ALEX-MIT/ISTOCK/GETTY IMAGES PLUS
ALEX-MIT/ISTOCK/GETTY IMAGES PLUS
The Process of Remineralization
Oral health professionals are well-positioned to make individualized clinical recommendations regarding diet, oral self-care, and product selection in order to encourage remineralization.
The process of remineralization remains crucial to preventing caries and arresting incipient lesions.1 As prevention specialists, dental hygienists are well-positioned to make clinical recommendations regarding diet, oral self-care, and product selection. Clinicians should use a caries management by risk assessment (CAMBRA) approach to determine best practices for treatment and at-home recommendations tailored to each patient’s needs. By conducting a caries risk assessment, the clinician can tailor his or her oral self-care instruction to meet the specific needs of each patient. Professional recommendations informed by specific patient risk factors may lead to early intervention of initial carious lesions and potentially prevent or minimize the need for surgical interventions.2
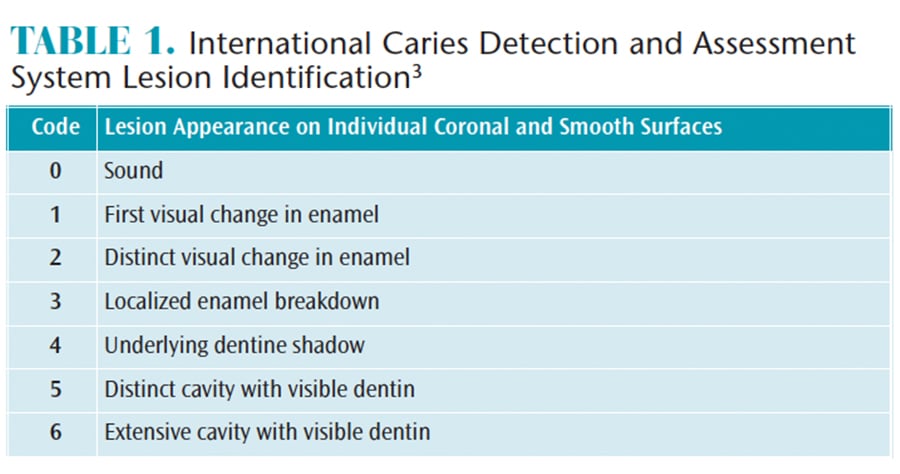
Historically, the surgical approach to treating caries was used extensively in dentistry. More recently, the International Caries Detection and Assessment System (ICDAS) was developed after an extensive systematic review of the literature.3 Following the ICDAS, clinicians score the stage and activity level of carious lesions (Table 1).3 In today’s practice, clinicians should refer to the ICDAS, which emphasizes minimally invasive dental practices for lesions in the initial stages in an effort to remineralize weakened tooth structure.3–6 Lesions that are characterized as moderate or extensive should still be treated operatively.3 This paradigm shift from the surgical approach to the nonsurgical approach emphasizes CAMBRA, and supports the concept of addressing the cause of caries and determining treatment options based on evidence-based literature.4–6
The nonsurgical approach is a less invasive way to manage caries and allows the clinician to focus on identifying the cause of disease through the assessment of risk factors. Once the risk factors for caries are identified, they can be modified via professional recommendations made for both in-office and at-home care for each patient.6 For existing carious lesions, the clinician critically evaluates and suggests best treatment options, including focusing on remineralization for initial stage lesions.3 An area of demineralized hydroxyapatite can be remineralized, and depending on the agents used to enhance remineralization, the tooth structure can become stronger and more caries resistant.4
PROCESS
An essential component to consider when addressing caries and discussing remineralization is pH.7 The scale of pH ranges from 0 to 14. The lower the pH reading, the more acidic the environment being measured. A neutral pH reading is considered to be 7. A low pH, or an acidic environment, leads to demineralization of the teeth. Enamel, the hardest substance in the body, begins to break down at a pH of 4.5 to 5.5.8 Cementum begins to break down in a pH environment of 6.0 to 6.7.8 A drop in the pH may be caused by carbohydrate consumption, acid-producing bacteria, and decreased salivary flow.1 When the pH is low or the environment is acidic, the risk for caries increases.7 By identifying low pH as a risk factor for caries, the clinician can use this information to educate the patient and make evidence-based recommendations for professional and at-home care.7 The pH of the oral environment should be assessed at each appointment to further understand the patient’s needs and facilitate more appropriate treatment and at-home recommendations.7
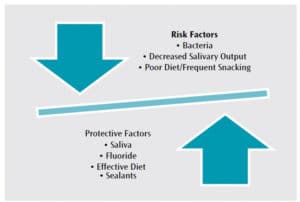
When the oral bacteria absorb sugars from the foods consumed, they produce acid, which dissolves calcium and phosphate in the enamel.9 When produced in smaller amounts and more infrequently, the acid can be neutralized by saliva, and the saliva replaces the lost minerals in the enamel. However, when the acid production is more frequent or in higher quantities, the saliva cannot keep up in neutralizing the acidity, and the tooth begins to demineralize.9 Therefore, when demineralization, or breakdown of the tooth structure, occurs faster than the remineralization process, the tooth is weakened. The imbalance between the two processes will eventually lead to a cavitated tooth structure. However, in the early stages of the caries lesion, remineralization is possible with the appropriate primary intervention and additional adjunctive therapies.1,10 This intervention consists of protective factors that can combat the risk factors (Figure 1). Understanding the acidity of the oral environment can explain clinical findings and assist the dental hygienist in tailoring oral self-care education and recommendations.
