Dental Care for Patients With Heart Disease
Current approaches to ensure the safe provision of oral health services to individuals with hypertension and heart failure.
This course was published in the April 2015 issue and expires April 30, 2018. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Identify the prevalence of hypertension.
- Discuss the two types of hypertension and their implications for dental care.
- Define heart failure and discuss appropriate dental management strategies
Hypertension in adults is the persistent elevation of systolic blood pressure at or above 140 mm Hg and the diastolic blood pressure at or above 90 mm Hg.2 Hypertension is the leading cause of stroke and a major cause of myocardial infarction. In the US alone, more than 30% of adults have high blood pressure, with men and women equally affected.2,3 All health care providers—including dental hygienists—should become involved in the detection and prevention of hypertension. A dental office that routinely monitors patient blood pressure may discover untreated or inadequately treated hypertension in approximately one in five patients.4 Accurate readings, however, are contingent upon a properly sized and fitted blood pressure cuff, as well as correct placement. Cuffs placed too loosely or too low on the arm may result in inaccurate readings and subsequent misdiagnosis.4
Table 1 lists the four categories of blood pressure designated by the Seventh Joint National Committee on Prevention, Detection, Evaluation, and Treatment of Blood Pressure.5 For most adults, the treatment goal is less than 140 mm Hg/90 mm Hg; for patients with chronic renal disease or diabetes, the target is less than 130 mm Hg/80 mm Hg.5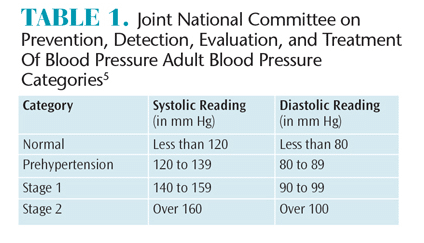
PRIMARY HYPERTENSION
There are two types of hypertension: primary and secondary. Also known as essential idiopathic hypertension, primary hypertension is the most common. It has an unknown etiology with a slow and gradual onset. The pathophysiology of primary hypertension is complex and related to arteriolar vasoconstriction with peripheralvascular resistance.6 Genetic predisposition, excessive salt intake, environmental factors, and adrenergic tone may interact to produce primary hypertension.4 Decreased renal flow associated with vasoconstriction may be related to the increase in blood pressure and volume.4 Increased vasoreactivity causing normal or reduced cardiac output and elevated systemic vascular resistance is also involved. Additionally, high salt and water reabsorption (salt sensitivity) by the kidney, which increases circulation of the volume of blood, may be a factor.3,7
SECONDARY HYPERTENSION
Secondary hypertension is caused by another medical condition affecting the cardiovascular system, endocrine system, renal system, or neurological system.3,4 It may also manifest with pregnancy and medication use, such as steroids and decongestants. The underlying medical condition must be addressed before secondary hypertension can be resolved. Individuals with secondary hypertension may not exhibit any symptoms, even if blood pressure has reached extremely high levels.8 Others may experience occipital headaches, dizziness, and ringing in the ears, but it is difficult to ascertain if high blood pressure or another health problem is causing the symptoms.9
Prolonged, uncontrolled hypertension causes renal failure and cardiovascular problems. Left ventricular hypertrophy arises with chronic hypertension—increasing the heart’s oxygen demand and workload. Increased susceptibility to ventricular fibrillation and death is a possible sequelae.10 Hypertension enhances the growth of coronary atherosclerosis—reducing blood flow to the myocardium and contributing to angina and myocardial infarctions. Long-term hypertension is also associated with vascular damage, accelerated atherosclerosis, retinal problems, and stroke.11
IMPLICATIONS FOR DENTAL TREATMENT
Clinicians should obtain current blood pressure readings at each new and recare visit or at least annually as a screening method for detecting hypertension. Clinical signs associated with severe hypertension should be documented. Blood pressure should continue to be monitored at subsequent appointments as indicated by condition, medication usage, and type of dental treatment. A physician’s consult is warranted when elevated blood pressure is detected or when a known hypertensive patient’s blood pressure is high.7 Readings at or above 180 mm Hg/110 mm Hg are contraindications for treatment.4 Failure to detect severely elevated blood pressure could result in a stroke or myocardial infarction. High blood pressure may be due to patients’ noncompliance with treatment recommendations, lack of a proper diagnosis, inappropriate medication usage, financial barriers to following recommendations, and/or inadequate treatment.4 Patients should be strongly encouraged to receive follow-up care from their physicians.
