 KOSAMTU/ISTOCK/GETTY IMAGES PLUS
KOSAMTU/ISTOCK/GETTY IMAGES PLUS

Despite advances in preventive oral care, dental caries remains the most common chronic disease among American children.1 Once a child experiences caries, he or she is likely to experience additional caries, demonstrating that past caries experience is a predictor of future caries development. Moreover, children with caries in their primary teeth are more likely to experience caries in their permanent teeth.2,3 Data from the National Health and Nutrition Examination Survey 2011 to 2014 show approximately 18% of children in the United States ages 6 to 11 had treated or untreated caries in their permanent teeth.4 Prevention of caries formation in children is critical to ensure the preservation of the permanent dentition. The survey also revealed more than half of adolescents ages 12 to 19 (58%) had decay in their permanent teeth. Approximately 90% of adults have had at least one caries lesion and one in four adults currently has untreated tooth decay.5
Dental sealants are one of the most effective means for preventing occlusal caries. According to the US Centers for Disease Control and Prevention (CDC), dental sealants prevent 80% of caries over 2 years and continue to protect against 50% of caries for up to 4 years.5 School-aged children without dental sealants placed on their first molars are also three times more likely to develop caries on these teeth than children with sealants.5
Currently, resin-based sealants are the most commonly used; however, placement typically generates aerosol spray. This is because, with most but not all resin-based sealants, acid etch must be applied and then thoroughly rinsed off prior to applying the resin material. Glass ionomer sealants are also effective in preventing caries and their placement technique does not generate airborne pathogens because phosphoric acid etch is not used. Over the past year, the onset of COVID-19 has greatly impacted the way dental care is provided and oral health professionals are charged with reducing viral transmission risk in the dental office.

PREVENTING CARIES WITH DENTAL SEALANTS
Dental sealants provide a physical barrier over the pits and fissures of posterior teeth to prevent bacterial colonization and acid challenges from cariogenic bacteria.6,7 Molar and premolar teeth are particularly vulnerable to caries as deep pits and fissures provide reservoirs for bacteria to colonize, making them the ideal teeth to evaluate for sealants. As a primary prevention strategy, sealants are part of a comprehensive caries management approach to prevent lesions by sealing grooves or pit and fissures on occlusal surfaces of permanent molars and premolars. As a secondary prevention measure, sealants impede the progression of noncavitated lesions.7,8
Despite the known benefits of dental sealants, they remain underutilized. Between 2011 and 2014, only 48% of US children ages 6 to 11 had dental sealants.4 Children of lower socioeconomic status are less likely to have sealants compared to children from higher income families.8 More emphasis needs to be placed on the importance of sealants in an effort to increase their utilization.
When determining whether a patient is a candidate for dental sealants, several factors are considered, including which sealant material is best for the individual patient. The two most common types of sealant materials used today are resin-based sealants and glass ionomer-based sealants.
RESIN-BASED SEALANTS
Resin-based sealants consist of composite materials that are either light-cured or self-cured (chemical-cured). Resin-based sealant material is flowable and does not require mixing. However, resin-based materials that are hydrophobic depend on a dry field.9 This is often difficult to achieve, especially when working on a small, moving child. Additionally, to achieve an adequate microbond, many resin-based sealants require etching, rinsing, and thoroughly drying the tooth, which necessitates an aerosol-generating procedure for placement.10 Research has shown that resin-based dental sealants have better retention than glass ionomer sealants.11,12

GLASS IONOMER SEALANTS
Glass ionomer sealants consist of a polymeric water-soluble acid, silicate glass, and water.9,13 The material fuses directly to tooth structure, therefore no etching is required. Glass ionomer sealant materials are hydrophilic, meaning they can be applied in a wet field.9 Self-curing with a hardening time of approximately 2 minutes to 3 minutes, glass ionomer sealants do not require occlusal adjustment, as they wear down on their own. Furthermore, because glass ionomer sealants do not require the additional step of etching, they are quick to place. Also, glass ionomer sealant material does not contain bisphenol A-glycidyl methacrylate or bisphenol A (BPA).9 Although the BPA released from resin-based sealants is well below the limit of 1 million nanograms per day and does not pose any health risk, patients may still prefer to choose a dental sealant material without BPA.14
While resin-based sealants offer higher retention rates, both resin-based and glass ionomer sealants exhibit the same caries prevention effect.11,12 Research does show that the fluoride-releasing capability of glass ionomer sealants is higher than resin-based sealants.9 Glass ionomer sealants can be placed under the operculum of partially erupted molars when teeth are not fully in occlusion to aid in self-cleansing, and they chemically bond directly to enamel/dentin, preventing microleakage.15
PLACEMENT OF GLASS IONOMER SEALANTS
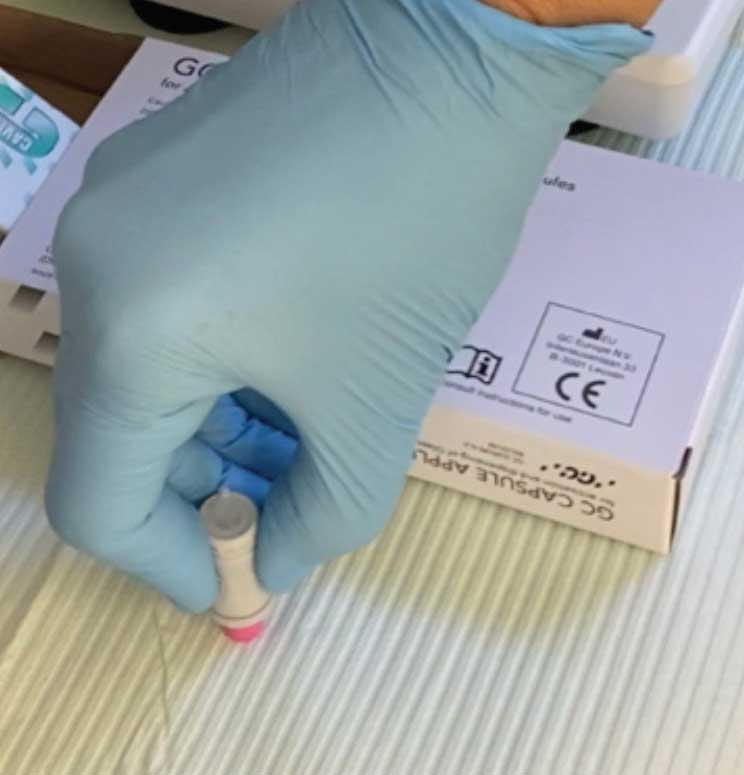
The placement of glass ionomer sealants is simple, and may be preferred during the global pandemic. After determining the tooth is eligible for sealant placement, it should be cleaned with pumice using either a toothbrush or a disposable prophy brush head (Figure 1).14 The pumice is then cleaned from the tooth using water-soaked cotton rolls. Next, isolate the tooth (isolation is not to create a dry surface, but rather to prevent the oral structures, such as the cheek or tongue, from impeding the process). Then, apply cavity conditioner with a microbrush (Figure 2).15 After 10 seconds, remove the cavity conditioner with a water-soaked cotton roll. The materials should then be activated by pressing the base (plunger end) of the glass ionomer capsule firmly on the counter (Figure 3). Place the capsule in the titrator for 10 seconds, remove, put the activated capsule in the applicator, and press trigger twice (break the diaphragm).15 Place a tiny amount of product onto the tooth (Figure 4) and with a wet, gloved finger, press the material into the grooves (Figure 5). Ask the patient to bite a few times, remove any excess, and rinse. The material hardens in approximately 2 minutes to 3 minutes.

