Technology Transformation
Advancements in technology have greatly impacted the provision of dental hygiene services for both patients and clinicians.
Techniques and technologies in dental hygiene practice have significantly advanced since the profession began in the early 1900s. Improvements are vast—ranging from design developments in hand instruments to new techniques in dental radiography. These advancements have changed the way dental hygiene is practiced, and they offer many benefits to both patients and practitioners. As we celebrate this evolution and fondly look back on our history, dental hygienists need to remember that staying up to date on these advancements and remaining open to change are key to best practices. While it’s impossible to list all of the technological advances in dental hygiene practice over the past 100 years, below are a few that have had significant impact.

TOOTHBRUSH EVOLUTION
The toothbrush—one of the oldest oral care devices still used today—was first introduced by the Egyptians and Babylonians. They brushed with a “chew stick,” which consisted of chewing on one end of a Salvadora persica branch until wood fibers formed a brush, which was believed to have antiseptic properties. Later, the Chinese invented the first bristle toothbrush in the late 15th century using hairs from the Siberian wild boar and attaching them to bamboo sticks.
 This brush made its way to Europe, but was rough on gingiva and prone to bacterial growth, which led to the use of horsehair instead of boar’s hair. Some Europeans used a cloth or sponge coated in sulfur oils and salt solutions, otherwise known as “the Greek method,” as their primary toothbrushing method.1
This brush made its way to Europe, but was rough on gingiva and prone to bacterial growth, which led to the use of horsehair instead of boar’s hair. Some Europeans used a cloth or sponge coated in sulfur oils and salt solutions, otherwise known as “the Greek method,” as their primary toothbrushing method.1
The first modern toothbrush is attributed to an Englishman, William Addis, in 1780, who is said to have created it with bristles and a bone from his dinner while he was serving time in prison. After his release, Addis began to manufacture the brushes using hair and cow bones. Celluloid toothbrush handles were introduced during World War I, and nylon bristles replaced animal hair in 1938. Nylon filament brushes were advantageous for many reasons, including decreased production cost and better brush design and texture variability. After World War II, American soldiers returned to the United States with improved oral hygiene from stringent brushing habits overseas. Although boar hair toothbrushes still account for 10% of toothbrushes produced around the world today, more advanced designs have evolved to meet specific needs, including the invention of the electric toothbrush in 1960.1
Currently, power brushes are available with sonic or oscillating technology and features such as pressure sensors to alert patients when brushing too hard, reminders to replace brush heads, timers that signal how long to brush in each quadrant, and the ability to select various brushing modes. Several researchers have demonstrated that power toothbrushes reduce plaque and gingivitis more effectively than manual toothbrushes; however, some clinical trials have shown that manual toothbrushing is just as efficient as power brushes when used correctly.2,3 For plaque and gingivitis reduction, the greatest advantage of the power toothbrush is the built-in timer because the majority of patients do not brush long enough. Dental hygienists should review proper brushing techniques with patients and consider recommending a power toothbrush to encourage patients to brush for the appropriate amount of time to optimally reduce plaque and the risk of gingivitis.
![]() INFECTION CONTROL
INFECTION CONTROL
One of the most significant advancements over the past 100 years of dental hygiene is the emphasis on diminishing the spread of infection. In the 1980s, universal infection control precautions solely focused on protection against the human immunodeficiency virus (HIV), hepatitis B, and hepatitis C. With the introduction of new infectious viruses and the broadening of patient populations seen in dental operatories, it is more important than ever for dental hygienists to strictly adhere to infection control standards for their own protection, as well as their patients’. Today, many patients are immunocompromised and more susceptible to infections.4 In 2011, the presence of Legionella pneumophila in the dental waterlines of an Italian dental practice was deemed responsible for the death of an 82-year-old woman who had no other medical conditions.5 The US Centers for Disease Control and Prevention (CDC) guidelines state that dental waterlines must meet the Environmental Protection Agency (EPA)6 drinking water standard of <500 CFU/mL, and recommend dental practices monitor water quality and provide chemical treatments to treat the waterlines.6,7 A variety of products is available for use in dental unit waterlines, such as daily tablets that are placed directly into water reservoirs and treatment “straws” that fit in place of the water pickup tube and can last for up to 1 year. Dental hygienists are well-equipped to monitor dental unit waterlines in clinical practice.
Regardless of practice setting, all dental hygienists need to remain abreast of the most current CDC infection control guidelines,6 which were updated in 2003. These guidelines also address personal protective equipment (protective eyewear, masks, and gloves). Research on three types of face masks found that a particulate respirator mask was most efficient (94% to 98%) in reducing airborne contaminants in the dental office and molded surgical masks reduced contaminants at 90% to 92%, while tie-on surgical masks8 reduced contaminants by 85% to 88%.