Pain management as part of pre- and post-operative dental hygiene care is important to keep blood pressure from elevating in patients with hypertension. Stress management protocols are also important. Patients with stage 1 hypertension or well-controlled hypertension have minimal risk involving dental care. Sedation with nitrous oxide may be appropriate for anxious patients.
When performing more complex surgical procedures, patients whose blood pressure is in the higher categories should undergo thorough risk assessment, and stress management protocols must be implemented. Uncontrolled hypertension (180 mm Hg/110 mm Hg) would necessitate the delay of elective dental treatment until the condition is under control. Patients should be referred to their physicians who will then need to provide a clearance for dental treatment. To ensure safety, epinephrine in local anesthetic injections should be limited to two cartridges of 1:100,000 epinephrine or four cartridges of 1 to 200,000 epinephrine.12,13
Many anti-hypertensive medications including diuretics, ?-adrenergic blocking agents, calcium channel blockers, and central alpha-2-adrenergic blocking agents have oral consequences, with xerostomia being the most prevalent. Patients should be encouraged to sip water throughout the day, and the use of calcium phosphate technologies may boost remineralization and reduce caries risk. Secretagogues may boost salivary production. Over-the-counter salivary substitutes can be recommended along with xylitol products to stimulate salivary flow. More frequent recare visits are important for patients with xerostomia. Calcium channel blockers may cause drug-induced gingival enlargement, which makes effective biofilm control of paramount importance. Consulting with a patient’s physician about substituting another hypertensive medication that does not cause gingival enlargement should be considered.
β–adrenergic blocking agents and calcium channel blockers are both associated with orthostatic hypotension and care must be taken to avoid moving the dental chair too quickly.7,13 Erythromycin and clarithromycin should be avoided in patients taking calcium channel blockers, as they increase the risk for hypotension.4 Additionally, nonsteroidal anti-inflammatory drugs should not be used for longer than 2 weeks because they can reduce the effectiveness of anti-hypertensive medications.7
Hypertension is an important modifiable risk factor for cardiovascular disease and stroke. Patient education should focus on modifying risk factors and encouraging patient participation in behaviors associated with a healthy lifestyle, as well as effective oral self-care measures (Table 2).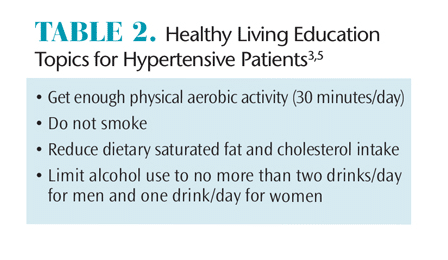
HEART FAILURE
Heart failure, or congestive heart failure, is an epidemic, affecting approximately 5.1 million people in the US, with more than 825,000 patients diagnosed each year.1 By 2030, projections indicate that 8 million people will experience heart failure, a 46% increase since 2012.1 Heart failure is the most common hospital discharge diagnosis in patients older than 65, and Medicare spends more money on the diagnosis and treatment of heart failure than any other condition.7 Survival after onset has improved; however, the mortality rate still remains at 50% within 5 years of diagnosis.1 Heart failure is a chronic condition, with an array of signs and symptoms that coincide with the part of the heart that is affected. Dyspnea (shortness of breath) upon exertion or lying supine, persistent cough, and expectoration are common findings in people with left-sided heart failure. Those with right-sided heart failure show signs of systemic venous congestion, peripheral edema (especially in the ankles and feet) and have cold feet and hands.7,14
Congestive heart failure is a progressive condition in which the heart pump cannot keep up with the metabolic demands of the body due to inadequate emptying (during systole) or filling (during diastole) of the ventricles. Heart failure represents the end stage of several pre-existing cardiovascular diseases, with the most common underlying causes being ischemic heart disease, cardiomyopathy, hypertension, valvular heart disease, myocarditis, and infective endocarditis.7 Heart failure may affect one or both of the ventricles, with left ventricular (LV) dysfunction most likely to present first. LV dysfunction is caused by an increase in workload or damage to the myocardium and is often followed by right ventricular (RV) dysfunction. LV dysfunction leads to an increase in blood in the ventricle, causing a boost in left atrial pressure, which leads to a boost in pressure of the capillaries in the lungs, causing pulmonary congestion and dyspnea.15 RV dysfunction results in higher pressure in the right atrium, causing increased pressure in the vena cava. This leads to impaired drainage from the body, resulting in venus congestion and peripheral edema.16 In an attempt to maintain normal cardiovascular homeostasis, dilation and hypertrophy of the ventricles occurs. While initially helpful, these compensatory mechanisms eventually worsen the severity of heart failure.15
