIES CONTROL
Dental hygienists play an important role in caries control, from assessment to treatment compliance.
.jpg)
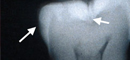
Figure 1. Bitewing radiograph and histological view of hemisection of the same tooth. The radiograph shows a lesion in the enamel on the proximal surface (arrowed) that extends just into the dentin when viewed histologically. This would not be restored as it does not radiographically extend past the dentino-enamel junction. The lesion is remineralizable. In contrast there is a faint shadow (arrow) under the occlusal surface on the radiograph, but the lesion extends to the pulp and will require restoration.
The dental hygienist needs to be actively involved in caries risk assessment and should work closely in conjunction with the dentist to deliver caries management under the umbrella of minimally invasive dentistry. A structured caries risk assessment should be carried out based on the concept of the caries balance. After the risk assessment is complete, a treatment plan is devised that leads to the control of dental caries for the patient.
The dental hygienist and the dentist, as a team, can more effectively perform caries risk assessment and manage dental caries for individuals and in community settings with the knowledge that we now have of the caries process. The caries balance concept must be embraced by dental hygienists in order to deliver caries prevention and intervention effectively in modern dental practice.1-3
Pathological factors, including 1) cariogenic bacteria, 2) frequent ingestion of fermentable carbohydrates, and 3) salivary dysfunction, drive the caries process toward demineralization. Protective factors such as, 1) salivary components, 2) fluoride and remineralization, and 3) antibacterial therapy, drive the caries process toward remineralization. Effective caries management revolves around these principles. In the case of high caries risk, people with bacterial infection must be dealt with at the same time that remineralization is enhanced. All this must be done in conjunction with restorative dentistry, if needed, using minimally invasive techniques in order to preserve as much of the existing sound tooth structure as possible.
CONSERVATIVE CARIES MANAGEMENT
The goal of conservative caries management is to preserve as much of the existing tooth structure as possible by controlling the bacterial infection, thus swinging the caries balance toward remineralization and the prevention of future cavities.
First, carious lesions should be detected early enough so that their formation, prior to cavitation, can be reversed or arrested rather than restored. Second, the individual caries risk of the patient should be assessed by examination, questionnaire, and biological testing. Third, a treatment plan that involves enhancement of remineralization, reduction of the bacterial challenge, and monitoring of the patient’s progress should be put in place. Fourth, existing cavities should be restored by filling with appropriate materials while conserving tooth structure.1,3
These principles enhance the natural repair mechanism—provided by saliva—by addressing the bacteria challenge, chemically reversing or arresting caries, and by providing the patient with a better chance of healthy teeth in the future. Every dental hygienist is familiar with the current methods of caries detection that primarily include visual, tactile (with an explorer), and radiographic assessment. These methods have been in use for many years and are successful and useful up to a point.
In the case of proximal lesions, the radiograph as currently used is adequate and successful. The current guiding principle used to decide on restoration is: if the radiographic lesion in these surfaces does not extend beyond the dentino-enamel junction (DEJ) then restoration is not required and remineralization is possible. However, for occlusal surfaces this basic principle does not hold. Visual inspection of occlusal surfaces can indicate by discoloration that subsurface decay may be present. Obvious cavitation is easy to detect with the visual/tactile combination. However as illustrated in Figure 1, it is possible to have major decay in the dentin underneath an enamel surface where only a faint radiographic shadow is observed. Figure 1 shows a proximal lesion in the conventional bitewing radiograph, which extends slightly into the dentin as illustrated by the histological section. However, the radiograph does not show this beyond the DEJ and the lesion is remineralizable.
In the case of the lesion under the occlusal surface, this extends right to the pulp and does need physical intervention and removal. The surrounding sound enamel has reduced the x-ray beam so that only the faint shadow is shown just beyond the DEJ. Obviously with this conventional methodology, early lesions in occlusal enamel will not be detected. This means that early intervention in occlusal surfaces by antibacterial therapy and remineralization require better detection methods.
