 IKONOSMEDIA / ISTOCK / GETTY IMAGES PLUS
IKONOSMEDIA / ISTOCK / GETTY IMAGES PLUS
The Role of the Dental Hygienist in External Root Resorption
Enabling patients to choose the best treatment option for them is important when addressing this oral condition.
Detection and assessment are important aspects of dental hygiene therapy.1 The preliminary examination can point the therapist toward the unique needs of each patient. Dental hygienists are trained to be observant—examining soft and hard tissues of the oral cavity to detect deviations from “normal” or “healthy” tissues. Detection of abnormal findings can alter the planned course of treatment. This article provides a case study that focuses on the discovery of root resorption and the role played by the dental hygienist.
The Dental Hygiene Standard of Care states that the beginning of an appointment should start with a patient assessment, which includes a patient interview.2 The interview is used to determine if the patient has a chief complaint or any perceived changes since his or her last dental visit. The information provided by the patient can initiate the assessment of a selected area of the oral cavity by the dental hygienist. A thorough examination is still essential because early dental problems may be symptom free and clinically undetectable.3,4

Case Study
A 90-year-old woman returns to the dental office for her 4-month recare visit. The patient is a retired judge in favorable general health, and is not currently taking any medications. The patient presents with no oral pain or concerns; however, she has a history of performing subpar oral hygiene. She does not practice routine flossing and presents with marginal biofilm at each appointment. An initial oral examination and full-mouth probing were performed by the dental hygienist. At the time of the visit, the buccal aspect of the lower right first premolar presented with an increase in pocket depth—from 2 mm to 6 mm. A dark purple discoloration of the soft tissue was also noted in this area (Figure 1,).
A full-mouth radiographic survey had been taken 15 months prior to this appointment. At that time, the radiographs had been evaluated by the dentist and no disease had been noted (Figure 2). Upon exploration with an ODU 11/12 explorer, a subgingival concavity in the root structure was detected approximately 4 mm below the cementoenamel junction and extending to the base of the pocket area. The dentinal surface of the root was hard, but the concave area was soft when gently explored with the ODU 11/12. Reflecting the tissue gently with a Marquis probe reveled an irregular defect in the root surface (Figure 3). The patient did not experience any pain when the subgingival defect was explored or probed.

When a concerning finding is made during the assessment stage of an appointment, the dental hygienist needs to form a dental hygiene diagnosis.2 This step involves data collection and consultation with the supervising dentist to discuss a comprehensive care plan for the patient.2 A new radiograph of the area may be necessary to complete the data collection process.
Understanding the problem is key to formulating the correct treatment plan. Careful attention to the location of abnormal findings, their clinical and radiographic appearance, and the presence of any etiologic agents can make accurate detection, diagnosis, and management possible. Detailed scaling of the root defect may not be the appropriate treatment for this tooth. Without a diagnosis, the tooth may be damaged by the incorrect treatment. Determination of a diagnosis and subsequent sequenced treatment plan is of paramount importance.

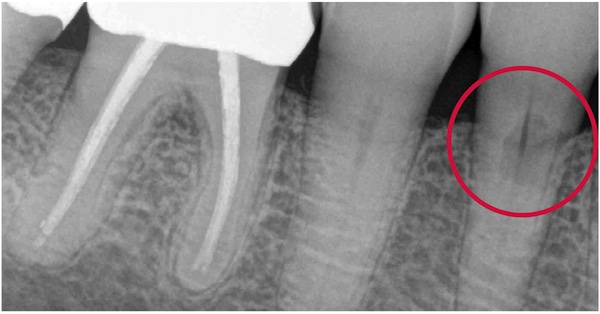
In this case, the dentist determined that a new periapical radiograph should be taken of the concerning area. A comparison of the past radiograph to the new radiograph showed a significant change to the root structure of the lower right first premolar. The new radiograph showed a large radiolucency in the root surface, with no apparent change in the nerve canal (Figure 4). These findings, combined with the clinical examination, revealed that the tooth presented with possible root resorption.
The next step was to determine which type of resorption was present on the root surface. Clinicians must understand how to differentiate between internal and external root resorption. Internal root resorption is its own unique entity, whereas external resorption can display many forms.5,6 Internal root resorption starts within the root canal space or pulp chamber, and the cells of origin are the pre-dentin lining of the pulpal area.5,6 Radiographs will show a radiolucency that involves the pulpal area of the tooth. Internal root resorption may focus on the coronal aspect of the tooth, causing bleeding into the crown. This can turn the crown a pink or purple color, otherwise known as “pink tooth.”7,8
External Root Resorption
There are multiple forms of external root resorption. Each presents with its own unique signs and symptoms. However, the pathogenesis is linked to the loss or damage of the periodontal ligament, activating cementoblasts.9,10 External root resorption is a pathological process, which tends to occur following a wide range of mechanical or chemical stimuli such as infection, pressure, trauma, or orthodontic tooth movement. External root resorption is usually detected radiographically, however, some cases may be identified by clinical symptoms such as pain or swelling.11

