The Oral Microbiome and the Risk of Lung Infection
Aspirating oral pathogens to the lower airway may cause serious health implications for vulnerable patients.
This course was published in the April 2015 issue and expires April 30, 2018. The author has no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Identify the different types of pneumonia.
- Discuss the role of oral health in the prevention and treatment of pneumonia.
- Define chronic obstructive pulmonary disease (COPD).
- Explain the association between COPD and oral health.
PNEUMONIA
Community-acquired pneumonia (CAP) is a significant cause of morbidity and mortality in individuals who have not recently been admitted to a hospital or other health care facility (eg, long-term care facility [LTCF]). CAP is often preceded by chronic viral or bacterial infections, which diminish the cough reflex, interrupt mucocilliary clearance, and enhance pathogenic bacterial adherence to respiratory mucosa.3
Viruses such as respiratory syncytial virus or rhinovirus are common etiologic agents of CAP. Bacterial causes of CAP include exposure to group B streptococci or Gram-negative enteric bacteria early in life. Streptococcus pneumoniae and Hemophilus influenzae are often the cause of CAP in adults (Figure 1).
About 4 million CAP cases occur in the United States each year.4 Many of these cases are successfully treated in the primary-care setting. Overall, CAP results in more than 600,000 hospitalizations, 64 million days of restricted activity, and 45,000 deaths annually.
Risk factors for CAP include advanced age, male gender, smoking, and the presence of chronic obstructive pulmonary disease (COPD), asthma, diabetes mellitus, and/or congestive heart failure.5 A recent large, population-based cohort study of 46,237 adults aged ?65 observed over a 3-year period6 found additional risk factors for CAP, including exposure to sudden changes of temperature at work, the use of inhalation therapy (particularly containing steroids) and oxygen therapy, and the presence of asthma and chronic bronchitis. Interestingly, these authors also identified a visit to a dentist in the past month as an independent protective factor for CAP, presumably due to subsequent improvements in oral hygiene.6
MONICA SCHROEDER/SCIENCE SOURCE
CAP is usually treated with antibiotics—including oral azithromycin, clarithromycin, erythromycin, or doxycycline—in otherwise healthy patients, or oral moxifloxacin, gemifloxacin, or levofloxacin in patients with other comorbidities. The emergence of community-acquired methicillin-resistant Staphylococcus aureus as a cause of CAP emphasizes the need to formulate novel strategies for pneumonia prevention to reduce the need for antibiotic use.7
Until recently, hospital-acquired (nosocomial) pneumonia (HAP) was defined as pneumonia occurring more than 48 hours after admission to a hospital. Over the past decade, however, there has been a shift in the delivery of medical services—such as antibiotic therapy, chemotherapy, wound management, dialysis, and short-term rehabilitation—from hospitals to outpatient settings. As a result, the classification scheme for pneumonia has changed. Pneumonia occurring in outpatient settings is referred to as health care-associated pneumonia.8 Nursing-home associated pneumonia affects LTCF residents, comprising 13% to 48% of all infections.9 Pneumonia also is a common reason for transfer of residents from LTCFs to hospitals.10
HAP is a common infection in hospital settings, often causing severe morbidity or mortality, as well as extending the length of stay and increasing the cost of care. HAP can be further divided into two subtypes: ventilator-associated pneumonia (VAP) and nonventilator-associated pneumonia. VAP is the most common infection in the intensive care unit (ICU).11 VAP is also the leading cause of death in the ICU, with estimated prevalence rates of 10% to 65%, and mortality rates of 25% to 60% depending on the study, patient populations, and medical/surgical conditions involved.11,12 VAP and other forms of HAP are independent risk factors for mortality in hospitalized patients regardless of the severity and type of underlying illness.13 An episode of HAP extends hospital stays by approximately 5 days to 6 days and adds thousands of dollars in medical costs.12
Aspiration pneumonia (AP) is caused by the aspiration of oropharyngeal secretions containing pathogenic bacteria into the lower airway.14 AP is particularly prevalent among older adults, especially those living in institutions. AP can also be community acquired or associated with health-care settings. AP is almost always caused by a mixed infection that includes anaerobic bacteria derived from the oral cavity, and most often develops in patients with elevated risk of aspirating oral contents into the lung, such as those with dysphagia15 or depressed consciousness.16
Patients diagnosed with AP tend to be older (mean age 77), with a 30-day mortality rate of 21%.17 Compared to CAP patients, AP patients tend to have more frequent inpatient and ICU?admissions, comorbidities, and higher rates of mortality. Risk factors include dependence for feeding and oral care; smoking; multiple medical diagnoses; high medication usage; and presence of dental caries, COPD, and diabetes.18
More recently, modifiable risk factors for pneumonia in elderly LTCF residents were identified in a prospective study of 613 older residents of five LTCFs.19 In this cohort, 18% developed pneumonia. Statistical modeling suggested that inadequate oral care and difficulty with swallowing were associated with pneumonia.