![]() ADVANCEMENTS IN HANDPIECES AND PROPHYLAXIS
ADVANCEMENTS IN HANDPIECES AND PROPHYLAXIS
In 1997, the American Dental Hygienists’ Association (ADHA) advocated selective polishing or the practice of polishing only tooth structures with stain.9 Subsequently, a position paper by ADHA was approved in 1998 stating that “the oral prophylaxis should consist of supragingival and subgingival removal of plaque, calculus, and stain.”10 Polishing all tooth surfaces to remove plaque and stain has long been a part of the prophylaxis in clinical dental hygiene care, but the safety of the technique was questioned when a study showed that polishing with a pumice-water slurry removed enamel.11 However, this study was problematic due to a small sample size and undisclosed variables. Therefore, in 2012, the selective polishing approach12 was replaced with essential selective polishing. This technique allows for the polishing of all teeth but stipulates that clinicians must choose the best cleaning or polishing agent for individual patient needs.13 The least abrasive option necessary to reduce stain should be implemented to protect tooth surfaces. Patients will undergo polishing procedures approximately 150 times in their lifetime, so it’s imperative that dental hygienists choose the cleaning or polishing agent carefully.9
New properties have been added to prophy pastes including perlite, amorphous calcium phosphate, casein phosphopeptide-amorphous calcium phosphate, and calcium sodium phosphosilicate. These new additives are designed to break down under pressure, thus reducing abrasiveness; remineralize incipient caries lesions within enamel; and decrease hypersensitivity. Further study is needed to support these claims.14

DIGITAL DENTAL RADIOGRAPHY
Radiography has seen immense change over the past 100 years as the trend has moved away from film toward digital imaging. In digital radiography, the intraoral and extraoral images are acquired from image receptors either directly through charge coupled devices and complementary metal oxide semiconductor sensor technology, or indirectly through photostimulable phosphor plates (PSPs). While digital imaging does have some limitations, its advantages outweigh the disadvantages, providing significant benefits in clinical practice.15 For example, digital radiography decreases radiation exposure up to 50% compared to E-speed film.16
Improvements have been made to direct digital sensors to increase patient comfort, including the design of sensors with contoured edges, which can also reduce the need for retakes, thus decreasing patients’ exposure to radiation. Clinicians should strictly adhere to the American Dental Association’s (ADA) and the federal Food and Drug Administration’s (FDA) recently updated “Recommendations for Prescribing Dental Radiographs,”17 which recommend that radiographic examinations be based on patient age, dental developmental stage, and individual risk factors for disease, to keep the exposure to ionizing radiation from dental images as low as reasonably achievable.
Technology advancements have led to the introduction of portable, handheld X-ray tube head devices, which are available for the exposure of all three types of image receptors: film, sensors, and PSPs. These devices are ideal for use by dental forensic teams during post-mortem identification and comparison of antemortem dental images.18 In addition, handheld X-ray devices can be used to take intraoral radiographs in community-based settings, such as long-term care facilities and locations where access to care is problematic.
Manufacturers of dental X-ray units have improved the generators responsible for radiation output by using direct current (DC) as opposed to alternating current, or typical household current. Radiology units equipped with DC create consistent X-ray energy better suited for use with digital image receptors, thereby reducing the amount of radiation exposure needed to produce an acceptable image.19

ELECTRONIC HEALTH RECORDS
Electronic health records (EHRs) are changing the way dental hygienists document, chart, and treatment plan as more offices make the transition to paperless practice. Computer software programs allow today’s progressive dental office to implement other advancements, such as voice-activated technology for dental and periodontal charting. These systems are fairly easy to use and incorporate into existing computer systems, while providing optimal infection control procedures through the use of a hands-free headset or a foot-operated mouse.
 The presence of computers in every operatory also enables the use of the Internet in clinical practice. This allows dental hygienists to easily look up patient medications, obtain contact information of other health care providers for consultation, and email digital radiographic images to specialists when referral is necessary.
The presence of computers in every operatory also enables the use of the Internet in clinical practice. This allows dental hygienists to easily look up patient medications, obtain contact information of other health care providers for consultation, and email digital radiographic images to specialists when referral is necessary.
INSTRUMENTATION
Dental hygiene instruments have progressed from the primitive to the futuristic. New and improved hand instruments are introduced on a regular basis, such as the use of metals and alloys that reduce the need for sharpening; advancements in design to improve access to deep periodontal pockets, furcation involvements, and posterior deposits; and the addition of lightweight handles to improve ergonomics.
