The Periodontal Probe
Periodontal evaluation is critical to the early diagnosis and effective management of periodontal diseases.
Gingival inflammation is a clear indicator of periodontitis. However, periodontal pockets and other symptoms of periodontal diseases can be present without the telltale signs of gingival inflammation. This makes periodontal probing, assessment of clinical attachment level, and measurement of the attached gingiva’s width absolutely essential to routine periodontal examinations.
|
|
Probing depth assessments are the basis of an effective periodontal evaluation. The results are used, along with an evalua tion of the patient’s medical and dental history, a review of evidence-based literature, and the clinician’s experience, to make therapeutic decisions.1 Dental hygienists are responsible for the completion and recording of comprehensive, accurate, and time-efficient periodontal assessments.2,3
Probing Designs
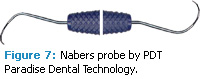
Manual periodontal probes are typically used during routine periodontal examinations.4 The design of the probe is important because it can affect the accuracy of the probing measurements. Factors to consider include diameter, force, gingival conditions (edema tous or fibrotic), angulation, pocket contour, root anatomy, and reading and/or recording of measurements. Single-ended or double ended periodontal probes are available (figures 1 and 2). The shank angle is usually straight, however, a right-angle design is available to enhance access to the posterior areas (Figure 3). Variances occur in the shank width, angle, and length; the working end and diameter; blunt-rounded (Figure 4), thin tapered (Figure 5), or ball-ended configura tions (Figure 6); and measurement indicators of 1 mm or more. Nabers probes are also part of the armamentarium for assessing furcations (Figure 7).
Technique
The straight periodontal probe is gently inserted into the sulcus/pocket to the epithelial attachment where light resilience should be felt. Radiographs should be used in conjunction with prob ing to ensure accuracy. Probing around calculus should be attempted. If the calculus impedes accurate measurement, probing can occur immediately after removal of heavier deposits and before final completion of the segment(s) planned for treatment.
The working end of a probe is adapted parallel to the root surface. The tip is placed at a 0º angle to the root surface and the remainder of the working end is angulated at approximately 10º to the root surface. Small walking motions of about 1 mm in height are used to negotiate the sulcus/pocket topography. This allows for assessment of not only the six recommended points but also the entire base of the sulcus/pocket. This walking motion allows the clinician to find the deepest portion of the facial, lingual, and line angle areas. It is important to evaluate the entire circumference of the sulcus/ pocket because the epithelial attachment is not even around the tooth.5
Insertion generally occurs mesial to the distal line angle on posterior teeth and near the midline for anteriors. The walking motions must overlap. Another option is to continue probing the anterior region by inserting at the distal line angle of the canine across the anterior sextant. The probe is rolled and pivoted at line angles to maintain the same angulation through out the procedure. On the proximal sur faces, the working end must remain against the contact area, and the probe must be extended to the midline of the proximal surface. Observing the occlusal surface to help estimate the location of the midline can facilitate proximal extension. The review of radiographs is also important in the proximal area to assess whether interdental craters are present.
Bleeding on probing, which is an indi cator of disease, is dependent on the force used by the operator. Daniel et al recommend pressing the probe into the finger pad of the thumb approximately 2 mm to estimate appropriate force.6 Because probing force will vary slightly from patient to patient, comfort should be assessed through communication with the patient. Pain control should be used when needed.
Dental hygienists working in the same practice setting can calibrate their probing by observing each other during probing, using the same type of probes, and compar-ing readings. This calibration will improve accuracy. Thorough and accurate technique and calibration help establish that changes in oral health are due to advancing disease and not differences in probing technique and the type of probe used.
Systematic Approach
The periodontal assessment should include a full mouth, six-point probing with every sulcus/pocket depth recorded for all adult patients. The six measurements include three on the facial surface (mesiofacial, facial, distofacial) and three on the lingual surface (mesiolingual, lingual, distofacial). When completing the periodontal assess ment, the clinician should develop a stan dardized sequence that is easy to apply. For example, begin with the facial of the maxillary right to maxillary left, then com plete the lingual area before moving to the mandibular arch.
