 SELVANEGRA/ISTOCK/GETTY IMAGES PLUS
SELVANEGRA/ISTOCK/GETTY IMAGES PLUS
Strategies for Safe and Effective Treatment of Patients With Alzheimer Disease
Oral health professionals need to be prepared to treat individuals with varying stages of this neurodegenerative disorder.
This course was published in the August 2020 issue and expires August 2023. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Explain how to best assess patients with Alzheimer disease (AD) and provide patient communication.
- Discuss strategies for treating this patient population.
- Identify ways to help patients with AD and their caregivers perform effective oral hygiene.
Alzheimer disease (AD) is a progressive neurodegenerative disorder that causes cognition impairment and memory loss, affecting activities of daily living.1 In the United States, an estimated 4.5 million people have AD and this figure is expected to reach 14 million by 2050.2 The population affected by AD across the world is projected to increase to 81.1 million by 2040.3,4 Because patients with AD experience a deterioration of their mental functions, patients need more help with their activities of daily living, including oral hygiene, as their AD progresses. Studies have found that individuals with AD often experience poor oral health.5,6 As advanced age is a risk factor for AD and the number of older adults in the US continues to rise, oral health professionals must be knowledgeable about treating patients with this neurodegenerative disorder.7
ASSESSMENT
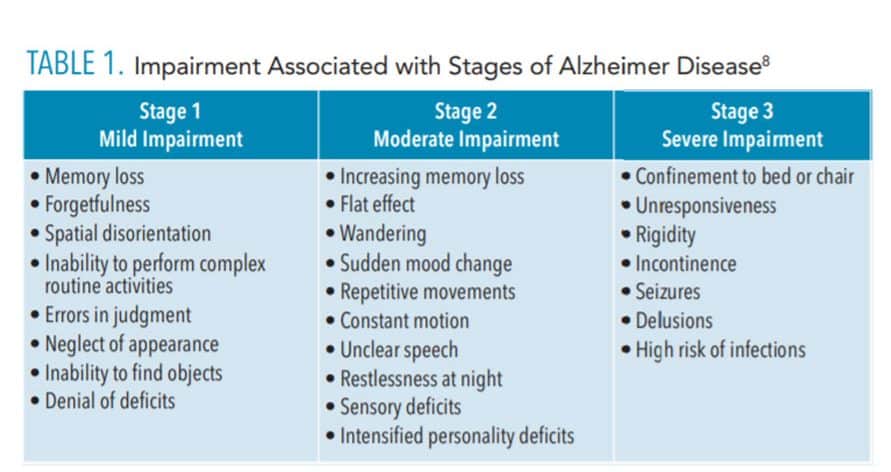
Patients with early or mild stages of AD are still able to perform most of their own oral hygiene care (Table 1).8 Because AD is a progressive disease, oral health professionals should assess patients with AD at every visit to evaluate their ability to perform self-care. Talking with both caregivers and patients is recommended. Caregivers should be contacted 1 week to 2 weeks in advance of the appointment to update patients’ health, dental, and pharmacologic histories.9 A comprehensive examination, including radiographs, should be conducted on each patient with AD. The earlier the screening for oral conditions, the more effective the application of preventive procedures can be. All of these efforts will help to prevent the deterioration of oral health among this population.10
APPOINTMENT
When a patient is diagnosed with AD or dementia, caregivers should be advised to schedule regular appointments with the patient’s dentist and dental hygienist. Appointments should be scheduled when the care setting is the least crowded. The same treatment area and the same oral health professional should be used at every appointment; this bit of familiarity may decrease the patient’s agitation and increase cooperation.4
Patients with AD should maintain regular dental checkups every 6 months or less (based on each patient’s stage of AD and needs) for continued care, in order to maintain oral health and to prevent the progression of periodontal diseases.10,11 Caregivers may have difficulty getting patients with AD to appointments on time; providers should be prepared for early or late arrivals. In the event of difficulty, the visit should be rescheduled; forcing a patient to receive care may lead to aggressive behaviors.11 Some patients may need anti-anxiety medications to control their stress and/or their challenging behaviors.10
COMMUNICATION
Communicating with patients with AD can be challenging, and oral health professionals need to demonstrate empathy.12 When communicating verbally, simple, short sentences should be used as well as a soft tone of voice. In addition, patients with AD may face difficulty in describing their feelings and oral symptoms.13,14 Written treatment plans and self-care instructions can be given both to patients and caregivers in order to increase compliance. If information needs to be repeated, the exact original words and manner should be used to avoid any confusion or misunderstanding.12