PATHOGENESIS OF PNEUMONIA
In healthy individuals, the lower airway presents formidable defense against aspirated bacteria.20 A viscous mucous layer coats the epithelium, which contains host-derived mucins, antimicrobial components, and other antimicrobial peptides.21 This coating traps bacteria that are then removed from the lung by the mucocutaneous escalator. Complex bacterial surface components interact with pattern-recognition receptors to activate inflammation through signaling pathways.22 Activation of these pathways recruits activated macrophages and neutrophils that engulf and dispose of the invading bacteria.
Pneumonia is the result of aspiration of infectious agents colonizing the oral cavity and/or upper respiratory tract.2 Any condition that compromises upper airway defenses will increase the risk for pneumonia by allowing aspirated bacteria to attach to the respiratory epithelium. For example, placement of an endotracheal tube through the larynx and trachea into the lung can provide a route for bacteria to bypass the structures that normally prevent aspirations, such as the glottis. Dysphagia also promotes aspiration and is very common among LTCF residents.23 Reduction in salivary flow, which occurs frequently in older adults most commonly as a side effect of medication usage, also contributes to increased risk for pneumonia by allowing enhanced microbial biofilm formation.24
Dysphagia can occur in the absence of overt signs of swallowing difficulty and is called “silent” aspiration.25 Certain conditions, such as stroke or impaired cough reflex, may increase the frequency of silent aspirations.
ORAL HEALTH AND PNEUMONIA
Prior to the mid 1990s, the role of oral conditions in the pathogenesis of pneumonia, particularly poor oral hygiene and periodontal inflammation, were mostly ignored in the medical arena, despite the fact that oral microflora was the known source of many infectious agents. This began to change as knowledge of oral microflora’s role in the pathogenesis of pneumonia became available.2 Much of the work at this time was performed on hospitalized patients, particularly mechanically ventilated patients in ICUs who had a substantially elevated risk for pneumonia. It was shown that teeth serve as a reservoir for respiratory pathogen colonization,26,27 and thus provide a source of bacteria in aspirated secretions. Further research also concluded that methods to improve oral hygiene in these populations could reduce the risk of pneumonia.28,29
Other studies suggested that the oral cavity might also serve as a reservoir for pulmonary infection.4,30 The oral cavities of elderly LTCF residents were more frequently found to harbor respiratory pathogens than those of ambulatory patients. A recent study reported the wearing of dentures during sleep doubles the risk for pneumonia,31 emphasizing the importance of oral biofilms in the etiology of pneumonia in older adults.
A case-control study compared the periodontal status of 100 individuals who were hospitalized for the treatment of an acute respiratory disease or an exacerbation of COPD to a group of 100 controls without respiratory disease.32 All periodontal parameters (gingival index, periodontal index, oral hygiene index, periodontal disease, and clinical attachment loss) for patients with respiratory disease were significantly worse than for the control subjects.
There is some evidence that periodontal diseases may be associated with pneumonia risk among older adults. A study of an elderly Japanese population found that the adjusted mortality rate due to pneumonia was 3.9 times higher among individuals with 10 or more teeth and probing depths exceeding 4 mm than in those without periodontal pockets.33
In light of these findings, it seems clear that oral hygiene or periodontal therapy would potentially help prevent the onset or progression of pneumonia in high-risk patients.
PNEUMONIA PREVENTION
The most common oral intervention used to prevent pneumonia in hospital settings is the application of antiseptics, such as chlorhexidine. A large number of studies have tested the effectiveness of chlorhexidine to reduce VAP rates.34–36 Several suggest that the topical application of chlorhexidine mouthrinse reduces pneumonia in mechanically ventilated patients, and may even decrease the need for systemic intravenous antibiotics or shorten the duration of mechanical ventilation. Also, oral application of chlorhexidine in the early post-intubation period appears to lower the number of cultivable oral bacteria and may delay the development of VAP.37 Mechanical oral hygiene also prevented mortality caused by pneumonia, and nonfatal pneumonia in hospitalized older adults and elderly LTCF residents.35 Improving oral hygiene may prevent approximately one in 10 cases of death from pneumonia in elderly LTCF residents.