CARIES DETECTION DEVICES
One device is currently on the market in the United States—the DIAGNOdent™ (KaVo America Corp, Lake Zurich, Ill), which uses a red laser light through a fiber optic and specially-designed hand piece to shine into the subsurface of the tooth. If there is caries present and if specific bacterial byproducts have soaked into the porous area, then the red light will interact with these bacterial byproducts and fluoresce in the infrared region, which is picked up by the detector, giving a number between 0 to 99. Numbers over about 25 indicate the probability of a subsurface lesion, and physical intervention with a small bur can decide whether to proceed and open up for restoration.4
The DIFOTI (Electro-Optical Sciences Inc, Irvington, NY) is another caries detection device that is currently available. It uses a digital charged couple device camera to capture the visually observed images that identify carious lesions and then sends them to a computer for analysis. Clinical research is still being done on its efficacy.5 One limitation of this system is that it cannot indicate whether a lesion has reached the dentin. OMNII Oral Pharmaceuticals,
West Palm Beach, Fla, is introducing another new device—the QLF (quantitative light fluorescence). This device uses a light source of selected wavelength to improve the visibility of noncavitated lesions and will be introduced to the market this year.5
The key point is that early detection is integral to future conservative caries management and the hygienist can play a key role along with the dentist in more effective caries detection.
CARIES RISK ASSESSMENT
Numerous attempts have been made to come up with effective and proven methods of caries risk assessment. However, with the science now available, following a simple set of guidelines for effective caries risk assessment as part of caries management is possible.1-3,6 The April 2002 California Dental Association meeting in Sacramento, Calif, produced caries risk assessment procedures and two simple 1-page forms that can be used in dental practice. One form is for children 0 through 5 years of age and the second form is for children 6 years and older as well as adults.6 These forms are listed with the web version of this article at www.dimensionsofdentalhygiene.com.
The following steps are recommended for caries risk assessment of patients aged 6 years through adulthood. The more risk factors involved, the higher the caries risk. The more protective factors identified, the lower the caries risk. At the end of the assessment, which can be done in a few minutes by a practiced dental health professional, an overall assessment of high, medium, or low caries risk is made and used as the basis for tipping the caries balance toward no caries and for developing the subsequent treatment plan for the patient. The procedures for children 0 through 5 years of age are similar but reference should be made to the special risk assessment form for that age group.6
HIGH RISK FACTORS
These factors are indicators of high caries risk with more factors cumulatively indicating a higher risk.
- Visible caries cavitation or caries into the dentin by radiograph. In this case it is very likely that the patient has high levels of mutans streptococci and/or lactobacilli and a bacterial test is immediately indicated to provide a baseline for measuring the success of antibacterial treatments.
- Caries restored in the past 3 years. If the patient has had recent caries restored, this is also a good indicator that new caries will occur in the immediate future.
- Readily visible heavy plaque on the teeth. This indicates poor oral hygiene and/or prolific plaque growth and is an indirect indicator that high levels of cariogenic bacteria are likely.
- Frequent between meal snacks of sugars or fermentable carbohydrates. If the patient is snacking more than three times daily between meals on foods or beverages that contain sucrose, glucose, fructose, or cooked starch (cookies or bread), this increases the acid challenge to the teeth to high.
- Saliva reducing factors. If a patient is taking hyposalivatory medications, such as tranquilizers or mood altering medications, saliva flow is reduced. Patients taking multiple medications are at increased risk. If a patient has cancer in the head and neck region and is receiving radiation treatment, this may also severely impair salivary function. Saliva flow rate can be measured by having the patient chew and spit into a measuring cup and calculating the number of milliliters (ml) per minute. A value less than 0.7 ml/minute is low, whereas 1 ml to 4 ml per minute is normal.
- Presence of fixed or removable appliances in the mouth such as orthodontic brackets or removable partial dentures leads to undue accumulation of plaque and an increase in the percent of cariogenic bacteria.
MODERATE RISK FACTORS
Moderate risk factors for caries include:
- Exposed tooth roots. This is a prerequisite for the formation of root caries.
- Deep pits and fissures or developmental defects. These provide extra retentive areas for cariogenic plaque to thrive.
- Interproximal white spot lesions, as determined by radiographs, indicate past caries or potentially new early carious lesions. The overall risk assessment needs to be carried out to determine whether these lesions may be arrested or if they are progressive.
- Discoloration of occlusal surfaces may indicate ongoing subsurface caries.
PROTECTIVE FACTORS
These factors are what keep the majority of the population from caries initiation or progression for the majority of the time.
