Synergistic Approach
Fluoride therapy, in addition to adjunctive over-the-counter remedies, can help patients with xerostomia relieve the dry mouth symptoms and reduce their risk of decay.
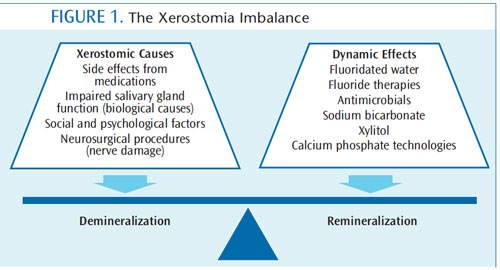
Xerostomia is a multifactorial oral condition characterized by loss of salivary function due to medication use,1 biological causes, social and psychological factors,2 or neurosurgical procedures.3 It is accompanied by a change in the normal composition of saliva. The symptoms of this condition, often referred to as dry mouth, can adversely affect quality of life and significantly increase the risk of oral disease.2
Oral health professionals—especially dental hygienists—should use a multidimensional, synergistic approach in order to effectively address xerostomia.
DEMINERALIZATION AND XEROSTOMIA
Enamel demineralization occurs when the oral pH rapidly decreases from a neutral pH to a pH of less than 5.5. This decrease is caused by the provision of sucrose to acidogenic bacteria in biofilm, and results in the demineralization of the subsurface enamel by the movement of the calcium and phosphate ions toward the enamel’s outer surface. This causes the calcium and phosphate ions to move from the subsurface enamel into the bacterial biofilm overlying the tooth surface. Although dental plaque is saturated with calcium and phosphate ions, the rapid increase in hydrogen ions provides a fortress for enamel demineralization.3
This drop in plaque pH, however, is secondary to the action of fermentable dietary carbohydrates. Following a cariogenic acid challenge, the resting pH of the bacterial biofilm is restored and the influx of the hydrogen ions is no longer a critical factor.4
ENHANCING REMINERALIZATION
The remineralization process begins when the oral pH of plaque rises above 5.5, releasing calcium and phosphate from the surrounding dental plaque near the tooth-plaque interface.1 High levels of calcium and phosphate ions occlude enamel pores to the demineralized enamel.3 Remineralization is defined as the process whereby calcium and phosphate ions are supplied from a source external to the tooth to promote calcium and phosphate ion deposition into the hydroxyapatite pores of demineralized enamel—ultimately producing a net mineral gain.4
Calcium and phosphate derived from saliva are necessary for effective daily remineralization and maintenance of the enamel surface after an acidogenic challenge. The ability of saliva to remineralize enamel was recognized more than 40 years ago, when it was demonstrated that some white-spot lesions reverted to arrested enamel and remained stable.3 Initially, patients may be unaware of a reduction in their salivary flow. As such, oral health professionals should be prepared to spot the first signs of xerostomia so strategies can be implemented to address potential complications and alleviate symptoms.2
THE FLUORIDE FACTOR
Saliva is a major carrier of topical fluoride. Fluoridated water supplies and fluoride toothpastes are the most common vehicles of fluoride deposition in the United States. Patients with xerostomia are more susceptible to root caries and greatly benefit from fluoride exposure.5 Many patients drink bottled water, replacing tap water partially or completely as a source of drinking water. Although some brands of bottled water marketed in the US contain an optimal concentration of fluoride (approximately 1.0 ppm), most contain ?0.3 ppm fluoride. Current US Food and Drug Administration regulations require that fluoride be listed on the label only if it is added during processing. Ideally, patients with xerostomia should know the fluoride concentration of their primary source of drinking water. This information should then be used as the basis for all individual and professional decisions made regarding the use of adjunctive over-the-counter (OTC) fluoride management strategies.5
MANAGEMENT STRATEGIES
The daily use of fluoride combined with meticulous oral hygiene and a noncariogenic diet must be recommended in order to promote remineralization in all patients—especially those who experience dry mouth. In addition to nutritional counseling, the dental hygienist should be knowledgeable about specific adjunctive OTC products and therapies to help alleviate discomfort caused by xerostomia.
