
Preventive Interventions for Musculoskeletal Disorders
Evaluating the evidence behind strategies designed to reduce the risk of these common injuries is key to improving the ergonomics of clinical practice.
Weighing the evidence on preventive interventions for musculoskeletal disorders can be challenging for dental hygiene educators and practitioners alike—especially given the lack of research regarding the efficacy of these measures in the practice of dental hygiene.1,2 The maintenance of musculoskeletal health is critical to practicing clinicians, as well as dental hygiene educators who are teaching the next generation of professionals. This warrants further investigation into the prevention of musculoskeletal disorders.
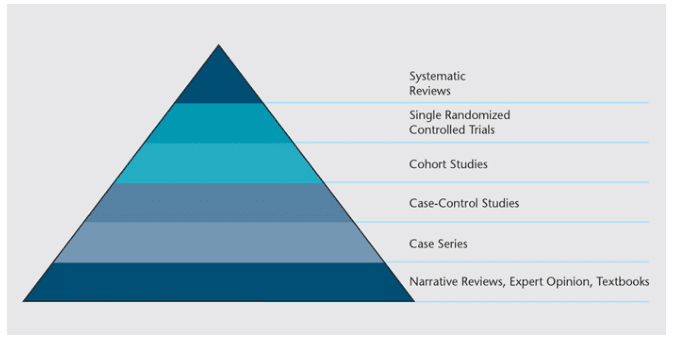
Since the mid-1990s, dental hygiene educators and clinicians have been charged with integrating an evidence-based approach into education, clinical practice, and research. However, in many circumstances, this task remains difficult.3 In part, this is because there may be little or no evidence to address a particular clinical question. One example is the limited research conducted on preventing or mitigating musculoskeletal disorders among clinicians. While there are several studies in the literature that investigate preventive or mitigative measures for musculoskeletal disorders in dental hygienists, only one study—which evaluated certain characteristics of hand scalers—is positioned relatively high on the evidence-based pyramid (Figure 1).4,5
Although there is general agreement on the existence of risk factors for musculoskeletal disorders among dental hygienists and other oral health professionals, there is little consensus on measures to prevent or manage them.6–10 Furthermore, there is a lack of information regarding ergonomic education and the rate of clinical implementation of preventive measures taught in educational institutions.6,10 In the case of interventions aimed at preventing or mitigating musculoskeletal disorders in dental hygienists, some preventive measures, such as loupes, are widely seen as beneficial to ergonomic practice. Yet, when used incorrectly, these can contribute to the very musculoskeletal disorders they were aimed at addressing.11
Traditionally, educators taught students about instrument design, selection, and use, as well as postural positioning during patient care. Often little or no attention was paid to the risks of musculoskeletal disorders or how to prevent them.12 In recent decades, however, an increased focus by educators and clinicians on occupational risks and musculoskeletal concerns has occurred. Many articles can be found that suggest numerous preventive measures aimed at limiting or avoiding musculoskeletal disorders among dental hygienists, but the information included in these articles needs to be critically analyzed before implementation.13 These preventive measures include what might be seen as common-sense approaches, such as improving fitness levels. Others focus on learning and adopting good postural skills.14–16 Complementary medicine offers alternatives to traditional medicine approaches, which often include the use of pain medications.17
Improved working environments, as well as better instrument and lighting design are frequently addressed in ergonomic studies.5 Nevertheless, the need for longitudinal studies and standardized research techniques that might improve clinical practice recommendations remains high. This article provides an overview of the evidence regarding improved instrument design and the use of loupes, two of the practices most commonly used to prevent or mitigate musculoskeletal disorders among dental hygienists.
