
The Critical Component
Effective hand hygiene is a fundamental part of an infection prevention and control program.
Hand hygiene has long been recognized as an important element of an infection prevention and control program. The success of any hand hygiene program is based on using appropriate techniques and selecting effective products.
The Centers for Disease Control and Prevention (CDC) estimates that nearly 2 million patients get an infection while hospitalized and almost 90,000 die as a result of these infections each year.1 The most common mode of transmission of health care-associated infections is through contaminated hands, making hand hygiene a major focus in all health care settings.2 The United Nations issued a report on November 11, 2006, stating that “Hand hygiene remains the primary measure to reduce health care-associated infection and spread of antimicrobial resistance…it enhances the safety of care across all settings, from complex modern hospitals to simple health posts.”
HAND HYGIENE BEGINS
Inadequate hand hygiene was associated with the spread of infection and mortality as far back as 1846 when Dr. Ignaz Semmelweiss noted that mortality among women delivering babies in hospital wards with and without medical students differed. The mortality rate was higher in those hospitals where medical students attended births directly after leaving the pathology laboratory because they did not wash their hands upon exiting the laboratory. Semmelweiss introduced hand washing protocols and the mortality rate dropped to less than 1%.3
Dr. Oliver Wendell Holmes concluded that health care practitioners who did not wash their hands transmitted puerperal fever. Unfortunately, it was many years before his recommendations for hand washing were incorporated into standard surgical practice.4
In 2003, the CDC released updated guidelines for infection control in dental settings.1 Incorporated within this guidance are recommendations from other CDC guidelines released in years previous to 2003, including those for personnel health, environmental health, and hand hygiene. The CDC recognizes that “hand hygiene substantially reduces potential pathogens on the hands and is considered the single most critical measure for reducing the risk of transmitting organisms to patients and health care personnel.”1 Compliance with hand hygiene protocols remains a challenge for many health care settings. Gloving is not a substitute for handwashing—gloving follows handwashing as an engineering control to further reduce the risk of transmission of and exposure to potentially infectious organisms.1,5
Hand hygiene is an infection prevention and control priority in the United States and worldwide. The World Health Organization (WHO) has identified hand hygiene as a major priority in addressing the global patient safety challenge of “Clean Care Is Safer Care.” In April 2006, WHO published WHO Guidelines on Hand Hygiene in Health Care.6
Hand hygiene is a general term that applies to handwashing, antiseptic handwash, alcohol-based handrub, or surgical hand hygiene/antisepsis procedures. Selecting the specific method for hand hygiene depends on the type of procedure, the anticipated degree of contamination, and the desired persistence of antimicrobial action on the skin. The CDC recommends that hand hygiene be done when hands are visibly soiled, after barehanded touching of inanimate objects likely to be contaminated, before and after treating patients, before donning gloves, and immediately after their removal. Hand hygiene is also indicated if gloves become compromised during a procedure and need to be replaced.1
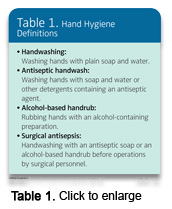 In selecting the appropriate hand hygiene method, understanding the various types of hand hygiene is key (Table 1). The following definitions are adapted from the CDC Guideline for Hand Hygiene.5
In selecting the appropriate hand hygiene method, understanding the various types of hand hygiene is key (Table 1). The following definitions are adapted from the CDC Guideline for Hand Hygiene.5
- Handwashing is washing hands with plain soap and water. Hand washing removes dirt and transient microorganisms.
- Plain soap is a detergent (surfactant) product that does not contain an antiseptic agent at a concentration, which is sufficient to reduce or inhibit the growth of microorganisms.
- Antiseptic handwashing is washing hands with water and soap or other detergents containing an antiseptic agent. Antiseptic handwash agents remove dirt, transient microorganisms, and some resident microorganisms
- Antiseptic agents are antimicrobial substances that reduce or inhibit the growth of microorganisms on living tissues. Examples include alcohols, chlorhexidine gluconate, chlorhexidine derivatives, iodine, PCMX, and triclosan.
- Alcohol-based handrubs are alcohol-containing antiseptic agents designed to reduce the growth of microorganisms when applied to the hands. These liquid, gel, or foam preparations may contain one or more types of alcohol and other active ingredients. Alcohol-based handrubs do not contain detergents and are, therefore, not good cleaning agents.
- Surgical hand antisepsis requires two steps. Step one is a surgical hand scrub with an antiseptic handwash agent. Step two is either second antiseptic handwash or application of an alcohol-based handrub. All surgical personnel prior to donning surgical gloves must perform surgical hand hygiene pre-operatively. Antiseptic preparations for surgical hand hygiene should have persistent (long-lasting) antimicrobial activity.