Not all studies, however, have validated the effectiveness of oral chlorhexidine in reducing pneumonia. For example, gingival decontamination with chlorhexidine gel significantly decreased the prevalence of oropharyngeal colonization by pathogenic bacteria in ventilated patients, but this reduction was not sufficient to reduce the incidence of respiratory infections.38 Another study reported that a significant reduction in pneumonia through the use of chlorhexidine rinse among ICU patients was achieved only after 24 hours of intubation.39 A recent randomized trial compared twice-daily oral topical 0.2% chlorhexidine to 0.01% potassium permanganate (control) solution in 512 cardiac surgery patients.40 No differences were found between the groups with respect to nosocomial pneumonia, median day of development of pneumonia, median ICU stay, or mortality. A recent meta-analysis41 compared three methods for VAP prevention on infection and mortality: selective digestive decontamination, selective oropharyngeal decontamination, and topical oropharyngeal chlorhexidine. Interestingly, while selective digestive decontamination reduced mortality in ICU patients, both selective digestive decontamination and selective oropharyngeal decontamination were found to be superior to chlorhexidine. It was also noted that chlorhexidine was associated with increased mortality. There is a possibility that chlorhexidine has a toxic effect in this patient population.42
Other anti-plaque agents have been investigated. Oropharyngeal decontamination using topical antibiotics such as polymyxin B sulfate, neomycin sulfate, and vancomycin hydrochloride43 or gentamicin/colistin/vancomycin44 reduce VAP. Recently, mechanical oral care in combination with povidone iodine were found to significantly decrease pneumonia in ventilated ICU patients.45 These findings suggest that toothbrushing combined with a topical antimicrobial agent may be a promising method for oral cleansing of mechanically ventilated patients.
 Two randomized trials have tested the specific effect of toothbrushing to prevent VAP.46,47 Both studies evaluated the effect of power toothbrushing in addition to chlorhexidine rinse. While the addition of toothbrushing reduced the amount of visible dental plaque on the teeth,47 it did not reduce the incidence of VAP.46
Two randomized trials have tested the specific effect of toothbrushing to prevent VAP.46,47 Both studies evaluated the effect of power toothbrushing in addition to chlorhexidine rinse. While the addition of toothbrushing reduced the amount of visible dental plaque on the teeth,47 it did not reduce the incidence of VAP.46
Institutionalized but nonventilated patients may also benefit from improved oral care due to a reduction in the numbers of oral bacteria. Daily toothbrushing and topical oral swabbing with povidone iodine has been shown to significantly decrease pneumonia in LTCF residents.48 An earlier study, however, found that oral care with both brushing and antimicrobial gargling had an effect on fever incidence but not on pneumonia incidence.49 Professional prophylaxis by a dental hygienist once a week significantly reduced the prevalence of fever and fatal pneumonia in 141 elderly patients in LTCFs.50 Another study showed that once-a-week professional oral prophylaxis significantly reduced influenza infections in an older population.51 These studies suggest that improved oral care—even without chemical agents or a daily regimen—not only reduces the oral bacterial, viral, and fungal load, but also may help reduce the risk of pneumonia.
A systematic review of randomized controlled trials assessed the role of oral care in the prevention of LTCF-acquired pneumonia.35 This analysis suggested that oral hygiene interventions reduced rates of pneumonia and respiratory tract infection in elderly LTCF residents.
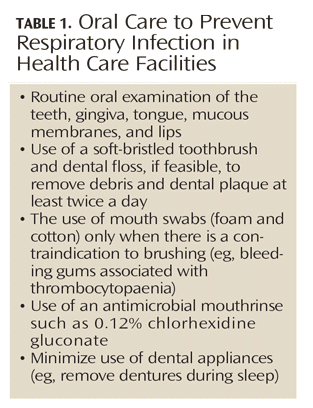
Oral cleansing reduces pneumonia in both edentulous and dentate subjects, suggesting that oral colonization of bacteria contributes to nosocomial pneumonia to a greater extent than periodontitis. However, intervention studies on the treatment of periodontitis and the incidence of pneumonia have not been performed due to the complexities required in investigating ICU or bed-bound LTCF patients. In edentulous individuals, dentures may easily serve as a similar reservoir as teeth for oral and respiratory bacteria if not cleaned properly every day. Practical suggestions for implementing oral care strategies to prevent pneumonia among vulnerable patients are listed in Table 1.
