 MICHAEL L. MATSUDA, DDS
MICHAEL L. MATSUDA, DDS
Strategies for Success
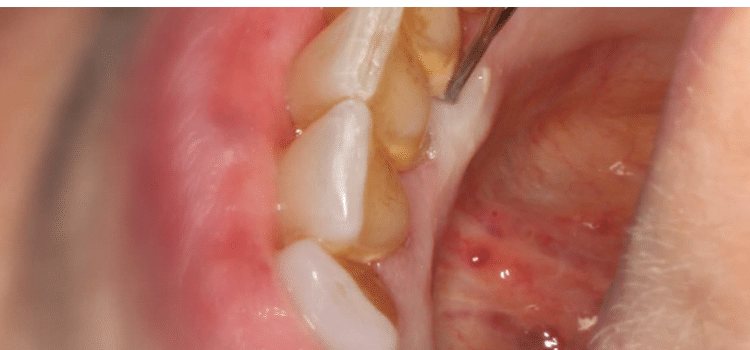
Removing tenacious calculus deposits requires a complementary approach that includes both ultrasonic and hand instrumentation.
Patients present at the dental office in varying stages of oral health. While some patients have little to no tenacious deposits, others exhibit heavy, persistent calculus that is challenging to remove. As the evidence demonstrates, all calculus deposits must be removed in order to maintain periodontal health.1–3 This fact charges dental hygienists to develop superior instrumentation technique in order to effectively remove biofilm and calculus deposits.
Although complete calculus removal is often impossible to achieve without open flap surgery, clinicians should strive to achieve this goal by reevaluating areas of bleeding on probing at subsequent appointments and rescaling judiciously with specialized small instruments. Scaling indiscriminately and forcefully with standard instruments should be avoided, as this can lead to overinstrumentation of roots. Ideally, this very precise root instrumentation should be accomplished with the aid of a dental endoscope, which, during the last decade, has allowed expert dental hygienists to achieve 99% calculus removal without overinstrumentation of the roots or periodontal surgery.4
TREATMENT PLANNING
Clinicians need to determine how many teeth they can effectively instrument during a single appointment when treating patients with heavy, tenacious calculus. Subsequent appointments should then be scheduled accordingly. This may be one quadrant, a sextant, or only two teeth, depending on the amount of calculus and the depth of pocketing. Instrumenting to completion in segments helps patients understand the contrast between their current disease state and where healing has occurred in response to the provided therapy. This demonstrates the need for additional therapy until treatment is complete.
COMPLEMENTARY APPROACH
The complementary approach is based on the idea that neither hand instrumentation nor power instrumentation is a substitute for the other. Both types of instrumentation offer unique benefits. When used in concert, they can improve the effectiveness of periodontal therapy.5
Hand instruments are not able to access all aspects of the dentition, such as the base of deep, narrow pockets. Ultrasonic scalers are able to reach the base of deep narrow pockets more easily when the appropriate ultrasonic insert/tip (UIT) is used. UITs, however, can be difficult to adapt to curvatures, contours, concavities, and longitudinal depressions.
The complementary approach improves efficiency when used on patients with pockets or extensive calculus deposits. The approach entails first implementing the ultrasonic scaler with sufficient power to remove the bulk of calculus deposits, then following with hand instruments to cover root contours, and, finally, performing a finishing debridement/flush using the power scaler with a thin UIT.
When implementing power scaling, remain aware of the UIT’s pattern of movement across the surface. Keep strokes slow, methodical, and comprehensive—not rapid and haphazard. Strokes must be precise and overlapping in order to completely debride the entire root surface.6,7 Choose the appropriate UIT for the task at hand. One UIT does not fulfill all power scaling needs. When deciding on a UIT, consider the cross-section of the tip. UITs that are round in shape are more effective for biofilm debridement, while those with a beveled, trapezoidal, or rectangular shape are more effective for calculus removal.