METHODS FOR ROUTINE PROCEDURES
 CDC recommends performing hand hygiene with either a nonantimicrobial (plain soap) or antimicrobial soap and water when hands are visibly dirty or potentially contaminated. Dental health care personnel (DHCP) have choices in hand hygiene agents for use in routine procedures (Table 2). If hands are not visibly dirty or contaminated, an alcohol-based handrub is adequate. Handwashing should be performed prior to routine dental examinations and nonsurgical procedures. Health care workers have choices in hand hygiene for routine dental procedures. Plain detergents/soap are adequate for cleaning. Liquid or foam soaps are less likely to become contaminated than reusable bar soaps. Plain soap is good for reducing bacterial counts. Antimicrobial soap or antiseptic handwash agents that contain detergents remove dirt and also remove the transient microorganisms and reduce or destroy resident microorganisms on the skin.1
CDC recommends performing hand hygiene with either a nonantimicrobial (plain soap) or antimicrobial soap and water when hands are visibly dirty or potentially contaminated. Dental health care personnel (DHCP) have choices in hand hygiene agents for use in routine procedures (Table 2). If hands are not visibly dirty or contaminated, an alcohol-based handrub is adequate. Handwashing should be performed prior to routine dental examinations and nonsurgical procedures. Health care workers have choices in hand hygiene for routine dental procedures. Plain detergents/soap are adequate for cleaning. Liquid or foam soaps are less likely to become contaminated than reusable bar soaps. Plain soap is good for reducing bacterial counts. Antimicrobial soap or antiseptic handwash agents that contain detergents remove dirt and also remove the transient microorganisms and reduce or destroy resident microorganisms on the skin.1
The CDC recommends using cool to luke-warm water for hand washing. Hot water can open skin pores of the hands and be irritating to the skin and may lead to irritant dermatitis.1
When the hands are clean, antiseptic alcohol-based handrub agents can be used between patients, eg, before donning gloves and after removal of gloves. Scientific evidence shows that alcohol-based handrubs are good at reducing microbial counts, but are not good cleaning agents and should only be used on clean hands.1 Alcohol rubs are effective in removing transient microorganisms and reducing or destroying resident microorganisms, but only when the skin is clean, not visibly dirty. The CDC recommends selecting an agent that has persistent activity to prevent or inhibit survival of microorganisms after the product is applied.5
Manufacturer instructions for use should be reviewed, including amount of the handrub agent to be used and the recommended duration of contact. Manufacturer directions also stress that the agent should cover all parts of the hand and fingers and the hands should be rubbed until dry.1
ORAL SURGICAL PROCEDURES
Dental hygienists should understand the necessity for specific hand hygiene procedures in practice settings where oral surgical procedures are performed. The CDC defines oral surgical procedures as those that “involve the incision, excision, or reflection of tissue that exposes the normally sterile areas of the oral cavity.”1 Examples include biopsy, periodontal surgery, apical surgery, implant surgery, and surgical extractions of teeth. Oral surgical procedures present an opportunity for entry of microorganisms into the vascular system and other normally sterile areas of the oral cavity. Consequently, there is an inherent risk for localized or systemic infection.1 Because of this risk, the CDC provides specific hand hygiene recommendations for oral surgical procedures (Table 3).
The purpose of surgical hand antisepsis is to eliminate transient flora and reduce resident flora on the hands. The goal of surgical hand antisepsis is to reduce the risk of introducing microorganisms into sterile tissues and to prevent health care-associated infections.
Antiseptic agents used for surgical hand antisepsis should substantially reduce microorganisms on intact skin. Other recommended selection criteria include that the product be nonirritating, have a broad spectrum of activity, be fast-acting, and have a persistent effect,5 ie, extended antimicrobial activity that prevents or inhibits survival of microorganisms after the product is applied. The long lasting effect is critical because microorganisms can colonize on hands in the moist environment underneath gloves.
Even though alcohol handrubs have a rapid germicidal effect on the skin, the CDC recommends using alcohol handrub products that also contain additional antiseptics such as chlorhexidine, quaternary ammonium compounds, octenidine, or triclosan to achieve persistent activity.5 Factors that can influence the effectiveness of the surgical hand antisepsis, in addition to the choice of antiseptic agent, include duration and technique of scrubbing, as well as condition of the hands, and techniques used for drying and gloving. The CDC’s 2002 guideline on hand hygiene in health care settings provides more complete information.5
In order to achieve optimal hand antisepsis, selecting an antiseptic agent that contains the optimal concentration of the active ingredients is key. The Food and Drug Administration (FDA) clears antiseptic hand hygiene products intended for use in health care settings. Therefore, health care facilities personnel should select antiseptic hand hygiene products that have FDA approval as health care antiseptic products.5
REFERENCES
- Kohn WG, Collins AS , Cleveland JL, Harte JA, Eklund KJ, Malvitz DM, Centers for Disease Control and Prevention (CDC). Guidelines for infection control in dental health-care settings—2003. MMWR Recomm Rep. 2003;19;52(RR-17):1-61.
- Institute of Medicine. To Err Is Human: Building a Safer Health System. Available at www.iom.edu/CMS/8089/5575.aspx. Accessed January 2, 2007.
- Semmelweis I. Etiology, Concept, and Prophylaxis of Childbed Fever. Carter KC, ed. 1st ed. Madison, Wis: The University of Wisconsin Press; 1983.
- Rotter M. Hand washing and hand disinfection. In: Mayhall CG, ed. Hospital Epidemiology and Infection Control. 2nd ed. Philadelphia: Lippincott Williams & Wilkins; 1999.
- Boyce JM, Pittet D, Healthcare Infection Control Practices Advisory Committee, HICPAC/SHEA/APIC/IDSA Hand Hygiene Task Force. Guideline for hand hygiene in health-care settings. MMWR Recomm Rep. 2002;51(RR-16):1-45, quiz CE1-4.
- WHO World Alliance for Patient Safety: WHO Guidelines on Hand Hygiene in Health Care (Advanced Draft) April 2006. Available at: www.who.int/patientsafety/information_centre/ghhad_download/en/index.html. Accessed December 20, 2006.
From Dimensions of Dental Hygiene. January 2007;5(1): 20, 22, 24.

