The Evolution of Air Polishing
This dynamic technique is a helpful addition to the dental hygiene armamentarium.
This course was published in the May 2015 issue and expires May 31, 2018. The author has no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Identify the abrasiveness of air polishing powders.
- Describe the appropriate use of subgingival air polishing.
- List the indications for this technique.
- Explain the risks inherent to air polishing use.
When specially designed, low-abrasive powders are used, air polishing can subgingivally deplaque 3 mm to 4 mm pockets during periodontal maintenance. Glycine powder air polishing (GPAP), which uses a low abrasive powder and a uniquely designed handpiece with a special nozzle, can remove plaque from deeper pockets (up to 10 mm).3
ABRASIVES IN AIR POLISHING POWDERS
Table 1 summarizes the various types of abrasive powders. The abrasiveness of air polishing powders is affected by several factors, including hardness, mass, shape, and fragmentation ability. Particle mass, determined by its density and size, significantly affects the particle’s kinetic energy. When speeds are the same, a particle with more mass will have more energy than a particle with less mass. Increased hardness and angularity also increase abrasiveness, while the tendency toward fragmentation decreases abrasiveness.3 Comparing abrasiveness of air polishing powders can be difficult due to these variables.
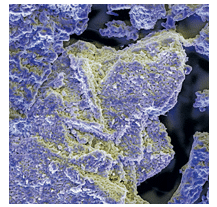
Sodium bicarbonate has been commonly used in air polishing for decades (Figure 1). Though its Mohs hardness level is low at 2.54 sodium bicarbonate is effective in removing most stains. Sound enamel is not damaged when sodium bicarbonate is used with proper technique, but it can significantly damage dentin, as well as composite and glass ionomer restorations.5 Sodium bicarbonate powder is contraindicated for use on root structures because it can cause defects within seconds.6
Aluminum trihydroxide is a sodium-free alternative to sodium bicarbonate. It has a Mohs value of 4 and is more abrasive than sodium bicarbonate. Its hardness and large particle size make it an excellent stain remover, but its use is limited to enamel.7
Calcium carbonate powder (Figure 2) has a Mohs value of 3 and is available in round particles.8 It can, however, cause defects on root surfaces.2 Bioactive glass, or calcium sodium phosphosilicate, has a particle size of 30 ?m to 90 ?m.9 With a Mohs value of 6, it has the potential to cause significant abrasion. In a recent pilot study, enamel surfaces subjected to air polishing with bioactive glass were qualitatively similar to pretreated surfaces (ie, unchanged), while cementum was altered by the uptake of minerals. Study parameters, however, may not have been sufficient to elicit the true effect on enamel, and quantitative tissue changes were not determined.10
Bioactive glass removes stain but is also marketed as a therapeutic prophy powder for treatment of dentin hypersensitivity and repair of dental tissues.11–13 Because it contains calcium and phosphorus, bioactive glass powder has remineralization properties and may occlude dentinal tubules. With its remineralizing capacity, it may have application in treatment of white spot lesions. Banerjee et al13 demonstrated that air polishing with bioactive glass powder was more effective in whitening and desensitizing than sodium bicarbonate, and patients experienced less discomfort.
LOW-ABRASIVE POWDERS
Low-abrasive powders that can be used safely in subgingival air polishing are made from either glycine or erythritol. The high abrasiveness of sodium bicarbonate, calcium carbonate, and bioactive glass contraindicate their use subgingivally. GPAP is more gentle on gingival tissue and significantly less abrasive on root structure than sodium bicarbonate.6 One study, however, showed that GPAP removed 33.9 ?m of root structure in a 20-second application.3 The clinical significance of the removal of this amount of root structure is unclear. GPAP’s deplaquing ability combined with its gentleness make it an excellent choice for use on orthodontic patients.
Erythritol, a noncariogenic sugar alcohol used as a sweetener,14 is effective in subgingival biofilm removal. Its small particle size (14 ?m) is similar to the smaller glycine particles and may limit soft tissue and root damage.15 Erythritol also exerts negative effects on mutans streptococci.16 While not yet available in the United States, more research is in progress on this potentially promising new air polishing powder.