Instruments are also available that are safe to use on titanium implants.20 The introduction of the ultrasonic scaler is a significant innovation. Ultrasonic instrumentation debrides plaque and calculus when the tip is appropriately adapted subgingivally. Originally, ultrasonic inserts or tips (UITs) consisted of three designs: universal, triple bend, and beavertail. Today, UITs come in a wide variety of designs manufactured for adaption to all surfaces within the oral cavity, such as curved, thin designs with varying lengths, and ball-tipped UITs ideal for furcation involvement.
The dental endoscope—a very small magnifying camera attached to the end of a probe—allows clinicians to visualize subgingival calculus and plaque in real time. The ability to see into the pocket helps clinicians ensure they are removing all deposits, and decreases the risk of common instrumentation mistakes, such as failing to use continual, overlapping strokes when instrumenting with an ultrasonic scaler.
ERGONOMICS
The past 100 years have brought about many ergonomic innovations in the dental hygiene profession. Advancements in lighting, magnification, seating, and instruments have helped reduce the risk of musculoskeletal injuries from the repetitive motions common in dental hygiene and oral care.
Coaxial illumination (headlights) and lighting fixed to magnification eyewear (loupes) can be particularly advantageous compared to traditional overhead lighting because the light source is directly in the clinician’s line of vision, reducing shadows. Headlights support a neutral body position by providing illumination directly to the oral cavity—eliminating the need to bend or reach to adjust overhead lighting. Light emitting diode (LED) technology has replaced older fiber optic, halide, halogen, and xenon headlights, producing less heat and providing longer service life.21 In addition, dental hygiene prophy handpiece manufacturers now offer more lightweight, cordless products that may offer ergonomic benefits.
Instrument design and width are critical to reducing injuries caused by repeated scaling motions, such as carpal tunnel syndrome. A study assessed instrument shape and design on muscle activity using electromyography in dentists and dental hygienists. Results indicated that the instrument with the largest diameter (10 mm) and more tapered design required the least amount of pressure.22

USE OF ANTIBIOTICS AND ANTIMICROBIALS
The use of antibiotics and antimicrobials has significantly increased in dental hygiene practice—from therapeutic mouthrinses and toothpastes to local drug delivery systems. Both antimicrobials and antibiotics can play a large role in the reduction of oral disease.
Antimicrobial mouthrinses contain ingredients designed to kill and disrupt biofilm leading to reductions in plaque and gingivitis. Chlorine dioxide, chlorhexidine, essential oils (thymol, menthol, eucolyptol, and methyl salicylate), quaternary ammonium compounds, cetylpyridinium chloride (CPC), benzethonium chloride, and domiphen bromide, as well as stannous fluoride, have been shown to exhibit antimicrobial effects.23 Chlorhexidine remains the gold standard for its antiplaque and antigingivitis properties.23 In vitro research on the substantive action of antimicrobial mouthrinses and toothpastes concluded that plaque biofilm left behind after brushing held the antimicrobial effects from the slurry of toothpaste and rinsing, which enabled prolonged antimicrobial effects of newly-formed biofilm.23 Patients who need further assistance in plaque management can benefit different from the addition of antimicrobial toothpastes and mouthrinses to existing self-care routines.
Locally applied antimicrobials/antibiotics (LAAs) should be reserved for patients who are unresponsive to debridement and self-care therapies. Introduced in the 1980s, three agents are used presently in LAAs: minocycline, doxycycline, and chlorhexidine. In some cases, LAAs used in unresponsive periodontal pockets with bleeding can improve tissue attachment and help patients avoid periodontal surgery.

WHAT THE FUTURE HOLDS
While the profession of dental hygiene has vastly progressed, the next 100 years will also look very different. Universal licensure and self-regulation practices for all states could be achieved, allowing dental hygienists to work independently. Mid-level providers with the education and experience to provide diagnostic, preventive, restorative, and therapeutic services across the US could significantly help solve the growing access-to-care problem. More dental hygienists with advanced degrees will be necessary to meet the needs of growth in the profession. To date, there are shortages of qualified dental hygiene educators able to lead existing programs, and the number of dental hygiene schools continues to grow across the country. A great deal of knowledge is provided by scientific research, and further study is needed to better understand caries, periodontal diseases, inflammation, and oral cancer. The future of oral health care lies in what science will uncover in these areas. Dental hygienists must be prepared to advance the profession and meet the needs of a variety of patient populations.
REFERENCES
- Sutter, E. The evolution of the toothbrush. Available at: www.dentaltribune.com/ articles/ specialities/dental_ hygiene/4578_ the_ evoution_ of_ the_ toothbrush.html. Accessed March 13, 2013.
- Cronin M, Dembling W, Warren PR, King D. A 3-month clinical investigation comparing thesafety and efficacy of a novel electric toothbrush (Braun Oral-B 3D Plaque Remover) with amanual toothbrush. Am J Dent. 1998;11:S17-21.