There are two complementary systems to assess the severity of heart failure. The New York Heart Association (NYHA) classification categorizes patients into one of four categories based on their physical disability (Table 3).16 The American College of Cardiology (ACC) and American Heart Association (AHA) classification of heart failure consists of four stages ranging from A to D, emphasizing its progressive nature.17 Stage A and stage B represent patients who do not have signs or symptoms of heart failure, but have risk factors such as coronary artery disease, hypertension, or diabetes mellitus that predispose them to the disease.7,17 Patients progress from stage A to stage B when they develop LV hypertrophy or dysfunction. The majority of patients with heart failure are classified as stage C, having past or present symptoms associated with structural heart disease. Stage D represents patients with refractory heart failure who may require specialized treatment or end-of-life care.7,17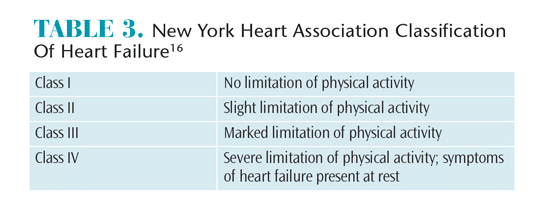
DENTAL HYGIENE MANAGEMENT
A detailed history of heart failure should be documented, including the date of diagnosis, underlying etiology, severity of the disease, medical management, and medication usage. Because heart failure is the end stage of many cardiovascular conditions, its cause should be identified so the dental hygienist can make the appropriate accommodations. Patients with uncontrolled or untreated heart failure should not receive elective dental treatment because they are at high risk for sudden death. They should be referred to their physicians.7,17,18 As part of conducting a thorough medical history, the patient’s vital signs—including blood pressure, pulse and rhythm, and respiration rate— should be evaluated at every appointment.
Dental hygienists should thoroughly review side effects, drug interactions, and oral manifestations of medications taken by patients with heart failure. Pharmacological agents may include diuretics, angiotensin-converting enzyme inhibitors, beta blockers, calcium channel blockers, aldosterone antagonists, angiotensin receptor antagonists, vasodilators, and digitalis glycosides.7,19,20 Each of these medications has potential side effects that may interfere with dental hygiene treatment. Oral side effects of diuretics are xerostomia, hypokalemia, and precipitation of arrhythmias.7 Saliva substitutes, sialogogues, and avoiding alcohol and caffeine consumption can be recommended to help alleviate xerostomia. Patients taking digitalis glycosides, such as digoxin, are more prone to an exaggerated gag reflex, so procedures that may induce gagging, such as taking X-rays or impressions, should be performed with additional care.15 Additionally, digoxin toxicity can easily occur due to its narrow therapeutic range.19 Patients should be monitored for clinical manifestations of digoxin toxicity such as vomiting, nausea, hypersalivation, blurring or yellowing of vision, and headache.14,19 If toxicity is suspected, the patient should be referred for medical evaluation immediately.
Facilitating a stress-free appointment to avoid an increased workload on the failing heart and prevent a cardiac crisis is important. If possible, treatment should be broken up into short appointments so the patient is not overwhelmed. Stress management strategies include developing a trusting relationship between patient and practitioner, effective pain management strategies, and nitrous oxide sedation. Stress-induced comorbidities like hypertension, anxiety, and tachycardia can be reduced by sedation.19 In addition to reducing anxiety, supplemental low-flow oxygen is beneficial for patients with heart failure who experience dyspnea. Patients with heart failure tolerate epinephrine well; however, a maximum of 0.04 mg epinephrine (ie, two cartridges of anesthetic with 1:100,000 epinephrine) is recommended.19,20 Epinephrine is contraindicated for patients categorized as NYHA Class III or IV, or patients taking digitalis medications due to the increased risk of epinephrine-induced arrhythmias.19
Additional modifications may be needed to facilitate a safe and effective appointment for patients with heart failure. For example, ultrasonic instrumentation should be limited so unnecessary fluid does not back up in the patient’s mouth, as fluid reduction minimizes anxiety and facilitates breathing.15 Additionally, an upright or semi-supine chair position should be implemented for patients who cannot tolerate the supine position due to pulmonary edema or orthopnea.14,18 The dental chair should also be raised slowly to prevent orthostatic hypotension.