INDICATIONS
While all air polishing powders remove biofilm, research demonstrates that sodium bicarbonate, aluminum hydroxide, and bioactive glass are also effective in stain removal.13 Because of its extreme abrasiveness, use of aluminum hydroxide should be restricted to heavy stain only.
Air polishing with sodium bicarbonate or glycine powder has been shown to safely and effectively remove biofilm from orthodontic wires and brackets.17 If the archwire is removed, however, the bracket slots should be avoided to prevent damage.1 Extended application times with sodium bicarbonate can roughen plastic brackets, so care should be taken to use the appropriate duration of 3 seconds to 5 seconds for several teeth. Glycine powder is less abrasive and does not roughen plastic brackets as much as sodium bicarbonate.17 Air polishing around bands should be avoided because it may remove the cement used for band retention.18
Occlusal plaque removal prior to sealant placement is more effective in air polishing with sodium bicarbonate than a rotary bristle brush.19 Additionally, sealants experience less microleakage when surfaces are precleaned with sodium bicarbonate air polishing compared to rubber cup polishing with pumice slurry, use of a dry bristle brush, or an extended etch time.20
Glycine’s low abrasiveness enables it to be used safely supragingivally around gingival tissue as well as subgingivally. Subgingival deplaquing via hand instrumentation resulted in more tissue irritation than 5 seconds of GPAP.21
RISKS
As is the case with other dental hygiene procedures, air polishing does come with certain risks. Because of the risk of gingival penetration, any patient who requires antibiotic prophylaxis to prevent endocarditis will need premedication prior to treatment.22 Air polishing is contraindicated for patients with respiratory difficulties because they may develop infections from inhaling aerosols produced during the procedure. Air polishing should be used with caution on patients who have difficulty breathing or swallowing. Close monitoring and adequate suction are imperative if air polishing is used on these patients.
Because carbonates can affect blood pH, both sodium bicarbonate and calcium carbonate should not be used on patients who have limited buffering capacity against pH changes in the blood. This includes patients with kidney disease or adrenal dysfunction, as well as those taking mineral corticosteroids.23
Though incidences are rare, use of pressurized air can result in facial subcutaneous emphysema if air penetrates into a connective tissue space.24 As such, traditional air polishing nozzles should never be directed into periodontal tissues.3,25 Symptoms of facial emphysema include facial swelling, tenderness, and pain. Patients exhibiting these symptoms must receive immediate medical care to prevent serious health problems. While the risk of facial emphysema is low, clinicians should closely follow all manufacturer instructions when using air polishing devices to reduce the likelihood of this occurring.
Inadvertent gingival irritation is common with air polishing. Trauma is difficult to avoid because biofilm and stain often reside near the gingival margin.26–29 A recent study comparing gingival effects of air polishing demonstrated that glycine produces less gingival trauma than sodium bicarbonate.21 Air polishing with any abrasive is contraindicated immediately after periodontal debridement29 or when an acute gingival condition exists, due to an increased risk of tissue trauma and facial emphysema.
Air polishing can damage esthetic restorations and sealants.7,18,30,31 Research has shown that both sodium bicarbonate and glycine remove sealant material, although glycine removed considerably less.30 Aluminum trihydroxide, sodium bicarbonate, and glycine harmed composite restorations, with glycine resulting in less surface damage.7,18,31,32 Glass ionomers were also damaged with sodium bicarbonate, but no research was found on the effect of glycine.33
Gold and amalgam surfaces may be dulled by air polishing with sodium bicarbonate and aluminum trihydroxide. Johnson et al7 recommend avoiding polishing on metallic restorations with either abrasive. Though porcelain is not adversely affected, luting cements used on fixed prosthetics are easily removed by air polishing. To maintain integrity of cast restorations, air polishing around margins should be avoided.32 Titanium implant abutments, however, are not damaged by air polishing. In fact, milling grooves may actually be smoothed by air polishing.34
PREPARATION
Fundamental technique for traditional air polishing has not changed. Because substantial aerosols are produced during air polishing, patients’ neck and upper torso areas should be covered with a moisture-resistant apron. Lip balm is recommended to protect the lips from the drying effects of the powder. Placing a gauze square on the patient’s tongue during the procedure minimizes taste from the abrasive. The clinician and assistant, who handles the high-evacuation suction, should wear disposable or washable long-sleeved overgarments and hair covers in addition to typical personal protective equipment.29
In traditional air polishing, circular strokes are made with the nozzle held approximately 3 mm to 5 mm from the tooth surface. Direct the spray on an area (one to two teeth) for no longer than 3 seconds to 5 seconds and rotate the nozzle to reach around line angles as needed.35 Manufacturer instructions regarding the angle of spray should be followed. Again, traditional-use nozzles with abrasive powders should never be directed into the sulcus or pocket, and extreme care should be used to avoid inadvertent spraying into the gingival area to avoid soft tissue damage. While GPAP can be used subgingivally, clinicians should be well versed in appropriate technique before using this modality.