Patients with AD should be encouraged to express their ideas and feelings. For example, asking a patient about hobbies, favorite sports teams, or family may facilitate care and compliance, which helps foster inclusion in the decision-making process.15 However, the caregiver should be consulted before the patient with AD is included in the decision-making process.15
Nonverbal communication, such as direct eye contact, empathetic facial expressions, and supportive body postures, may assist in communicating with patients with AD. Patting the patient’s shoulder and smiling can help to decrease anxiety and increase cooperation. Demonstrating the procedures to be performed can alleviate fear and encourage cooperation.16 Oral health professionals should treat patients with AD with the utmost compassion and respect.17
Even though caregivers should be involved in decision making, talking about patients as if they are not in the room, or treating patients as if they are children, should be avoided.11 The presence of caregivers in the treatment room is an asset to both patients and providers, as they can reassure patients and help oral health professionals understand patients’ speech and body language. Dental professionals play a crucial role in ensuring that family members or caregivers know how to perform oral hygiene tasks with/for the patient and ensuring they are willing to do so.11
TREATMENT CONSIDERATIONS
Dental treatment, behavioral management, and oral care for individuals with AD is dependent on the stage and severity of the AD, and caregivers or family members must be involved.18 Appointments with patients who have early stage AD may proceed normally. However, they may need to be helped into the dental chair; the clinician may hold the patient’s hand and softly and slowly speak to guide him or her to the correct position. If the patient does not like the supine position, he/she should not be fully reclined, in order to preserve his or her feelings of control and safety.
Patients in the more severe stages of AD can be extremely uncooperative. Performing their oral screening or treatment can be challenging; therefore, sedation or general anesthesia is commonly recommended. Informed consent should be obtained if restraints are used.19 Sedation enables dental professionals to treat patients effectively and to perform all of the required dental treatments in one day; therefore, sedation saves time and the cost of visiting the dental clinic multiple times.14,20–22
Dental disease prevention should occur as early as possible in the AD diagnosis, in order to prevent the need for more complex procedures when the patient is in the later, more difficult, stages of AD. If patients become unable to make their own health decisions, a healthcare decision maker with a power of attorney will be appointed. This legal arrangement must be documented in the patient record.17
Some medications are associated with orthostatic hypotension and increased fall risk. As such, the back of the chair should be raised slowly after completing treatment, permitting the patient to sit upright for about 5 minutes before he or she leaves the chair.23
ORAL CONSIDERATIONS
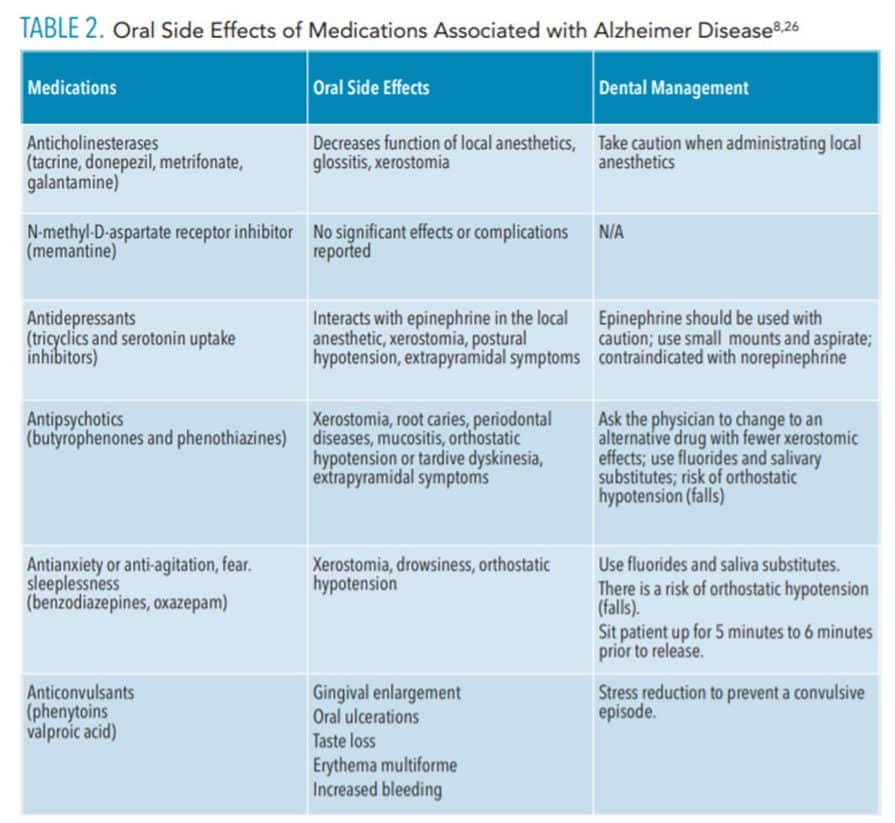
Xerostomia is a side effect of many of the medications used in the treatment of AD and may result in increased plaque biofilm and calculus, oral malodor, chapped lips, and higher risk for periodontal diseases and dental caries.24 Over-the-counter mucosal lubricants, saliva substitutes, and saliva stimulants with xylitol may help patients with AD manage dry mouth. Additionally, medications prescribed to address seizures (eg, phenytoin) or heart disease (eg, nifedipine) may cause drug-influenced gingival enlargement.25 Table 2 lists the oral side effects of medications used to treat AD.8,26