- Parizi MT, Mohammadi TM, Afshar SK, Hajizamani A, Tayebi M. Efficacy of an electric toothbrushon plaque control compared to two manual toothbrushes. Int Dent J. 2011;61:131–135.
- Lux J. Infection control practice guidelines in dental hygiene—part 1. Canadian Journal ofDental Hygiene. 2008;42(2):63–103.
- Ricci ML, Fontana S, Pinci F, et al. Pneumonia associated with a dental unit waterline. Lancet.2012;379:684.
- Kohn WG, Collins AS, Cleveland JL, et al. Guidelines for infection control in dental health-caresettings—2003. MMWR Recomm Rep. 2003;52:1–66.
- Organization for Safety, Asepsis, and Prevention. Dental unit waterlines. Available atwww.osap.org/?page=Issues_DUWL. Accessed March 13, 2013.
- Checchi L, Montevecchi M, Moreschi A, Graziosi F, Taddei P, Violante FS. Efficacy of three facemasks in preventing inhalation of airborne contaminants in dental practice. J Am Dent Assoc.2005;136:877–882.
- Pence SD, Chambers DA, Van Tets IG, Wold RC and Pfeiffer DC. Repetitive coronal polishing yields minimal enamel loss. J Dent Hyg. 2011;85:348–357.
- American Dental Hygienists’ Association. Position Paper on the Oral Prophylaxis. Available at: www.adha.org/resources-docs/7115_Prophylaxis_Postion_Paper.pdf. Accessed March 13, 2013.
- Vrbic V, Brudevold F, McCann HG. Acquisition of fluoride by enamel from fluoride pumice paste. J Dent Res. 1956;35:420.
- Barnes CM. Polishing. In: Wilkins EM. Clinical Practice of the Dental Hygienist. 11th ed. Philadelphia: Lippincott Williams and Wilkins; 2012.
- Barnes CM. Shining a new light on selective polishing. Dimensions of Dental Hygiene. 2012;10(3):42–44.
- Barnes CM. The science of polishing. Dimensions of Dental Hygiene. 2009;7(11):18–20.
- Bruhn AM, Sokolik TL. Dental X-rays go digital. Dimensions of Dental Hygiene. 2011;9(6):40–44
- Berkhout WE, Beuger DA, Sanderink GC, van der Stelt PF. The dynamic range of digital radiographic systems: dose reduction or risk of overexposure? Dentomaxillofac Radiol. 2004;33:1–5.
- American Dental Association Council on Scientific Affairs and U.S. Department of Health and Human Services. Dental Radiographic Examinations: Recommendations for Patient Selection andLimiting Radiation Exposure. 2012. Available at: www.ada.org/sections/professionalResources/pdfs/Dental_Radiographic_Examinations_2012.pdf. Accessed March 13, 2013.
- Erdman KA, Colon JE. Dental detectives. Dimensions of Dental Hygiene. 2012;10(11):50–53.
- United States Air Force Dental Evaluation and Consultation Service. Synopsis of Intra-Oral X-ray Units. Available at: www.airforce medicine .afms.mil/ idc/ groups/ public/ documents/ afms/ ctb_108739.pdf. Accessed March 13, 2013.
- Pattison A. Innovation in hand instruments. Dimensions of Dental Hygiene. 2012;10(5):44–49.
- United States Air Force Dental Evaluation and Consultation Service. Synopsis of Headlights for Dentistry and Surgery. Available at: www.airforcemedicine.afms.mil/ idc/ groups/ public/ documents/afms/ ctb_109457.pdf. Accessed March 13, 2013.
- Dong H, Loomer P, Barr A, LaRoche C, Young E, Rempel D. The effect of tool handle shape on hand muscle load and pinch force in a simulated dental scaling task. Appl Ergon. 2007;38:525–531.
- Otten MP, Busscher HJ, van der Mei HC, van Hoogmoed CG, Abbas F. Acute and substantive action of antimicrobial toothpastes and mouthrinses on oral biofilm in vitro. Eur J Oral Sci.2011;119:151–155.
From Dimensions of Dental Hygiene. Centennial Celebration of Dental Hygiene 1913-2013; 32, 34, 36, 38, 40, 42, 44.

 INFECTION CONTROL
INFECTION CONTROL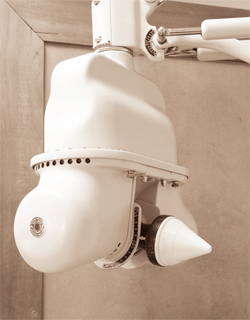 ADVANCEMENTS IN HANDPIECES AND PROPHYLAXIS
ADVANCEMENTS IN HANDPIECES AND PROPHYLAXIS