CHRONIC OBSTRUCTIVE PULMONARY DISEASE
COPD results in chronic airflow obstruction due to narrowing of the airways, with excess production of sputum resulting from chronic bronchitis and/or emphysema.52 Chronic bronchitis is the result of an insult to the bronchial airway and excessive secretion of mucus sufficient to cause cough with expectoration for at least 3 months of the year over 2 consecutive years.53 Emphysema results from the distention of the air spaces distal to the terminal bronchiole with destruction of the alveolar septa. Although this condition is associated with certain symptoms, the definitive diagnosis of emphysema can only be made histologically.
Approximately 20% to 30% of adults older than 45 have a history of chronic bronchitis.54 The incidence of emphysema is less well known because the main tool for noninvasive diagnosis (computed-tomography scanning) cannot be practically applied in population studies. While it is rare to find lungs completely free of emphysema post-mortem, most individuals do not show well defined histologic evidence of emphysema and do not have clinical symptoms of the disease.
The most significant risk factor for COPD is prolonged cigarette smoking. Other environmental risk factors include chronic exposure to toxic atmospheric pollutants (eg, secondhand smoke). Possible genetic risk factors include a defective alpha 1-antitrypsin gene, variant alpha 1-antichymotrypsin, alpha 2-macroglobulin, vitamin D-binding protein, and blood group antigen genes.55 These genetic defects account for only a small percentage of individuals with COPD.
Worldwide, the prevalence of COPD in adults age 40 and older is approximately 9% to 10%.56 In 2001, about 12.1 million adults older than 25 were diagnosed with COPD in the US, and another 24 million showed impaired lung function.57 It is likely that COPD remains underreported due to difficulties in the diagnosis. COPD is the fourth leading cause of morbidity and mortality in the US, and it is projected to be the fifth most common cause for morbidity and the third most frequent cause of mortality worldwide by 2020.57
COPD is caused by an inflammatory response to inhaled particles and gases in the lung, in most cases due to tobacco smoking (Figure 2).58 Smoking induces macrophage-predominant inflammation and airspace enlargement. High concentrations of reactive oxygen species in tobacco smoke result in oxidative stress. The resulting recruitment of macrophages leads to the release of proteases such as macrophage elastase, which seems to be a key pathogenic factor in tissue destruction. Not all smokers, however, get the disease. Thus, other factors may help explain why some individuals develop COPD while others do not.59,60 COPD is related to alpha-1 antitrypsin deficiency,62 although severity is affected by other risk factors such as gender, history of asthma, chronic bronchitis, and pneumonia. Some evidence demonstrates that COPD clusters in families. To date, attempts to associate COPD experience with specific genetic polymorphisms have proven inconclusive.60
It seems that an increase in the frequency of exacerbations is associated with bacterial infection.61 The bacterial species most often associated with the onset of exacerbation are nontypable H. influenzae, S. pneumoniae, and Moraxella catarrhalis. Viral infection has also been implicated in initiating this process.63 Thus, acute exacerbations of chronic obstructive pulmonary disease are often treated with empiric antibiotic therapy. The cost of therapy for this patient population is high. Treatment failure from routine antimicrobial therapy can cause hospitalization, respiratory failure, and death. Antibiotic therapy for exacerbations of COPD can also lead to emergence of antibiotic resistance and increased costs.
TREATMENT AND MANAGEMENT
Inhaled drug therapy is a common treatment for COPD. In severe cases, lung volume reduction surgery has been shown to reduce mortality, increase exercise capacity, and improve quality of life. Supplemental oxygen during exercise reduces exertional breathlessness and improves exercise tolerance of the hypoxemic patient. Noninvasive ventilation has been used as a palliative treatment to reduce dyspnea.
A recent systematic review concluded that antibiotics effectively reduce treatment failure and mortality rates in COPD patients with severe exacerbations.64 However, antibiotics may not be generally indicated for patients with mild to moderate exacerbations.
ORAL HEALTH IMPLICATIONS
A number of epidemiological studies have suggested an association between periodontal diseases and COPD. Relationships between respiratory diseases and oral health in community-dwelling populations were initially assessed by analysis of the National Health and Nutrition Examination Survey (NHANES ) I data.65 After controlling for gender, age, and race, subjects with a confirmed chronic respiratory disease had a significantly greater oral hygiene index than subjects without respiratory disease. Around this time, another study66 found that periodontal disease, measured as alveolar bone loss at baseline from periapical radiographs, was found to be an independent risk factor for COPD among adult male subjects.