![Oral side effects of medication taken for Alzheimer Disease]() ORAL SELF-CARE
ORAL SELF-CARE
In the early stages of AD, patients may be able to independently perform toothbrushing and interdental cleaning, although some may need to be reminded or supervised during the procedure.27 As the AD progresses, oral healthcare is often neglected. Patients may fail to remember how or why they should perform oral self-care.25 Hence, caregivers must assume responsibility for the patient’s oral care. Oral health professionals should educate both patients and caregivers on effective oral hygiene techniques, products, and devices, based on the stage of AD (Table 1).28 Caregivers may not have the knowledge or skills necessary to provide dental care.29 Supervision of patients with AD is crucial; caregivers must remind patients to perform oral care at least once a day and must make sure they clean and remove their dentures before sleep.10
All patients with AD do not share the same cognition level; some may be able to accomplish a complex task, but unable to complete a simple activity. During the middle stages of AD, the cognition status of the patient deteriorates, and apraxia and apathy lead to a lack of interest in, and a lack of capacity to execute suitable oral hygiene practices.30
Family members/caregivers should be involved in the oral healthcare plan discussion in order to help with any questions patients may have. Demonstrations and hands-on practice are needed to assess mastery.31 Caregivers can post photographs of oral hygiene procedures in the bathroom to remind patients of toothbrushing or interdental cleaning.4
In the late stages of AD, patients become more reliant on caregivers for self-care. Despite the fact that a power toothbrush may be easier for caregivers to use on a patient with AD, the noise and vibration may disturb the patient. Mouthrinses are contraindicated due to swallowing risk. Flossing can be difficult for patients with AD; therefore, the use of an interdental brush is recommended.25 Caregivers should be encouraged to perform oral care at the same time every day, as a routine will facilitate cooperation.4 Caregivers face daily challenges; therefore, it is important to provide positive reinforcement to both patients and caregivers in order to keep them motivated.
Finally, due to the gradual deterioration of their mental capabilities, patients with AD are more at risk for dental diseases than healthy people. As such, patients with AD need special care and treatment in dental clinics. Oral health professionals should remain knowledgeable about effective strategies for treating this patient population.
REFERENCES
- Syrjälä A, Ylöstalo P, Knuuttila M, et al. Dementia and oral health among subjects aged 75 years or older. Gerodontology. 2012;29:36–42.
- Prince MJ, Wu F, Guo Y, et al. The burden of disease in older people and implications for health policy and practice. Lancet. 2015;385:549–562.
- Ferri C, Prince M, Brayne C, et al. Global prevalence of dementia: a Delphi consensus study. Lancet. 2005;366:2112–2117.
- Little JW. Dental Management of the Medically Compromised Patient. 7th ed. St. Louis: Mosby Elsevier; 2008.
- Kumar A, Singh A. A review on Alzheimer’s disease pathophysiology and its management: an update. Pharmacol Rep. 2015;67:195–203.
- Aragón F, Zea-Sevilla MA, Montero J, et al. Oral health in Alzheimer’s disease: a multicenter case-control study. Clin Oral Investig. 2018;22:3061–3070.
- Shay K. The evolving impact of aging American dental practice. J Contemp Dent Pract. 2004;5:101–110.