CONCLUSION
While all air polishing powders are effective in supragingival biofilm removal, only sodium bicarbonate, aluminum hydroxide, and bioactive glass are also effective in stain removal.13 GPAP is the only technique that can be used in subgingival biofilm removal.3 Air polishing has become a dynamic procedure, with new products and applications being developed. Oral health professionals will need to stay abreast of new scientific data regarding the efficacy and safety of air polishing in order to support their clinical decision making.
REFERENCES
- Graumann SJ, Sensat ML, Stoltenberg JL. Air polishing: a review of current literature. J Dent Hyg. 2013;87:173–180.
- Pelka M, Trautmann S, Petschelt A, Lohbauer U. Influence of air-polishing devices and abrasives on root dentin-an in vitro confocal laser scanning microscope study. Quintessence Int. 2010;41:e141–148.
- Petersilka GJ. Subgingival air-polishing in the treatment of periodontal biofilm infections. Periodontol 2000. 2011;55:124–142.
- Lehne RK, Winston AE. Abrasivity of sodium bicarbonate. Clin Prev Dent. 1983;5:17–18.
- Atkinson DR, Cobb CM, Killoy WJ. The effect of an air-powder abrasive system on in vitro root surfaces. J Periodontol. 1984;55:13–18.
- Petersilka GJ, Bell M, Häberlein I, Mehl A, Hickel R, Flemmig TF. In vitro evaluation of novel low abrasive air polishing powders. J Clin Periodontol. 2003;30:9–13.
- Johnson WW, Barnes CM, Covey DA, Walker MP, Ross JA. The effects of a commercial aluminum airpolishing powder on dental restorative materials. J Prosthodont. 2004;13:166–172.
- Frankenberger R, Lohbauer U, Tay FR, Taschner M, Nikolaenko SA. The effect of different airpolishing powders on dentin bonding. J Adhes Dent. 2007;9:381–389.
- White Paper Report: Sylc—The Science Behind the Powder. Available at: dent2go.net/pdffiles/ Whitepaper.pdf Accessed February 19, 2015.
- Janicki T, Sobczak-Kupiec A, Skomro P, Wzorek Z. Surface of root cementum following air-polishing with bioactive hydroxyapatite (Ca and P mapping). A pilot study. Acta Bioeng Biomech. 2012;14:31–38.
- Sauro S, Watson TF, Thompson I. Dentine desensitization induced by prophylactic and airpolishing procedures: An in vitro dentine permeability and confocal microscopy study. J Dent. 2010;38:411–422.
- Sauro S, Watson TF, Thompson I. Ultramorphology and dentine permeability changes induced by prophylactic procedures on exposed dentinal tubules in middle dentine. Med Oral Patol Oral Cir Bucal. 2011;16:e1022–1030.
- Banerjee A, Hajatdoost-Sani M, Farrell S, Thompson I. A clinical evaluation and comparison of bioactive glass and sodium bicarbonate airpolishing. J Dent. 2010;38:475–479.
- Moon HJ, Jeya M, Kim IW, Lee JK. Biotechnological production of erythritol and its applications. Appl Microbiol Biotechnol. 2010;86:1017–1025.
- Daubert DM. Subgingival air polishing. Dimensions of Dental Hygiene. 2013;11:69–73.
- Runnel R, Mäkinen KK, Honkala S, et al. Effect of three-year consumption of erythritol, xylitol and sorbitol candies on various plaque and salivary caries-related variables. J Dent. 2013;41:1236–1244.