No matter what systematic approach is used, it should be comfortable for the dental hygienist and followed during each patient assessment. Experienced clinicians should be able to complete a full mouth probing and recording in approximately 10 minutes. If the clinician has a dental assistant recording, the assessment time is likely reduced.
Application During Assessment
Probing depth measurements provide an overall assessment of the periodontal pocket depths, which is where periodon tal microorganisms thrive.4 Probing depth is the distance from the gingival margin to the epithelial attachment.4 After pocket depths are assessed, clinical attachments levels (CAL) are determined. CAL is the distance from the cementoe namel junction (CEJ) to the base of the sulcus/pocket. When the gingival margin is at the CEJ, the loss of attachment is equal to the probing depth. When the gingival margin is located apical to the CEJ (ie, recession), the loss of attachment is greater than the pocket depth, and distance between the CEJ and gingival margin should be added to the total probing depth.7 Table 1 provides a glossary of terms commonly used in periodontal assessment.
The periodontal probe is also used to assess attached gingiva. A probe meas ures the total width of the gingiva from the free gingival margin to the mucogin gival junction, and the pocket depth is subtracted from the total gingival width. Inadequate attached gingiva results when less than 1 mm of attached gin giva is present.8
Periodontal Maintenance
Serial probing measurements must be completed at periodontal maintenance appointments and compared with previous measurements to determine whether the disease is progressing.9 Rather than peri odontal pocket measurement, attachment loss over time is the primary indicator of the periodontal disease progression. Regular documen tation of attachment loss in the patient record is important to track periodontitis activity, progression, and severity.
Periodontal Probing Systems and Recording
The use of dental management systems and automated probing systems can fur ther enhance accuracy and efficiency of the periodontal probing assessment. Table 2 provides a list of automated prob ing systems. Pressure-sensitive, computer assisted, and voice – activated probing sys tems are alternatives to manual probing. Computer-generated periodontal charting systems capture visual images, which is helpful when educating patients about their disease status. The visual representation of their disease may improve patient motivation and commitment to oral health care practices.
Conclusion
Probe readings in increments of 1 mm provide the greatest accuracy, and in practices with more than one dental hygienist, the same types of probes should be used to ensure consistency of readings between clinicians. Dental hygienists can control some factors by selection of the proper probe and tech nique, however, the patient’s inherent conditions such as root anatomy and tissue tone cannot be controlled.
One of the most significant problems in the management of periodontal dis eases is the failure of some clinicians to monitor clinical outcomes and identify patients whose periodontitis is advancing. Comprehensive periodontal probing on a regular basis can increase the early diag nosis and subsequent management of periodontal diseases.
References
- Greenstein G. Current interpretations of periodontal probing evaluations: diagnostic and therapeutic implications. Compen Contin Educ Dent. 2005;26:381-382,384,387-390.
- American Dental Hygienists’ Association (ADHA). ADHA Bylaws and Code of Ethics. Available at: www.adha.org/aboutadha/index.html. Accessed August 27, 2010.
- ADHA. Standards for Clinical Dental Hygiene Practice. Available at:www.adha.org/downloads/adha_standards08.pdf. Accessed August 27, 2010.
- American Academy of Periodontology. Position paper: diagnosis of periodontal diseases. J Periodontol. 2003;74:1237-1247.
- Nield JS. Fundamentals of Periodontal Instrumentation and Advanced Root Instrumentation. 6th ed. Philadelphia: Lippincott Williams & Wilkins; 2008.
- Daniel SJ, Harfst SA, Wilder R. Mosby’s Dental Hygiene, Concepts, Cases, and Competencies. 2nd ed. St. Louis; Saunders Elsevier; 2008.
- Newman MG, Takei HH, Klokkevold PR. Carranza’s Clinical Periodontology. 10th ed. St. Louis: Saunders Elsevier; 2006.
- Darby ML, Walsh MM. Dental Hygiene Theory and Practice. 3rd ed. St. Louis: Saunders Elsevier; 2010.
- Jeffcoat MK. Current concepts in periodontal disease testing. J Am Dent Assoc. 1994;125: 1071-1078.
From Dimensions of Dental Hygiene. September 2010; 8(9): 50-52, 54.