External inflammatory root resorption (EIRR) tends to arise from endodontic pathology triggered by the loss of cementum.5,12 Apical EIRR is found at the apex of the tooth and can present with subclinical symptoms in cases of current or past orthodontic therapy or total pulp necrosis.5 Pressure resorption is a noninflammatory form of external resorption that may occur as secondary damage of the periodontal ligament due to orthodontic movement or the eruption of a misaligned tooth.5
External cervical resorption (ECR) is the final category of resorption.5 ECR typically starts at the cervical area of the tooth, but it may be found just above the epithelial attachment.7,10 Inflammation of the junctional epithelium of the periodontal attachment can predispose the patient to this type of resorptive process.7 Possible etiologies include a history of orthodontics, trauma, periodontal therapy, or internal bleaching with caustic agents. However, it often presents idiopathically.13,14 ECR is the form of resorption most often seen in clinical dental practice.5

The patient in the case study was interviewed to confirm that no known trauma had occurred to the tooth in question and that she had no dental pain. In addition, the patient had not undergone any recent endodontic, orthodontic, or periodontal procedures, so the dentist determined the diagnosis was likely idiopathic ECR. Treatment options vary depending on the extent of the ECR to the root structure. If the tooth is restorable, then the lesion can be managed with a surgical procedure, followed by restoration of the defect.13,15 If there is pulpal involvement, then endodontic treatment is indicated.5,6 These treatment options were discussed with the patient.

The dental hygienist serves a critical role in patient education as well as addressing any questions the patient may have concerning each treatment option, so that a mutually agreed upon treatment plan can be established.1 The patient did receive a full-mouth periodontal scaling at this appointment; however, the buccal of the lower right first premolar was not instrumented.
Treatment Options
The dental hygienist presented the following treatment options:
- Do nothing and continue to observe the tooth knowing that this may lead to future tooth pain and, ultimately, tooth loss.
- Extract tooth and do no additional therapy.
- Extract the tooth and replace with a bridge or implant.
- Save the tooth with endodontic treatment followed by periodontal surgery to allow access for restoration of the root surface.
The dental hygienist, when discussing the treatment options that the dentist had suggested, was aware that the patient was 90 years old and may make a decision based on her life expectancy. The patient may consider the most cost-effective treatment plan or the less stressful option. However, the patient made the decision to maintain the tooth at all costs. She did not want to lose a tooth at this point in her life.

Following are detailed photos of each stage of treatment. Since the resorption was close to the pulpal canal of the tooth, endodontic therapy was performed as a first step (Figure 5). The next procedure included periodontal surgery to expose the root defect. A periodontal flap was laid and the root surface was debrided and treated with an application of trichloroacetic acid (Figure 6 and Figure 7). The root was filled and the surgical area closed and allowed to heal (Figure 8 and Figure 9).

The patient was placed on a 3-month recare program and was followed for 8 years. Over that time, the lower right first premolar functioned well and was infection free. Slight inflammation was present in the area of the restoration with a 5-mm residual pocket (Figure 10). The patient continued to perform a suboptimal level of self-care. The patient is now 98 years old and she still has the tooth.