PREDISPOSING CONDITIONS
Individuals who are at risk for dental caries include those with cariogenic diets (including frequent carbohydrate consumption), xerostomia (decreased salivary flow), increased bacteria (especially mutans streptococci and lactobacilli), past caries experience, poor oral self-care, increased acidity due to acid reflux or bulimia, and root exposure.11 Educating patients on their caries risk is essential when explaining clinical findings and making recommendations. Recognizing the role that predisposing factors play in the caries process can alert and motivate patients to improve oral self-care and prevent future carious lesions.
Patients may experience xerostomia due to medication(s) or systemic conditions, such as Sjögren syndrome.10 In addition to aiding in masticatory processes, saliva is charged with combating demineralization. Saliva-derived components responsible for remineralization include proline-rich glycoproteins, statherins, calcium, phosphate, fluoride, and mucins.11 Salivary substitutes and stimulants may be recommended when salivary production is compromised. Salivary substitutes include gels, rinses, or liquids, while salivary stimulants include gums and lozenges.10 The use of self-care products containing carboxymethylcellulose or plant-based ingredients, such as coconut oil, as well as those with a neutral pH may help ameliorate dry mouth symptoms.12
TREATMENT RECOMMENDATIONS
Oral health professionals are positioned to critically assess clinical findings and determine the needs of each patient. Recommendations should include primary preventive strategies. Primary means of preventing decay remain unchanged. Recommendations for caries prevention and management include water fluoridation, dental sealants, diet modification, fluoride dentifrice and mouthrinse, and topical fluorides.1,4,13 Diet counseling should include a recommendation to decrease sugar consumption.6 Rinsing with water after eating and drinking may also be helpful. Diet counseling may include education on avoiding certain acidic foods and beverages. Even some bottled waters are considered more acidic and should be avoided.14
Adjunctive therapies that may be recommended include professional treatments and at-home prescriptive and over-the-counter regimens. Casein phosphopeptide-amorphous calcium phosphate (ACP) has shown similar remineralizing effects as fluoride, while 2% arginine added to neutral sodium fluoride (NaF) has shown to enhance remineralization.15,16 Prescription 1.1% NaF and calcium phosphate pastes have also been shown to decrease bacterial colonization and remineralize tooth structure.4,10
Silver diamine fluoride (SDF) both prevents and arrests dental caries.17 By promoting the formation of hydroxyapatite and fluorapatite, SDF strengthens the tooth.17 The silver in SDF also has antibacterial properties, making the lesion smaller and more resistant to acid attacks.17–19 Oral health products with ACP, casein phosphopeptide-ACP (Recaldent), calcium sodium phosphosilicate (NovaMin), and tricalcium phosphate may encourage remineralization.12
Nonfluoride adjunctive therapies exist, as well. A panel of experts established by the American Dental Association (ADA) Council on Scientific Affairs reviewed nonfluoride adjunctive therapies and noted that they are helpful as adjunctive therapies with the primary means of prevention being the first choice in caries prevention.20 Chlorhexidine has proven to be beneficial in the remineralization process, but patients should refrain from chlorhexidine rinses for 30 minutes after brushing.11,21 Calcium phosphate prescription rinse has been shown to decrease pH.10 Sugar alcohols—xylitol and sorbitol—are bacteriostatic and, when delivered in a gum or lozenge, can stimulate saliva.10,11 Chewing gums with calcium and phosphate may replenish calcium and phosphate lost during demineralization, and also assist in stimulating salivary production.10 Chewing gum should only be recommended to children age 5 and older who can chew adequately and do not experience dysfunction when chewing.11
CONCLUSION
Dental caries remains a concern for patients of all ages. Oral health professionals are charged with educating patients on caries prevention, risk factors, and treatment recommendations. Clinicians can refer to the ADA’s chairside guidelines for topical fluoride, sealants, fluoride toothpaste for young children, and nonfluoride caries preventive agents.22 These guidelines coupled with the clinician’s professional judgment and patient preference will serve as an evidence-based approach to using CAMBRA.