These results were supported by a subsequent study that analyzed data from the NHANES III to determine if measures of periodontal diseases were associated with a history of bronchitis and/or emphysema, as well as with measures of lung function.67 Following statistical analysis that adjusted for gender, age, race, education, income, dental treatment history, alcohol consumption, diabetes status, and smoking history, the risk for COPD appeared to be significantly elevated when attachment loss was severe (?2.0 mm mean attachment loss [MAL]) as compared to periodontal health (< 2.0 mm MAL). Lung function also appeared to diminish as the amount of attachment loss increased.
The relationship between airway obstruction and periodontal diseases was examined in a cohort of 860 community-dwelling older adults enrolled in the Health, Aging, and Body Composition Study.68 Results showed that, after stratification by smoking status and adjustment for age, race, gender, and pack/years smoking, those with normal pulmonary function had significantly better gingival index and loss of attachment scores than those with airway obstruction. Thus, a significant association between periodontal diseases and airway obstruction was noted, especially in former smokers.
An association between chronic periodontitis and severe COPD was also supported by a recent study that demonstrated a greater prevalence of chronic periodontitis in 130 patients with severe COPD than in 50 patients with other severe respiratory diseases.69 It was found that the prevalence of periodontitis was 44% in the COPD group vs 7.3% in the nonCOPD group, and this difference remained significant after adjustment for age, gender, and pack/years smoked.
Additional epidemiologic studies have supported an association between periodontal disease experience and the frequency of COPD exacerbation70 and diminished lung function.71 Finally, a recent meta-analysis that analyzed data from 14 studies involving 3,988 COPD patients validated that a significant association between periodontal diseases and COPD exists.72
Fewer studies have addressed the efficacy of oral interventions to manage COPD. A recent trial sought to determine the effect of periodontal treatment on the frequency of exacerbations over 1 year in patients with COPD treated with scaling and root planing compared to patients who did not receive periodontal therapy.73 A statistically significant reduction was found in the exacerbation frequency for patients who received the periodontal intervention. More recently, the effects of scaling and root planing, supragingival scaling treatment, or oral hygiene instruction only with no periodontal treatment as measured by periodontal indices, respiratory function, and the frequency of COPD exacerbations at baseline, 6 months, 1 year, and 2 years were assessed.74 Results showed that both scaling and root planing and supragingival scaling improved periodontal indices and lung function, while at the same time reduced the frequency of COPD exacerbation at the 2-year follow-up. While these two trials provide promising results, additional large-scale, multicenter trials are required to verify these findings.
CONCLUSION
Understanding the risk factors and preventive measures for management of pneumonia and COPD is essential. Control of oral biofilm formation and periodontal disease activity in these populations appears to be a promising strategy that likely will reduce the number of potential respiratory pathogens in oral secretions, which, in turn, will reduce the risk of lung infection.
REFERENCES
- Wade WG. The oral microbiome in health and disease. Pharmacol Res. 2013;69:137–143.
- Scannapieco FA. Role of oral bacteria in respiratory infection. J Periodontol. 1999;70:793–802.
- Stein RT, Marostica PJ. Community-acquired pneumonia. Paediatr Respir Rev. 2006;7(Suppl 1):S136–137.
- Lutfiyya MN, Henley E, Chang LF, Reyburn SW. Diagnosis and treatment of community-acquired pneumonia. Am Fam Physician. 2006;73:442–450.
- Almirall J, Bolibar I, Serra-Prat M, et al. New evidence of risk factors for community-acquired pneumonia: a population-based study. Eur Respir J. 2008;31:1274–1284.
- Jackson ML, Neuzil KM, Thompson WW, et al. The burden of community-acquired pneumonia in seniors: results of a population-based study. Clin Infect Dis. 2004;39:1642–1650.
- Durrington HJ, Summers C. Recent changes in the management of community-acquired pneumonia in adults. BMJ. 2008;336:1429–1433.
- Tablan OC, Anderson LJ, Besser R, Bridges C, Hajjeh R. Guidelines for preventing health-care-associated pneumonia, 2003: recommendations of CDC and the Healthcare Infection Control Practices Advisory Committee. MMWR Recomm Rep. 2004;53:1–36.
- Mylotte JM. Nursing home-acquired pneumonia. Clin Infect Dis. 2002;35:1205–1211.
- Muder RR. Pneumonia in residents of long-term care facilities: epidemiology, etiology, management, and prevention. Am J Med. 1998;105:319–330.
- Vincent JL, Bihari DJ, Suter PM, et al. The prevalence of nosocomial infection in intensive care units in Europe. Results of the European Prevalence of Infection in Intensive Care (EPIC) Study. EPIC International Advisory Committee. JAMA. 1995;274:639–644.