- Wilmes B, Vali S, Drescher D. In-vitro study of surface changes in fixed orthodontic appliances following air polishing with Clinpro Prophy and Air- Flow. J Orofac Orthop. 2009;70:371–384.
- Barnes CM, Hayes EF, Leinfelder KF. Effects of an airabrasive polishing system on restored surfaces. Gen Dent. 1987;35:186–189.
- Botti RH, Bossù M, Zallocco N, Vestri A, Polimeni A. Effectiveness of plaque indicators and air polishing for the sealing of pits and fissures. Eur J Paediatr Dent. 2010;11:15–18.
- Agrawal A, Shigli A. Comparison of six different methods of cleaning and preparing occlusal fissure surface before placement of pit and fissure sealant: an in vitro study. J Indian Soc Pedod Prev Dent. 2012;30:51–55.
- Petersilka G, Faggion CM Jr, Stratmann U, et al. Effect of glycine powder air-polishing on the gingiva. J Clin Periodontol. 2008;35:324–332.
- Wilson W, Taubert KA, Gewitz M, et al. Prevention of infective endocarditis: guidelines from the American Heart Association: a guideline from the American Heart Association Rheumatic Fever, Endocarditis and Kawasaki Disease Committee, Council on Cardiovascular Disease in the Young, and the Council on Clinical Cardiology, Council on Cardiovascular Surgery and Anesthesia, and the Quality of Care and Outcomes Research Interdisciplinary Working Group. J Am Dent Assoc. 2008;139 (Suppl:)3S–24S.
- Hodges KO. Concepts in Nonsurgical Periodontal Therapy. Boston: Delmar; 1998:351–354.
- Neville B. Oral and Maxillofacial Pathology. 3rd ed. St. Louis: Saunders Elsevier; 2008;323.
- Flemmig TF, Hetzel M, Topoll H, Gerss J, Haeberlein I, Petersilka G. Subgingival debridement efficacy of glycine powder air polishing. J Periodontol. 2007;78:1002–1010.
- Kontturi-Närhi V, Markkanen S, Markkanen H. The gingival effects of dental airpolishing as evaluated by scanning electron microscopy. J Periodontol. 1989;60:19–22.
- Mishkin DJ, Engler WO, Javed T, Darby TD, Cobb RL, Coffman MA. A clinical comparison of the effect on the gingiva of the Prophy-Jet and the rubber cup and paste techniques. J Periodontol. 1986;57:151–154.
- Weaks LM, Lescher NB, Barnes CM, Holroyd SV. Clinical evaluation of the Prophy-Jet as an instrument for routine removal of tooth stain and plaque. J Periodontol. 1984;55:486–488.
- Wilkins EM. Clinical Practice of the Dental Hygienist. 11th ed. Philadelphia: Lippincott Williams & Wilkins; 2013:703–705.
- Engel S, Jost-Brinkmann PG, Spors CK, Mohammadian S, Müller-Hartwich R. Abrasive effect of air-powder polishing on smooth-surface sealants. J Orofac Orthop. 2009;70:363–370.
- Giacomelli L, Salerno M, Derchi G, Genovesi A, Paganin PP, Covani U. Effect of air polishing with glycine and bicarbonate powders on a nanocomposite used in dental restorations: an in vitro study. Int J Periodontics Restorative Dent. 2011;31:e51–e56.
- Salerno M, Giacomelli L, Derchi G, Patra N, Diaspro A. Atomic force microscopy in vitro study of surface roughness and fractal character of a dental restoration composite after air-polishing. Biomed Eng Online. 2010;12:59.
- Carr MP, Mitchell JC, Seghi RR, Vermilyea SG. The effect of air polishing on contemporary esthetic restorative materials. Gen Dent. 2002;50:238–241.
- McCollum J, O’Neal RB, Brennan WA, Van Dyke TE, Horner JA. The effect of titanium implant abutment surface irregularities on plaque accumulation in vivo. J Periodontol. 1992;63:802–805.
- Darby ML. Mosby’s Comprehensive Review of Dental Hygiene. 6th ed. St. Louis: Mosby Elsevier; 2006:727.
From Dimensions of Dental Hygiene. March 2015;13(3):58–61.