- The patient lives, works, or goes to school in a fluoridated community. Fluoridation of the drinking water helps provide fluoride to the mouth for children and adults, which in turn, helps swing the caries balance toward no caries or reduced caries.
- Daily use of fluoride toothpaste is a major caries reducing factor and is a recommendation that should be made for all patients.
- Fluoride mouth rinse or gel. If the patient uses a fluoride mouth rinse (0.05 % sodium fluoride) or gel (5,000 ppm F) daily, this is additional protection beyond the use of fluoride toothpaste.
- Adequate saliva flow. This can be measured as described above or it may be obvious that saliva flow is adequate. Adequate saliva flow provides all of the multiple protections of the salivary components as described elsewhere.3
- Xylitol-containing gum or mints. Recent research has shown that daily use of xylitol-containing chewing gum or mints can maintain lower levels of cariogenic bacteria in the mouth and also inhibit transfer of bacteria from one individual to another.7,8
- Mother or caregiver has no caries activity. In the case of children, the most likely transfer of bacteria comes from the mother or caregiver9 and if that person has no caries activity and has low levels of cariogenic bacteria then this is considered a protective factor.
OVERALL ASSESSMENT
If the answer is yes for visible cavitation, then a bacterial test should be performed. It is possible to conduct a simple bacterial test in the dental office and kits are currently available through Vivadent, Amherst, NY, (Caries Risk Test) and Edge Dental, Traverse City, Mich, (Dentocult Test Strips). The test is done by having the patient chew on a gum-like substance and spitting into a cup for 3 to 5 minutes. The saliva flow is measured to determine whether it is low or normal and the whole mixed saliva produced by the patient is now applied to the bacterial test strips of selective media and incubated for approximately 72 hours (72 hours gives a better result than the 48 hour minimum recommended by the manufacturers). Incubators are available for use in the dental office and the bacterial test strips are easily read against a standard chart to determine whether the levels are high, medium, or low. These tests can be recorded in the patient’s chart and used as a motivational tool. New tests should be taken after 6 months of antibacterial therapy to determine the efficacy of the therapy and the compliance of the patient.
RECOMMENDED THERAPY
Once the risk assessment has been conducted, decisions can then be made as to what therapy will be recommended. The following are provided as guidelines:
• Daily Oral Hygiene
All patients, regardless of risk level, should be recommended to brush twice daily with an effective fluoride toothpaste/dentifrice. Not only will this reduce the plaque level in the mouth, most importantly, it will provide therapeutic levels of fluoride to the mouth on a regular basis. Fluoride is retained in the mouth for several hours subsequent to brushing and application twice daily is an effective therapeutic measure.10
• Additional Fluoride
For moderate and high risk patients, additional fluoride should be recommended depending on the likelihood of compliance. An over-the-counter fluoride rinse containing 0.05% sodium fluoride is very effective if used twice daily in addition to a fluoride toothpaste.11 For high risk patients, a brush-on gel or dentifrice with a high concentration of fluoride content, such as 5,000 ppm, should be prescribed. There are also fluoride lozenges available, which can be sucked by adults to provide therapeutic levels of fluoride in the mouth that enhance remineralization. This is especially useful for xerostomic patients.
• Chewing Gum
The use of chewing gum can be recommended for high risk patients, especially those with low saliva flow. The use of chewing gum will stimulate the saliva and, thereby, enhance remineralization. Chewing gum or mints that do not contain fermentable carbohydrates (sugarless) should be recommended. Some contain xylitol, which also has antibacterial effects. Xylitol-containing gums are becoming available now in supermarkets and they can be purchased through dental supply companies.
• Antibacterial Rinse
In the case of high risk patients who have medium to high levels of either mutans streptococci or lactobacilli or both, they should be placed on an antibacterial rinse. Currently the most effective antibacterial rinse is chlorhexidine gluconate 0.12%.12 Recommended use is as a once daily rinse with 10 ml for 1 minute at bedtime for 1 week. This should be repeated for 1 week every month for up to 6 months and then as further bacterial testing is done. Staining is possible with these products, but if used only 1 week per month, staining should be a minimal issue. Compliance is also a problem with this product, which is why we recommend 1 week at a time and repeating monthly rather than 2 weeks every 3 months. New antibacterials are expected to become available in the near future.