As part of promoting oral and overall health, dental hygienists should encourage patients to live a healthy lifestyle. Smoking cessation, maintaining or achieving a healthy bodyweight, sufficient sleep, moderation of alcohol use, and mild aerobic exercise should be recommended.21–23 Nutritional counseling may also be necessary to counsel patients with heart failure on reduced sodium diet to alleviate fluid retention.14
CONCLUSION
Hypertension and heart failure are common cardiovascular diseases that affect many dental patients. Oral health professionals must be prepared to identify systemic conditions by thoroughly reviewing patients’ medical histories. An understanding of disease characteristics, stress and pain management protocols, and medication side effects is necessary to ensure appropriate treatment modifications are implemented so patients can be treated safely and effectively.
REFERENCES
- Go AS, Mozaffarian D, Roger VL, et al. Heart disease and stroke statistics—2014 update: A report from the American Heart Association. Circulation. 2013;129:28–292.
- Centers for Disease Control and Prevention. High Blood pressure. Available at: cdc.gov/bloodpressure/ facts.htm. Accessed March 17, 2015.
- Mayo Clinic. High Blood Pressure (Hypertension). Available at: mayoclinic.org/diseases-conditions/high-bloodpressure/basics/definition/con-20019580. Accessed March 17, 2015.
- Yagiela JA, Haymore TL. Management of the hypertensive dental patient. J Calif Dent Assoc. 2007;35:51–59.
- National Institute of Health. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure. Available at: nhlbi.nih.gov/files/docs/ guidelines/jnc7full.pdf. Accessed March 17, 2015.
- Singleton J, DiGregoria R, Green-Hernandez C, Holzmer S, Faber E, Ferrara L., Slyer J. Primary Care. 2nd ed. New York: Springer Publishing Company; 2015.
- Little J, Falace D, Miller C, Rhodus N. Dental Management of the Medically Compromised Patient. 8th ed. St. Louis: Elsevier: 2013.
- Fuster V, Walsh R, Harrington R. Hurst’s The Heart. 13th ed. New York: McGraw-Hill; 2011.
- Rosdahi C, Kowalski M. Textbook of Basic Nursing. 10th ed. Philadelphia: Wolters Kluwer; 2011.
- . Katz J, Steinberg P. Coronary Artery Disease. Available at: nursingceu.com/courses/ 398/index_nceu.html. Accessed March 17, 2015.
- Lynn P. Taylor’s Clinical Nursing Skills. Philadelphia: Wolters Kluwer; 2014.
- Weyant R. There is minimal risk for adverse events in hypertensives associated with the use of epinephrine in local anesthetics. J Evid Base Dent Prac. 2007;7:60–61.
- Chidambaram R. Protocols for Hypertensive Patient Management in the Dental Office—Short Communication. Available at: ijmd.ro/ articole/328_17_pdf_IJMD%204-2013%20tipo.pdf. Accessed March 17, 2015.
- Darby ML, Walsh MM. Dental Hygiene Theory and Practice. 4th ed. St. Louis: Elsevier; 2015.
- Kemp C, Conte J. The pathophysiology of heart failure. Cardiovasc Pathol. 2012;21:365–371.
- American Heart Association. Classes of Heart Failure. Available at: heart.org/HEARTORG/ Conditions/HeartFailure/AboutHeartFailure/Classes-of-Heart-Failure_UCM_306328_Article.jsp. Accessed March 17, 2015.
- Jessup M, Abraham WT, Casey, DE, et al. Focused update incorporated into the ACC/AHA 2005 guidelines for the diagnosis and management of heart failure in adults: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2009;53:1–90.
- Newman M, Takei H, Klokkevold P, Carranza F. Carranza’s Clinical Periodontology. 12th ed. St. Louis: Elsevier; 2015.
- Herman W, Ferguson H. Dental care for patients with heart failure: An update. J Am Dent Assoc. 2010;141:845–853.
- Munoz MM, Soriano YJ, Roda RP, Sarrion G. Cardiovascular diseases in dental practice. Practical considerations. Med Oral Patol Oral Cir Bucal. 2008;13:296–302.
- Nilsson BB, Westheim A, Risberg MA. Effects of group-based high-intensity aerobic interval training in patients with chronic heart failure. Am J Cardiol. 2008;102:1361–1365.
- Muller L, Myers J, Kottman W, et al. Exercise capacity, physical activity patterns and outcomes six years after chronic rehabilitation in patients with heart failure. Clin Rehabil. 2007;21:923–931.
- Dracup K, Evangelista LS, Hamilton MA, et al. Effects of a home-based exercise program on clinical outcomes of heart failure. Am Heart J. 2007;154:877–833.
From Dimensions of Dental Hygiene. April 2015;13(4):65–68.