After the bulk of deposits has been removed with the ultrasonic scaler, hand instrumentation is recommended. If the patient presents with pockets, the use of hand instruments is critical. Teeth with deep pockets have accentuated surface contours that make comprehensive coverage with a UIT more difficult to achieve. Small diameter, curvature-bladed hand instruments are uniquely suited to adapt closely to the tighter concavities and convexities seen in deep pockets, making comprehensive surface coverage more likely to occur. Hand instruments are indicated for line angles and furcations following ultrasonic use for the same reason—especially when pockets exceed 4 mm.8 Periodontal pockets demand careful focus using precise technique. Specialized hand instruments, such as micro-minis and files, are needed to reach difficult-to-access areas.5,9,10
Periodontal files are well suited for crushing and fracturing calculus in the depths of pockets where sickle scalers cannot access. Activate linear pull strokes that are parallel to the terminal shank of the instruments (perpendicular to the blades themselves). Periodontal files play an essential role in periodontal therapy because they can effectively remove burnished calculus when all other instruments have failed. Use them on any periodontal maintenance patient with areas that bleed on probing—especially those with minute pinpoint bleeding, as this is an indication of burnished calculus.11–13 They can be positioned for use in any direction—vertical, oblique, and horizontal, which is especially effective on the cementoenamel junction.
Because sickles and files are not definitive debridement instruments, they must be followed up with scaling and root planing using curets with blade curvatures that can access the many contours of teeth. Begin with universal curets, which provide better torque and leverage than Gracey curets. Gracey and mini-Gracey curets follow the use of universal curets. For initial therapy and burnished calculus, use rigid Graceys as they are often the most effective. While Gracey curets are area-specific, they have great versatility and can be used in many other applications in periodontal therapy.
CONCLUSION
Effective instrumentation strategies and proper technique are the keys to successful outcomes. Ensuring that ultrasonic instrumentation is steady and thorough as opposed to random and haphazard is necessary for successful debridement. Optimally sharpened hand instruments used with adequate lateral pressure is an essential component of periodontal therapy, and will conserve time and effort while increasing the likelihood of success. A complementary approach to instrumentation combines both techniques’ unique advantages to better serve both the patient and the clinician.
References
- Cochran DL. Inflammation and bone loss in periodontal disease. J Periodontol. 2008;79:1569–1576.
- Haffajee AD, Cugini MA, Dibart S, Smith C, Kent RL Jr, Socransky SS. The effect of SRP on the clinical and microbiological parameters of periodontal diseases. J Clin Periodontol. 1997;24:324–334.
- Cobb CM. Clinical significance of non-surgical periodontal therapy: an evidence-based perspective of scaling and root planing. J Clin Periodontol. 2002;29(Suppl):6–16.
- Stambaugh RV, Myers G, Ebling W, Beckman B, Stambaugh K. Endoscopic visualization of the submarginal gingiva dental sulcus and tooth root surfaces. J Periodontol. 2002;73:374–382.
- Pattison AM, Matsuda S. Making the right choice. Dimensions of Dental Hygiene. 2003;1(8)(Suppl):4–10.
- Stach D. The five most common errors when using ultrasonic inserts. Dimensions of Dental Hygiene. 2010;8(7):46–50.
- Matsuda S. The importance of complete root surface coverage. Dimensions of Dental Hygiene. 2015;13(10):36–39.
- Otero-Cagide FJ, Long BA. Comparative in vitro effectiveness of closed root debridement with fine instruments on specific areas of mandibular first molar furcations. II. Furcation area. J Periodontol. 1997;68:1098–1101.
- Long B. The mini revolution. Dimensions of Dental Hygiene. 2003;1(3):28–31
- Pattison AM, Matsuda S. Technique focus—mini-bladed gracey curets. Dimensions of Dental Hygiene. 2006;5(4):28–29.
- Sherman PR, Hutchens LH, Jewson LG, Moriarty JM, Greco GW, McFall WT Jr. The effectiveness of subgingival scaling and root planing. I. Clinical detection of residual calculus. J Periodontol. 1990;61:3–8.
- Lang NP, Joss A, Orsanic T, Gusberti FA, Siegrist BE. Bleeding on probing. A predictor for the progression of periodontal disease? J Clin Periodontol. 1986;13:590–596.
- Checchi L, Montevecchi M, Checchi V, Zappulla F. The relationship between bleeding on probing and subgingival deposits. An endoscopical evaluation. Open Dent J. 2009;28:154–160.
From Dimensions of Dental Hygiene. January 2016;14(01):24,26.