- Kollef MH. Prevention of hospital-associated pneumonia and ventilator-associated pneumonia. Crit Care Med. 2004;32:1396–1405.
- Fagon JY, Chastre J, Hance AJ, Montravers P, Novara A, Gibert C. Nosocomial pneumonia in ventilated patients: a cohort study evaluating attributable mortality and hospital stay. Am J Med. 1993;94:281–288.
- Marik PE. Aspiration pneumonitis and aspiration pneumonia. N Engl J Med. 2001;344(9):665-71.
- van der Maarel-Wierink CD, Vanobbergen JN, Bronkhorst EM, Schols JM, de Baat C. Meta-analysis of dysphagia and aspiration pneumonia in frail elders. J Dent Res. 2011;90:1398–1404.
- Raghavendran K, Mylotte JM, Scannapieco FA. Nursing home-associated pneumonia, hospital-acquired pneumonia and ventilator-associated pneumonia: the contribution of dental biofilms and periodontal inflammation. Periodontol 2000. 2007;44:164–177.
- Lanspa MJ, Jones BE, Brown SM, Dean NC. Mortality, morbidity, and disease severity of patients with aspiration pneumonia. J Hosp Med. 2013;8:83–90.
- Terpenning MS, Taylor GW, Lopatin DE, Kerr CK, Dominguez BL, Loesche WJ. Aspiration pneumonia: dental and oral risk factors in an older veteran population. J Am Geriatr Soc. 2001;49:557–563.
- Quagliarello V, Ginter S, Han L, Van Ness P, Allore H, Tinetti M. Modifiable risk factors for nursing home-acquired pneumonia. Clin Infect Dis. 2005;40:1–6.
- Gellatly SL, Hancock RE. Pseudomonas aeruginosa: new insights into pathogenesis and host defenses. Pathog Dis. 2013;67:159–173.
- Gerson C, Sabater J, Scuri M, et al. The lactoperoxidase system functions in bacterial clearance of airways. Am J Respir Cell Mol Biol. 2000;22:665–671.
- Meijvis SC, van de Garde EM, Rijkers GT, Bos WJ. Treatment with anti-inflammatory drugs in community-acquired pneumonia. J Intern Med. 2012;272:25–35.
- Park YH, Han HR, Oh BM, et al. Prevalence and associated factors of dysphagia in nursing home residents. Geriatr Nurs. 2013;34:212–217.
- Gupta A, Epstein JB, Sroussi H. Hyposalivation in elderly patients. J Can Dent Assoc. 2006;72:841–846.
- . Ramsey D, Smithard D, Kalra L. Silent aspiration: what do we know? Dysphagia. 2005;20:218–225.
- El-Solh AA, Pietrantoni C, Bhat A, et al. Colonization of dental plaques: a reservoir of respiratory pathogens for hospital-acquired pneumonia in institutionalized elders. Chest. 2004;126:1575–1582.
- Heo SM, Haase EM, Lesse AJ, Gill SR, Scannapieco FA. Genetic relationships between respiratory pathogens isolated from dental plaque and bronchoalveolar lavage fluid from patients in the intensive care unit undergoing mechanical ventilation. Clin Infect Dis. 2008;47:1562–1570.
- Labeau SO, Van de Vyver K, Brusselaers N, Vogelaers D, Blot SI. Prevention of ventilator-associated pneumonia with oral antiseptics: a systematic review and meta-analysis. Lancet Infect Dis. 2011;11:845–854.
- Shi Z, Xie H, Wang P, et al. Oral hygiene care for critically ill patients to prevent ventilator-associated pneumonia. Cochrane Database Syst Rev. 2013;8:CD008367.
- Didilescu AC, Skaug N, Marica C, Didilescu C. Respiratory pathogens in dental plaque of hospitalized patients with chronic lung diseases. Clin Oral Investig. 2005;9:141–147.
- Iinuma T, Arai Y, Abe Y, et al. Denture wearing during sleep doubles the risk of pneumonia in the very elderly. J Dent Res. 2015;94(Suppl 3):28S–36S.
- Sharma N, Shamsuddin H. Association between respiratory disease in hospitalized patients and periodontal disease: a cross-sectional study. J Periodontol. 2011;82:1155–1160.
- Awano S, Ansai T, Takata Y, et al. Oral health and mortality risk from pneumonia in the elderly. J Dent Res. 2008;87:334–339.
- Scannapieco FA, Bush RB, Paju S. Associations between periodontal disease and risk for nosocomial bacterial pneumonia and chronic obstructive pulmonary disease. A systematic review. Ann Periodontol. 2003;8:54–69.