- Ettinger R. Dental management of patients with Alzheimer’s disease and other dementias. Gerodontology. 2000;17:8–16.
- Chiappelli F, Manfrini E, Edgerton M, Rosenblum M, Cajulis KD, Prolo P. Clinical evidence and evidence-based dental treatment of special populations: Patients with Alzheimer’s disease. J Calif Dent Assoc. 2006;34:439–447.
- Marchini L, Ettinger R, Caprio T, Jucan A. Oral health care for patients with Alzheimer’s disease: an update. Spec Care Dentist. 2019;39:262–273.
- Tolle L. Treating patients with Alzheimer’s disease: considerations for dental hygienists. J Pract Hyg. 2005;14:9–15.
- Byszewski AM, Molnar FJ, Aminzadeh F, Eisner M, Gardezi F, Bassett R. Dementia diagnosis disclosure: a study of patient and caregiver perspectives. Alzheimer Dis Assoc Disord. 2007;2:107–114.
- Chen X, Clark JJ, Naorungroj S. Oral health in nursing home residents with different cognitive statuses. Gerodontology. 2013;30:49–60.
- Kieser J, Jones G, Borlase G, MacFadyen E. Dental treatment of patients with neurodegenerative disease. N Z Dent J. 1999;95:130–134.
- Hirschman KB, Joyce CM, James BD, Xie SX, Karlawish JH. Do Alzheimer’s disease patients want to participate in a treatment decision, and would their caregivers let them? Gerontologist. 2005;45:381–388.
- Baum C, Edwards D. What persons with Alzheimer’s disease can do: a tool for communication about everyday activities. Alzheimer’s Care Q. 2003;4:108–118.
- Sacco D, Frost D. Dental management of patients with stroke or Alzheimer’s disease. Dent Clin North Am. 2006;50:625–633.
- Ocasio NA, Solomowitz BH, Sher MR. Dental management of the patient with Alzheimer’s disease. N Y State Dent J. 2000;66:32.
- DeBiase C, Austin S. Oral health and older adults. J Dent Hyg. 2003;77:125–147.
- Kocaelli H, Yaltirik M, Yargic LI, Özbas H. Alzheimer’s disease and dental management. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;93:521–524.
- So E, Kim HJ, Karm MH, Seo KS, Chang J, Lee JH. A retrospective analysis of outpatient anesthesia management for dental treatment of patients with severe Alzheimer’s disease. J Dent Anesth Pain Med. 2017;17:271–280.
- Caputo AC. Providing deep sedation and general anesthesia for patients with special needs in the dental office‐based setting. Spec Care Dentist. 2009;29:26–30.
- Meloto C, Rizzatti-Barbosa C, Gomes S, Custodio W. Dental practice implications of systemic diseases affecting the elderly: a literature review. Brazil J Oral Sci. 2008;7:1691–1699.
- Kocaelli H, Yaltirik M, Yargic I, Özbas H. Alzheimer’s disease and dental management. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2002;93:521–524.
- Darby ML, Walsh MM. Procedures Manual to Accompany Dental Hygiene: Theory and Practice. 3rd ed. St. Louis: Saunders/Elsevier; 2010.
- Gage TW, Pickett FA. Mosby’s Dental Drug Reference. 7th ed. St. Louis: Mosby; 2006.
- Prajer R. Treating patients with Alzheimer’s disease. Dimensions of Dental Hygiene. 2006;4(9):24.
- Delwel S, Binnekade TT, Perez RS, Hertogh CM, Scherder EJ, Lobbezoo F. Oral hygiene and oral health in older people with dementia: a comprehensive review with focus on oral soft tissues. Clin Oral Investig. 2018;22:93–108.
- Henry R, Wekstein D. Providing dental care for patients diagnosed with Alzheimer’s disease. Dent Clin North Am. 1997;41:915–943.
- Arai K, Sumi Y, Uematsu H, Miura H. Association between dental health behaviors, mental/physical function and self-feeding ability among the elderly: a cross-sectional survey. Gerodontology. 2003;20:78–83.
- Wilson R, Rochon E, Mihailidis A, Leonard C. Quantitative analysis of formal caregivers’ use of communication strategies while assisting individuals with moderate and severe Alzheimer’s disease during oral care. J Commun Disord. 2013;46:249–263.
From Dimensions of Dental Hygiene. July/August 2020;18(7):32-35.