Conclusion
Looking for the unexpected is part of the dental hygiene oral assessment. Keeping up to date about rare oral conditions can help the clinician to detect early disease and enable teeth to be saved. Educating patients about their oral condition and allowing them to choose the treatment option that is best for them should always be part of the dental visit. In addition, patients need to understand that ongoing care is critical for the success of any treatment option.
Supporting Clinician Health in Addition to Patient Health
Dental hygienists are charged with supporting their patients’ oral health as well as their overall health. With this responsibility, it is easy for clinicians to neglect their own well-being.
Scaling and root planing, which requires repetitive movements and awkward positioning, can lead to career-ending musculoskeletal injuries. Dental hygienists should strive to improve the ergonomics of their practice to prevent such injuries.
The most significant step to improving ergonomics during instrumentation is magnification. Loupes enable dental hygienists to maintain proper posture while eliminating the struggle to view the oral cavity. A variety of different styles and magnification levels are available. Dental hygienists should spend time with representatives of loupe manufacturers to determine which type best suits their needs.
Implementing ergonomic strategies into the process of instrumentation is also helpful. Instruments with wide diameters and textured grips may alleviate pain derived from the instrumentation process. Also, ensuring instruments are sharp is an ergonomic plus, as this eases the amount of pressure the clinician must apply.
Prioritizing self-care is paramount to health. Taking breaks to stretch and switch positions is supportive of ergonomic health. Also, a healthy diet, exercise regimen, and mental health support can all help dental hygienists maintain a long career in dental hygiene.
For more information on how to support ergonomic health, visit: dimensionsofdentalhygiene.com/category/articles/ergonomics.
References
- American Dental Hygienists’ Association. Professional Roles of the Dental Hygienist: Available at: adha.org/resources-docs/빀_DHiCW_Roles_Dental_Hygienist.pdf. Accessed May 18, 2022.
- American Dental Hygienists’ Association. Standards for Clinical Dental Hygiene Practice. Available at: adha.org/resources-docs/떐-Revised-Standards-for-Clinical-Dental-Hygiene-Practice.pdf. Accessed May 18, 2022.
- Mayo Clinic. Periodontitis—Symptoms and Causes. Available at: mayoclinic.org/diseases-conditions/periodontitis/symptoms-causes/syc-20354473. Accessed May 18, 2022.
- Mayo Clinic. Cavities/Tooth Decay—Symptoms and Causes. Available at: mayoclinic.org/diseases-conditions/cavities/symptoms-causes/syc-20352892. Accessed May 18, 2022.
- Blicher B. Differentiating resorption. Available at: aae.org/specialty/communique/differentiating-resorption. Accessed May 18, 2022.
- Tronstad L. Root resorption—etiology, terminology and clinical manifestations. Endo Dent Trauma. 1988;4:241–252.
- Warnsinck CJ, Shemesh H. [External cervical root resorption]. Ned Tijdschr Tandheelkd. 2018;125:109–115.
- Battista P. Clinical manifestations of internal resorption. Decisions in Dentistry. 2016;2(6):24–27.
- Barbosa dos Santos J, Castillo J, Nishiyama C, Esper L, Pinto L, Pinheiro C. External root resorption: diagnosis and treatment—clinical case report. Journal of Dental Health, Oral Disorders and Therapy. 2018;9(2).
- Chen Y, Huang Y, Deng X. External cervical resorption—review of the pathogenesis and potential predisposing factors. International Journal of Oral Science. 2021;13(19).
- Ahangari Z, Nasser M, Mahdian M, Fedorowicz Z, Marchesan MA. Interventions for the management of external root resorption. Cochrane Database Syst Rev. Interventions for the management of external root resorption. Cochrane Database Syst Rev. 2015;2015:11.
- Abbott PV. Prevention and management of external inflammatory resorption following trauma to teeth. Aust Dent J. 2016;61(Suppl 1):82–94.
- Patel S, Foschi F, Condon R, Pimentel T, Bhuva B. External cervical resorption: part 2 —management. Int Endo J. 2018;51:1224–1238.
- Heithersay GS. Invasive cervical resorption: an analysis of potential predisposingfactors. Quintessence Int. 1999;30:83–95.
- Heithersay GS. Treatment of invasive cervical resorption: an analysis of results using topical application of trichloroacetic acid, curettage, and restoration. Quintessence Int. 1999;30:96–110.
From Dimensions of Dental Hygiene. June 2022; 20(6)14,16,18,21.