•Sealants
Sealants should be considered for patients at high risk for caries, regardless of age. A risk assessment of individual teeth must be performed to determine if sealants are an appropriate treatment option. Teeth with enamel caries, those that may have decay, and those at risk for decay should all be considered for sealants. There are a variety of material options when using sealants. Resin, composite-based sealants come in several categories—unfilled, filled, and flowable composites. Fluoride-releasing glass ionomer sealants are also available and are particularly effective when a partially or newly erupted molar is hard to isolate.
CARIES MANAGEMENT OF HIGH RISK SUBJECTS
In simple terms, we need to reduce the bacterial challenge for high risk patients by using antibacterial rinses and increase the protective factors by using multiple fluoride therapy and saliva enhancement. Reducing the frequency of fermentable carbohydrate consumption must also be incorporated into the plan.
The following example of a high caries risk subject is not an actual case, but illustrates the above principles. A 20-year-old college student presents with the first cavity of his life and numerous interproximal radiographic lesions, some extending into the dentin. Bacterial testing reveals high counts of mutans streptococci and lactobacilli, saliva flow rate is normal, and the patient admits to frequent snacking and irregular meals because of his studying habits. He also admits to infrequent use of fluoride toothpaste and tooth brushing. Chlorhexidine is used to reduce his bacterial levels, as measured by the selective media testing. His cavity is restored; he is recommended to use fluoride toothpaste twice daily and is prescribed a 5,000 ppm high concentration fluoride toothpaste for daily use when he is not using his chlorhexidine rinse. He fills out a brief diet diary and, with dietary counseling, successfully substitutes xylitol chewing gum for his in-between meal cariogenic snacks. Within 6 months his bacteria are under control, remineralization is occurring, and he is on the road to dental health for the future. He reverts to the use of a regular over-the-counter fluoride toothpaste and adds a twice daily over-the-counter fluoride mouth rinse to maintain his caries-free situation.
The dental hygienist is the professional who first meets the patient, conducts caries risk assessment with the dentist, educates the patient, and follows-up to help with compliance, which can make a dramatic difference in tipping the balance toward caries control and future dental health.
References
- Featherstone JDB. The caries balance: contributing factors and early detection. J Calif Dental Assoc. 2003;31:129-133.
- Featherstone JDB. The caries balance. Dimensions of Dental Hygiene. 2004;2(2):14-18.
- Featherstone JDB. The science and practice of caries prevention. J Amer Dental Assoc. 2000;131:887-899.
- Lussi A, Megert B, Longbottom C, Reich E, Francescut P. Clinical performance of a laser fluorescence device for detection of occlusal caries lesions. Eur J Oral Sci. 2001;109:14-19.
- Stookey GK. The evolution of caries detection. Dimensions of Dental Hygiene. 2003;1(6):12-15.
- Featherstone JDB, Adair SM, Anderson MH, et al. Caries management by risk assessment: consensus statement, April 2002. J Calif Dental Assoc. 2003;31:257-269.
- Hildebrandt GH, Sparks BS. Maintaining mutans streptococci suppression with xylitol chewing gum. J Amer Dental Assoc. 2000;131:909-916.
- Isokangas P, Soderling E. Occurrence of dental decay in children after maternal consumption of xylitol chewing gum, a follow up from 0 to 5 years of age. J Dent Res. 2000;79:1885-1889.
- Berkowitz RJ. Acquisition and transmission of mutans streptococci. J Calif Dental Assoc. 2003;31:135-137.
- Zero DT, Raubertas RF, Pedersen AM, Fu J, Hayes AL, Featherstone JDB. Fluoride concentrations in plaque, whole saliva and ductal saliva after applications of home-use fluoride agents. J Dent Res. 1992;71:1768-1775.
- O’Reilly MM, Featherstone JDB. De- and remineralization around orthodontic appliances: an in vivo study. Am J Orthod. 1987;92:33-40.
- Anderson MH. Chlorhexidine: how useful is it in combatting the bacterial challenge and dental caries? J Calif Dental Assoc. 2003;31:211-216.
From Dimensions of Dental Hygiene. March 2004;2(3):20, 22, 24, 26-27.