REFERENCES
- Abou Neel EA, Aljabo A, Strange A, et al. Demineralization-remineralization dynamics in teeth and bone. Int J Nanomedicine. 2016;11:4743–4763.
- Chaffee B, Cheng J, Featherstone JDB. Baseline caries risk assessment as a predictor of caries incidence. J Dent. 2015;43:518–524.
- Shivakumar KM, Prasad S, Chandu GN. International Caries Detection and Assessment System: a new paradign in detection of dental caries. J Conser Dent. 2009;12:10–16.
- Compton R. Opportunities to increase prevention in dentistry. J Dent Hyg. 2015;89(Suppl 1):30–32.
- Rayapudi J, Usha C. Knowledge, attitude and skills of dental practitioners of Puducherry on minimally invasive dentistry concepts: A questionnaire survey. J Conser Dent. 2018;21: 57–262.
- Young DA, Featherstone JD, Roth JR. Curing the silent epidemic: caries management in the 21st century and beyond. J Calif Dent Assoc. 2007;35:681–685.
- Kianoush N, Adler CJ, Nguyen KT, Browne GV, Simonian M, Hunter N. Bacterial profile of dentine caries and the impact of ph on bacterial population diversity. PLoS One. 2014;9:e92940.
- Wilkins EM. Clinical Practice of the Dental Hygienist. 12th ed. Philadelphia: Wolters Kluwer; 2017:270.
- Featherstone JD, Domejean-Orliaguet S, Jenson L, Wolff M, Young DA. Caries risk assessment in practice for age 6 through adult. J Calif Dent Assoc. 2007;35:701–713.
- Cartee D, Maker S, Dalonges D, Manski M. Sjögren’s syndrome: Oral manifestations and treatment, a dental perspective. J Dent Hyg. 2015;89:365–371.
- Garcia-Godoy F, Hicks MJ. Maintaining the integrity of the enamel surface: The role of dental biofilm, saliva and preventive agents in enamel demineralization and remineralization. J Am Dent Assoc. 2008;139:255–345.
- Trushkowsky R. Xerostomia management. Dimensions of Dental Hygiene. 2014;12(3):3–39.
- Wiener CR, Crout RJ, Wiener MA. Toothpaste used by children, oral hygiene, and nutritional education: An assessment of parental performance. J Dent Hyg. 2009;83:141–145.
- Wright KF. Is your drinking water acidic? A comparison of the carried pH of popular bottled waters. J Dent Hyg. 2015;(Suppl 2):6–12.
- Li J, Xie X, Wang Y, et al. Long-term remineralizing effect of casein phosphopeptide-amorphous calcium phosphate (CPP-ACP) on early caries lesions in vivo: A systematic review. J Dent. 2014;42:769–777.
- Bijle MNA, Ekambaram M, Lo EC, Yiu CKY. The combined enamel remineralization potential of arginine and fluoride toothpaste. J Dent. 2018;76:75–82.
- Bowen D. Effectiveness of professionally-applied silver diamine fluoride in arresting dental caries. J Dent Hyg. 2016;90: 75–78.
- Gao SS, Zhang S, Mei ML, Lo EC, Chu CH. Caries remineralization and arresting effect in children by professionally applied fluoride treatment—a systematic review. BMC Oral Health. 2016;16:1–9.
- Gao SS, Zhao IS, Hiraishi N, et al. Clinical trials of silver diamine fluoride in arresting caries among children: a systematic review. JDR Clinical and Translational Research. 2016;1(3):201–210.
- Rethman MP, Betran-Aguilar ED, Billings RJ, et al. Nonfluoride caries preventive agents. J Am Dental Assoc. 2011;142:1065–1071.
- Almohefer SA, Levon JA, Gregory RL, Eckert GJ, Lippert F. Caries lesion remineralization with fluoride toothpastes and chlorhexidine—effects of application timing and toothpaste surfactant. J Appl Oral Sci. 2018;26:e20170499.
- American Dental Association Center for Evidence-Based Dentistry. Clinical Practice Guidelines. Available at: ebd.ada.org/en/evidence/guidelines. Accessed September 28, 2018.
From Dimensions of Dental Hygiene. October 2018;16(10):50,52–54.