- Sjogren P, Nilsson E, Forsell M, Johansson O, Hoogstraate J. A systematic review of the preventive effect of oral hygiene on pneumonia and respiratory tract infection in elderly people in hospitals and nursing homes: effect estimates and methodological quality of randomized controlled trials. J Am Geriatr Soc. 2008;56:2124–2130.
- Roberts N, Moule P. Chlorhexidine and tooth-brushing as prevention strategies in reducing ventilator-associated pneumonia rates. Nurs Crit Care. 2011;16:295–302.
- Grap MJ, Munro CL, Elswick RK, Jr, Sessler CN, Ward KR. Duration of action of a single, early oral application of chlorhexidine on oral microbial flora in mechanically ventilated patients: a pilot study. Heart Lung. 2004;33:83–91.
- Fourrier F, Dubois D, Pronnier P, et al. Effect of gingival and dental plaque antiseptic decontamination on nosocomial infections acquired in the intensive care unit: a double-blind placebo-controlled multicenter study. Crit Care Med. 2005;33:1728–1735.
- Houston S, Hougland P, Anderson JJ, LaRocco M, Kennedy V, Gentry LO. Effectiveness of 0.12% chlorhexidine gluconate oral rinse in reducing prevalence of nosocomial pneumonia in patients undergoing heart surgery. Am J Crit Care. 2002;11:567–570.
- Panchabhai TS, Dangayach NS, Krishnan A, Kothari VM, Karnad DR. Oropharyngeal cleansing with 0.2% chlorhexidine for prevention of nosocomial pneumonia in critically ill patients: an open-label randomized trial with 0.01% potassium permanganate as control. Chest. 2009;135:1150–1156.
- Price R, MacLennan G, Glen J, Su DC. Selective digestive or oropharyngeal decontamination and topical oropharyngeal chlorhexidine for prevention of death in general intensive care: systematic review and network meta-analysis. BMJ. 2014;348:2197.
- Xue Y, Zhang S, Yang Y, et al. Acute pulmonary toxic effects of chlorhexidine (CHX) following an intratracheal instillation in rats. Hum Exp Toxicol. 2011;30:1795–1803.
- Pugin J, Auckenthaler R, Lew DP, Suter PM. Oropharyngeal decontamination decreases incidence of ventilator-associated pneumonia. A randomized, placebo-controlled, double-blind clinical trial. JAMA. 1991;265:2704–2710.
- Bergmans DC, Bonten MJ, Gaillard CA, et al. Prevention of ventilator-associated pneumonia by oral decontamination. A prospective, randomized, double-blind, placebo-controlled study. Am J Respir Crit Care Med. 2001;164:382–388.
- Mori H, Hirasawa H, Oda S, Shiga H, Matsuda K, Nakamura M. Oral care reduces incidence of ventilator-associated pneumonia in ICU populations. Intensive Care Med. 2006;32:230–236.
- Pobo A, Lisboa T, Rodriguez A, et al. A randomized trial of dental brushing for preventing ventilator-associated pneumonia. Chest. 2009;136:433–439.
- Needleman IG, Hirsch NP, Leemans M, et al. Randomized controlled trial of toothbrushing to reduce ventilator-associated pneumonia pathogens and dental plaque in a critical care unit. J Clin Periodontol. 2011;38:246–252.
- Yoneyama T, Yoshida M, Ohrui T, Mukaiyama H, Okamoto H, Hoshiba K, et al. Oral care reduces pneumonia in older patients in nursing homes. J Am Geriatr Soc. 2002;50:430–433.
- Yoneyama T, Hashimoto K, Fukuda H, et al. Oral hygiene reduces respiratory infections in elderly bed-bound nursing home patients. Arch Gerontol Geriatr. 1996;22:11–19.
- Adachi M, Ishihara K, Abe S, Okuda K, Ishikawa T. Effect of professional oral health care on the elderly living in nursing homes. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;94:191–195.
- Molloy J, Wolff LF, Lopez-Guzman A, Hodges JS. The association of periodontal disease parameters with systemic medical conditions and tobacco use. J Clin Periodontol. 2004;31:625–632.
- Ingram RH. Chronic bronchitis, emphysema, and airways obstruction. In: Isselbacher KJ, Braunwald E, Wilson JD, Martin JB, Fauci AS, Kasper DL, eds. Harrison’s Principles of Internal Medicine. New York: McGraw-Hill; 1994:1197–206.