The most common medium for topical fluoride delivery is dentifrice. OTC fluoride toothpastes contain sodium fluoride, stannous fluoride, or sodium monofluorophosphate. Fluoride’s main role in caries development is to reduce demineralization and enhance remineralization.6 Fluoride, however, does not exert a significant antimicrobial effect on dental plaque.7 Thus, substances that act on bacterial metabolism—inhibiting or neutralizing the acids produced—may increase the anticariogenic effect of fluoride.8
Stannous fluoride offers additional antibacterial properties against plaque, gingivitis, and breath malodor.9 The results of two clinical trials that examined the efficacy of stannous fluoride toothpaste found that it reduced gingivitis by 14% to 20% and gingival bleeding by 20% to 33%.10,11 Toothpaste that contains the antibacterial agent triclosan may also be helpful for patients with xerostomia. An antibacterial, antifungal, and antiviral substance, triclosan is effective against Gram-positive and Gram-negative bacteria.12 Ciancio13 conducted a systematic literature review on the effects of triclosan copolymer/fluoride dentifrice and found that significant evidence was available to support its effectiveness in improving supragingival plaque control; encouraging gingival health; decreasing the likelihood of gingivitis developing into periodontitis; stopping the progression of periodontitis; preventing supragingival calculus; and reducing oral malodor.
Sodium bicarbonate (baking soda), due to its alkaline and buffering properties, may neutralize the acids produced by bacteria in dental plaque during sugar consumption, and enhance the effect of fluoride dentifrice. Sodium bicarbonate has also demonstrated bacteriocidal abilities, specifically against periodontal microorganisms. In a study by Rams et al,14 5-minute exposure to sodium bicarbonate quickly immobilized spirochetes and motile rods. Gram-positive cocci bacteria, such as Streptococcus mutans, were also shown to be susceptible against 4% sodium bicarbonate.8 Additionally, regular use of a dentifrice containing 65% sodium bicarbonate lowered the level of S. mutans in saliva.15 Another beneficial agent for patients experiencing dry mouth is xylitol. This naturally occurring, noncariogenic sweetener promotes remineralization by increasing salivary flow,16 and inhibits bacterial growth and metabolism in the plaque biofilm.17
Fluoride’s ability to promote remineralization is limited by the availability of calcium and phosphate ions in the saliva. Hence, the absence of calcium and phosphate ions in patients with xerostomia may be a limiting factor for fluoride retention and net remineralization results. For every two fluoride ions, 10 calcium ions and six phosphate ions are required to form one unit cell of fluorapatite.18 Calcium phosphate technologies, including amorphous calcium phosphate, casein phosphopeptide-amorphous calcium phosphate (Recaldent®), calcium sodium phosphosilicate (NovaMin®), and tricalcium phosphate, can supply additional calcium and phosphate ions, making them readily available in the saliva. These technologies may provide additional protection against tooth decay for patients with xerostomia. While clinical evidence suggests calcium phosphate agents complement the clinical effectiveness of fluoride,19 fluoride therapy continues to remain the cornerstone of the noninvasive management of noncavitated caries lesions.
For relief of dry mouth symptoms, patients often turn to gum, mints, or lozenges that contain sugar and acids. This may prolong the oral cavity’s exposure to fermentable carbohydrates while lowering the pH—increasing caries risk. Patients should be advised to instead chew sugar-free gum with xylitol or a calcium phosphate agent. Chewing gum has been shown to increase saliva production in patients with xerostomia.20 Patients may also want to try saliva substitutes, which are available as mouthrinses, sprays, swabs, tablets, gels, and patches.
CONCLUSION
Dental hygienists must be aware of the adverse effects of xerostomia on patients’ oral health, including increased risk of caries and reduced quality of life. Patients who experience this condition face challenges to maintaining satisfactory oral health, requiring dental professionals to create patient-focused prophylactic protocols and management strategies (Figure 1). Frequent dental hygiene appointments and thorough daily self-care are critical to helping these patients maintain their oral health. At-home therapies can also help patients address the negative effective effects of xerostomia while promoting remineralization.