INSTRUMENT DESIGN
In 2012, Rempel et al5 conducted one of the only workplace intervention studies on instrument design that evaluated arm pain among dentists and dental hygienists. Using a cluster-randomized controlled trial, eligible participants (110) were required to provide scaling and root planing or supragingival scaling procedures for more than 10 hours per week. Study participants had at least 1 year of experience in providing such therapies. They also completed weekly online questionnaires for 5 months to ascertain their weekly practice patterns, associated pain levels and numbness, and consumption of pain medication. Participants were subsequently divided into two groups to compare interventions. During the study, pain scores for three regions (wrist/hand, elbow/forearm, and the shoulder) improved in both intervention groups. However, participants who used instruments with light-weight and wide-diameter handles reported greater reductions in pain in all regions, compared with those who used instruments with heavy, narrow-diameter handles. The difference between groups was statistically significant for shoulder pain reduction only (not wrist or elbow pain). As noted by the authors, the intervention was limited to one type of instrument for each participant; thus, the use of multiple instruments with the same handle design may have impacted the study findings.
In another study that involved clinical simulation, Dong et al18 examined the effect of the instrument handle on hand muscle load and pinch force. Participants included 24 dentists and dental hygienists who had at least some scaling experience. Study subjects participated in an exercise using typodonts. The authors found that instruments with a 10 mm diameter and relative light weight (15 g to 18 g) were not only preferred by participants, but also produced the least amount of muscle load and pinch force. Instrument diameter was reported to be a more significant factor than instrument weight on muscle activity and pinch forces. Handles larger than 10 mm appeared to offer no additional benefits. Instruments lighter than 15 g were not included, and pain levels were not assessed in this study.
The results of these studies suggest that the use of instruments with wide-diameter and lightweight handles during dental hygiene procedures may be helpful in reducing musculoskeletal disorder risk.
IMPROVING VISUAL ACUITY WITH LOUPES
Surgical magnification has been used in medicine since the early 20th century, largely for improved visual acuity. Some studies have been conducted on the use of magnification in dentistry, but few have been done in dental hygiene. A seminal rationale for the use of loupes is that improved visual acuity will lead to improved patient care; however, there is little evidence to this effect. As noted by Sunnell and Rucker19 a decade ago, “There is little evidence-based information on the outcomes of dental hygiene services or clinical therapy with and without surgical magnification.” This remains the case today. However, logic suggests that improved visual acuity is beneficial during patient assessment procedures, such as oral cancer screenings or periodontal tissue evaluation. In 2012, Congdon et al20 found that the majority of dental hygiene faculty in the United States do not appear to have embraced the use of loupes in their institutions nor require them for student use. While the cost of loupes was identified as the prime reason for not requiring loupes for student use, educators may have also felt that magnification plays a less important role compared with developing skills in tactile sensitivity and proprioception when providing periodontal therapy.19
In contrast, the use of loupes to improve the ergonomics of clinical practice has received great attention. Most of the available evidence, however, is anecdotal. In spite of this, many oral health professionals report postural benefits due to the use of loupes.11,16,21,22
Much of the research on loupes and posture in dental hygiene has been conducted using student populations.21–23 Some authors have suggested that the use of loupes not only provides significant postural benefits for students, but also that loupes should be incorporated early in student’s educational experiences to facilitate the adoption of use in clinical practice.21 Branson et al23 note, however, that the long-term impact of improved posture and clinical performance with loupes remains unknown. Additional research is needed to examine the outcomes of dental hygiene services performed with the use of loupes, as well as the role of loupes in mitigating musculoskeletal disorders.
CONCLUSION
Musculoskeletal disorders should be thought of as a multifaceted problem—one that requires a multifaceted solution, especially given the dynamics of dental hygiene practice and variation among practitioners themselves.16 Whether preventive measures should be primarily focused on implementing more ergonomically designed work-related devices and environments,5 using complementary or alternative medicine to mitigate symptoms,17 alleviating work-related psychosocial stress,24 or a combination of these approaches is not abundantly clear. Research on other common ergonomic interventions—such as ambidextrous gloves, intraoral cameras, and operator seating—is also needed.
Dental hygiene is a prevention-oriented profession. Researchers should be encouraged to conduct additional high-quality research—especially longitudinal studies—on prevention strategies that help mitigate musculoskeletal disorders without adversely affecting patient care.
References
- Hayes MJ, Smith DR, Taylor JA. Musculoskeletal disorders in a 3 year longitudinal cohort of dental hygiene students. J Dent Hyg. 2014;88:36-41.