CONCLUSION
With financial hardships, increased consumption of sugary foods, and disruptions in daily oral hygiene, preventing oral disease is a priority. Dental sealants can assist in the prevention of occlusal caries in children and adolescents at high caries risk. A review of the literature on the effectiveness of pit and fissure sealants in caries prevention shows that both sealant types offer significant benefits and the decision about which should be used is based on individual patient and practice factors.
REFERENCES
- Dye BA, Tan S, Smith V, et al. Trends in oral health status: United States, 1988-1994 and 1999-2004. Vital Health Stat 11. 2007;248:1–92.
- Du Q, Yu M, Li Y, et al. Permanent caries experience is associated with primary caries experience: a 7-year longitudinal study in China. Community Dent Oral Epidemiol. 2017;45:43–48.
- American Academy of Pediatric Dentistry. Policy on early childhood caries (ECC): unique challenges and treatment options. The Reference Manual of Pediatric Dentistry. Chicago: American Academy of Pediatric Dentistry; 2020:82–83.
- Dye BA, Mitnik GL, Iafolla TJ, Vargas CM. Trends in dental caries in children and adolescents according to poverty status in the United States from 1999 through 2004 and from 2011 through 2014J J Am Dent Assoc. 2017;148:550–565.
- United States Centers for Disease Control and Prevention. Dental Sealants. Available at: cdc.g/v/oralhealth/fast-facts/dental-sealants/index.html. Accessed May 11, 2021.
- Wright JT, Tampi MPP, Graham L, et al. Sealants for preventing and arresting pit-and-fissure occlusal caries in primary and permanent molars: a systematic review of randomized controlled trials-a report of the American Dental Association and the American Academy of Pediatric Dentistry. J Am Dent Assoc. 2016;147:631–645.
- Wright JT, Crall JJ, Fontana M, Graham L, Estrich C, Carrasco-Labra A. Evidence-based clinical practice guideline for the use of pit-and-fissure sealants: a report of the American Dental Association and the American Academy of Pediatric Dentistry. J Am Dent Assoc. 2016;47:672–682.
- Griffin SO, Wei L, Gooch BF, Weno K, Espinoza L. Vital signs: Dental sealant use and untreated tooth decay among U.S. school-aged children. MMWR Morb Mortal Wkly Rep. 2016;65:1141–1145.
- Beauchamp J, Caufield PW, Crall J, Kohn W, Siegal M, Simonsen R. Evidence-based clinical recommendations for the use of pit-and-fissure sealants: a report of the American Dental Association Council on Scientific Affairs. J Am Dent Assoc. 2008;139:257–267.
- Brian Z, Weintraub JA. Oral health and COVID-19: increasing the need for prevention and access. Preventing Chronic Disease. 2020;17:e82.
- Alirezaei M, Bagherian A, Shiraz SA. Glass ionomer cements as fissure sealing materials: yes or no?: A systematic review and meta-analysis. J Am Dent Assoc. 2018;149:640–649.
- Jaafar N, Ragab H, Abedrahman A, Osman E. Performance of fissure sealants on fully erupted permanent molars with incipient carious lesions: a glass-ionomer-based versus a resin-based sealant. J Dent Res Dent Clin Dent Prospects. 2020;14:61–67.
- Sidhu SK, Nicholson JW. A review of glass-ionomer cements for clinical dentistry. J Funct Biomater. 2016;7:16.
- Manchir M. Is BPA in dental sealants safe? Available at: ada.org/en/publications/ada-news/2016-archive/august/bpa-in-dental-sealants-safe. Accessed May 11, 2021.
- Goldstep F, Delios, C. Glass ionomer fissure sealants for proactive intervention. Available at: oralhealthgroup.com/features/glass-ionomer-fissure-sealants-for-proactive-intervention. Accessed May 11, 2021.
From Dimensions of Dental Hygiene. June 2021;19(6):16-18.