- Society AT. Standards for the diagnosis and care of patients with chronic obstructive pulmonary disease. American Thoracic Society. Am J Respir Crit Care Med. 1995;152:77–121.
- Renwick DS, Connolly MJ. Prevalence and treatment of chronic airways obstruction in adults over the age of 45. Thorax. 1996;51:164–168.
- Sandford AJ, Weir TD, Pare PD. Genetic risk factors for chronic obstructive pulmonary disease. Eur Resp J. 1997;10:1380–1391.
- Halbert RJ, Natoli JL, Gano A, Badamgarav E, Buist AS, Mannino DM. Global burden of COPD: systematic review and meta-analysis. Eur Respir J. 2006;28:523–532.
- Skrepnek GH, Skrepnek SV. Epidemiology, clinical and economic burden, and natural history of chronic obstructive pulmonary disease and asthma. Am J Manag Care. 2004;10(Suppl 5):S129–S138.
- Fujita M, Nakanishi Y. The pathogenesis of COPD: Lessons learned from in vivo animal models. Med Sci Monit. 2007;13:19–24.
- Churg A, Wang R, Wang X, Onnervik PO, Thim K, Wright JL. An MMP-9/-12 inhibitor prevents smoke-induced emphysema and small airway remodeling in guinea pigs. Thorax. 2007;62:706–713.
- Molfino NA. Current thinking on genetics of chronic obstructive pulmonary disease. Curr Opin Pulm Med. 2007;13:107–113.
- Demeo DL, Sandhaus RA, Barker AF, et al. Determinants of airflow obstruction in severe alpha 1- antitrypsin deficiency. Thorax. 2007;62:806–813.
- Sethi S, Murphy TF. Acute exacerbations of chronic bronchitis: new developments concerning microbiology and pathophysiology—impact on approaches to risk stratification and therapy. Infect Dis Clin North Am. 2004;18:861–882.
- Papi A, Bellettato CM, Braccioni F, et al. Infections and airway inflammation in chronic obstructive pulmonary disease severe exacerbations. Am J Respir Crit Care Med. 2006;173:1114–1121.
- Puhan MA, Vollenweider D, Latshang T, Steurer J, Steurer-Stey C. Exacerbations of chronic obstructive pulmonary disease: When are antibiotics indicated? A systematic review. Respir Res. 2007;8:30.
- Scannapieco FA, Papandonatos GD, Dunford RG. Associations between oral conditions and respiratory disease in a national sample survey population. Ann Periodontol. 1998;3:251–256.
- Hayes C, Sparrow D, Cohen M, Vokonas PS, Garcia RI. The association between alveolar bone loss and pulmonary function: the VA Dental Longitudinal Study. Ann Periodontol. 1998;3:257–261.
- Scannapieco FA, Ho AW. Potential associations between chronic respiratory disease and periodontal disease: analysis of National Health and Nutrition Examination Survey III. J Periodontol. 2001;72:50–56.
- Katancik JA, Kritchevsky S, Weyant RJ, et al. Periodontitis and airway obstruction. J Periodontol. 2005;76:2161–2167.
- Leuckfeld I, Obregon-Whittle MV, Lund MB, Geiran O, Bjortuft O, Olsen I. Severe chronic obstructive pulmonary disease: association with marginal bone loss in periodontitis. Respir Med. 2008;102:488–494.
- Liu Z, Zhang W, Zhang J, et al. Oral hygiene, periodontal health and chronic obstructive pulmonary disease exacerbations. J Clin Periodontol. 2012;39:45–52.
- Holtfreter B, Richter S, Kocher T, et al. Periodontitis is related to lung volumes and airflow limitation: a cross-sectional study. Eur Respir J. 2013;42:1524–1535.
- Zeng XT, Tu ML, Liu DY, Zheng D, Zhang J, Leng W. Periodontal disease and risk of chronic obstructive pulmonary disease: a meta-analysis of observational studies. PLoS One. 2012;7:e46508.
- Kucukcoskun M, Baser U, Oztekin G, Kiyan E, Yalcin F. Initial periodontal treatment for prevention of chronic obstructive pulmonary disease exacerbations. J Periodontol. 2013;84:863–870.
- Zhou X, Han J, Liu Z, Song Y, Wang Z, Sun Z. Effects of periodontal treatment on lung function and exacerbation frequency in patients with chronic obstructive pulmonary disease and chronic periodontitis: a 2-year pilot randomized controlled trial. J Clin Periodontol. 2014;41:564–572.
From Dimensions of Dental Hygiene. April 2015;13(4):59–64.