- Lalumander JA, McPhee SD. Prevalence and risk factors of hand problems and carpal tunnel syndrome among dental hygienists. J Dent Hyg 2001;75:130–134.
- Forrest JL, Miller SA. Evidence-based decision making in dental hygiene education, practice, and research. J Dent Hyg. 2001;75:50–63.
- Kott K. Evidence-based decision making. Dimensions of Dental Hygiene. 2015;13(4):69–72.
- Rempel D, Lee D, Dawson K, Loomer P. The effects of periodontal curette handle weight and diameter on arm pain. J Am Dent Assoc. 2012;143:1105–1113.
- Hayes MJ, Smith DR, Cockrell D. An international review of musculoskeletal disorders in the dental hygiene profession. Int Dent J. 2010;60:343–352.
- Morse T, Bruneau H, Dussetschleger J. Musculoskeletal disorders of the neck and shoulder in the dental professions. Work. 2010;35:419–429.
- Sanders MJ, Michalak-Turcotte C. Preventing work-related musculoskeletal disorders in dental hygienists. Ergonomics and the Management of Musculoskeletal Disorders. St. Louis: Butterworth Heinemann; 2004:448–469.
- Murphy DC. Ergonomics and the Dental Care Worker. Washington, DC: American Public Health Association; 1998.
- Akesson I, Johnsson B, Rylander L, et al. Musculoskeletal disorders among female dental personnel-clinical examination and a 5 year follow-up study of symptoms. Int Arch Occup Environ Health. 1999;72:395–403.
- Rucker LM. Surgical magnification: Posture maker or posture breaker? In: Ergonomics and the Dental Care Worker. Murphy DC, ed. Washington, DC: American Public Health Association; 1998:191–216.
- Beach J, DeBiase C. Assessment of ergonomic education in dental hygiene curricula. J Dent Ed. 1998;62:421–425.
- Biller FE. Occupational hazards in dental practice. Oral Hygiene. 1946;36: 1194–1201.
- Barry R, Spolarich AE, Weber M. Occupational health hazards. Dimensions of Dental Hygiene. 2014;12(9):58–61.
- Sanders MJ, Michalak-Turcotte C. Posture makes perfect. Dimensions of Dental Hygiene. 2011;9(11):30–35.
- Valachi B, Valachi K. Preventing musculoskeletal disorders in clinical dentistry: strategies to address the mechanisms leading to musculoskeletal disorders. J Am Dent Assoc. 2003;134:1604–1612.
- . Chismark A, Asher G, Stein M, Tavoc T, Curran A. Use of complementary and alternative medicine for work-related pain correlates with career satisfaction among dental hygienists. J Dent Hyg. 2011;85:273–284.
- Dong H, Barr A, Loomer P, LaRoche C, Young E, Rempel D. The effects of periodontal instrument handle design on hand muscle load and pinch force. J Am Dent Assoc. 2006;137:1123–1128.
- Sunnell S, Rucker L. Surgical magnification in dental hygiene practice. Int J Dent Hyg. 2004;2:26–35.
- Congdon LM, Tolle SL, Darby M. Magnification loupes in U.S. entry-level dental hygiene programs-occupational health and safety. J Dent Hyg. 2012;86:215–222.
- Maillet JP, Millar M, Burke J, Maillet M, Maillet W, Neish N. Effects of magnification loupes on dental hygiene student posture. J Dent Ed. 2015;72:33–44.
- Branson BG, Bray KK, Gadbury-Amyot C, et al. Effect of magnification lenses on student operator posture. J Dent Ed. 2004;68:384–389.
- Branson B, Black M, Simmer-Beck M. Changes in posture: A case study of a dental hygienist’s use of magnification loupes. Work. 2010;35:467–476.
- Crawford L, Gutierrez G, Harber P. Work environment and occupational health of dental hygienists: A qualitative assessment. J Occup Environ Med. 2005;47:623–632.
From Dimensions of Dental Hygiene. January 2016;14(01):18,20–22.