REFERENCES
- 1. Kelly HM, Deasy PB, Busquet M, Torrance AA.Bioadhesive, rheological, lubricant and other aspects of an oral gel formulation intended for the treatment of xerostomia. Int J Pharm. 2004;278: 391–406.
- Guggenheimer J, Moore PA. Xerostomia: etiology,recognition and treatment. J Am Dent Assoc. 2003;134:61–69.
- García-Godoy F, Hicks MJ. Maintaining the integrity of the enamel surface: the role of dental biofilm, saliva and preventive agents in enamel demineralization and remineralization. J Am Dent Assoc. 2008;139:25S–34S.
- Cochrane NJ, Cai F, Hug NL, Burrow MF, ReynoldsEC. New approaches to enhanced remineralization of tooth enamel. J Dent Res. 2010;89:1187–1197.
- Recommendations for using fluoride to preven tand control dental caries in the United States. Centers for Disease Control and Prevention. MMWR Recomm Rep. 2001;50:1–42.
- Dawes C, Weatherell JA. Kinetics of fluoride in theoral fluids. J Dent Res.1990;69:682–683. Emilson CG. Potential efficacy of chlorhexidine against mutans streptococci and human dental caries. J Dent Res. 1992;73:682–691.
- Barnes CM. An evidence-based review of sodium bicarbonate as a dentifrice agent. Compend Contin Educ Dent. 1999;6(3):3–11.
- Sensabaugh C, Sagal ME. Stannous fluoride dentifrice with sodium hexametaphosphate: review of laboratory, clinical and practice-based data. J DentHyg. 2009;83:70–78.
- Chen X, He T, Sun L, Zhang Y, Feng X. A randomized cross-over clinical trial to evaluate the effect of a 0.454% stannous fluoride dentifrice on the reduction of oral malodor. Am J Dent. 2010;23:175–178.
- Beiswanger BB, Doyle PM, Jackson RD, et al. The clinical effect of dentifrices containing stabilized stannous fluoride on plaque formation and gingivitis—a six-month study with ad libitum brushing. J Clin Dent. 1995;6:46–53.
- Hodges K. Reduce the bacterial load. Dimensions of Dental Hygiene. 2012;10(6):52–55.
- Ciancio SG. Controlling biofilm with evidence based dentifrices. Compend Contin Educ Dent. 2011;32:70–76.
- Rams TE, Keyes PH, Wright WE, Howard SA. Long term effects of microbiologically modulated periodontal therapy on advanced adult periodontitis.J Am Dent Assoc. 1985;111:429–441.
- Legier-Vargas K, Mundorff-Shrestha SA,Featherstone JD, Gwinner LM. Effects of sodium bicarbonate dentifrices on the levels of cariogenic bacteria in human saliva. Caries Res. 1995;29:143–147.
- Atkinson JC, Grisius M, Massey W. Salivary hypofunction and xerostomia: diagnosis and treatment. Dent Clin North Am. 2005;49:309–326.
- Ritter AV, Bader JD, Leo MC, et al. Tooth-surface specific effects of xylitol: randomized trial results. J Dent Res. 2013;92;512–517.
- Reynolds EC, Cai F, Cochrane NJ, et al. Fluoride and case in phospho peptide-amorphous calcium phosphate. J Dent Res. 2008;87:344–348.
- Reynolds EC. Calcium phosphate-based remineralization systems: scientific evidence? Aust Dent J. 2008;53:268–273.
- Karami Nogourani M, Janghorbani M, KowsariIsfahan R, Hosseini Beheshti M. Effects of chewing different flavored gums on salivary flow rate and pH.Int J Dent. 2012;2012:1–4.
From Dimensions of Dental Hygiene. November 2013;11(11):43–45.

