 KARELNOPPE/ISTOCK/GETTY IMAGES PLUS
KARELNOPPE/ISTOCK/GETTY IMAGES PLUS
Dental caries remains the most prevalent chronic disease in both children and adults in the United States, even though it is largely preventable.1 Monitoring the prevalence of caries is key to preventing and controlling oral diseases.2 According to a study published by the US Centers for Disease Control and Prevention (CDC), one out of five children ages 5 to 11, and one out of seven adolescents ages 12 to 19 have tooth decay.3 More specifically, the National Institute of Dental and Craniofacial Research reports 42% of children ages 2 to 11 have had caries in their primary teeth, and 21% of children ages 6 to 11 have had caries in their permanent teeth.1
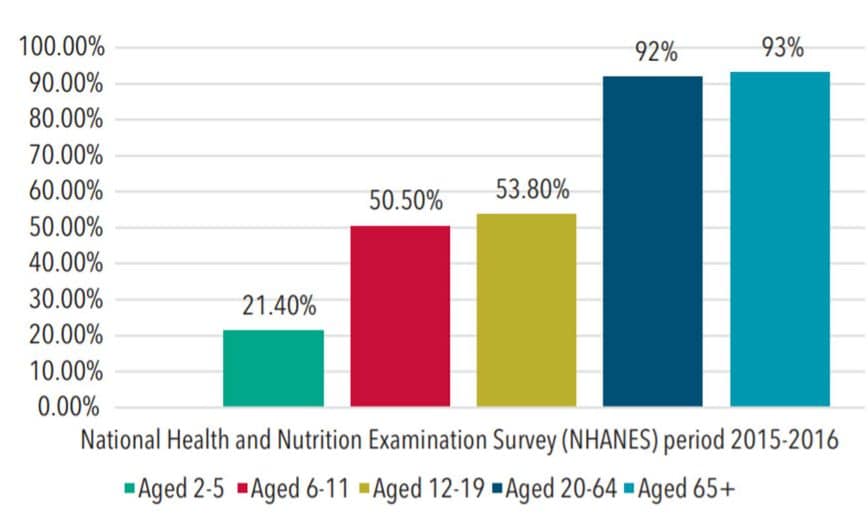
More recent statistics from the 2015-2016 National Health and Nutrition Examination Survey show the percentage of caries experience only is 41.9% among youth ages 2 to 19 (this is the average of percentages for those aged 2 to 19). These statistics demonstrate that caries prevalence increases with age (Figure 1).2 The highest prevalence of caries was in Hispanic adolescents and those living in low-income families.2 In addition, nearly all adults ages 20 to 64 (92%) and adults age 65 and older (93%) experienced caries in permanent teeth (Figure 1). Although caries has significantly decreased for most Americans over the past four decades, disparities remain among some population groups. In addition, this downward trend has recently reversed for young children.1
Based on national surveys of oral health status over the past 40 years, the prevalence of decay in primary teeth has persisted at similar levels. Estimates of caries prevalence and severity in children and adolescents for whom long-standing trends showed major declines in previous decades have leveled off. Additionally, an increasing number of adults are retaining more teeth, with a small reduction in the average number of decayed teeth. However, these largely favorable overall population trends mask large and important disparities in caries experience and its treatment.4
DENTAL SEALANTS
More progress has been made in the treatment of dental caries than in its prevention. With the shift from the surgical model of treatment to a medical model of disease management, strategies to emphasize disease prevention and conservation of tooth structure must be examined.5 Effective measures, such as dental sealants, should be considered to protect the pit and fissures on occlusal surfaces of posterior teeth.
Sealants play a role in primary and secondary prevention. Pit and fissure sealants have been used for nearly five decades to prevent and control caries lesions on primary and permanent teeth.6 Sealants are one of the most effective and least invasive methods available to ensure the complete protection and total preservation of the occlusal surface.7 According to the CDC, sealants can prevent up to 80% of tooth decay in treated teeth.8 Effectively penetrating and sealing teeth can prevent lesions, and should be part of a comprehensive caries management approach.9
In addition to the use of sealant materials for primary prevention of caries, a secondary prevention in areas already affected by caries should be considered. Evidence suggests sealants inhibit the progression of noncavitated caries lesions.7 The purpose of sealant application is to arrest the caries lesion and eliminate viable microorganisms under the sealing material.7 Therefore, teeth with early noncavitated carious lesions would benefit from sealant application.10
The long-term success of sealants depends on the intact mechanical barrier of the material. Strict compliance from the patient and access to regular recare appointments are essential. Otherwise, saliva and food remnants can penetrate the leaked sealant material, allowing bacterial growth, which leads to caries development or progression beneath the sealant.11 Despite the overall increase in sealant utilization, they are still underused worldwide.10
SEALANT PREVALENCE
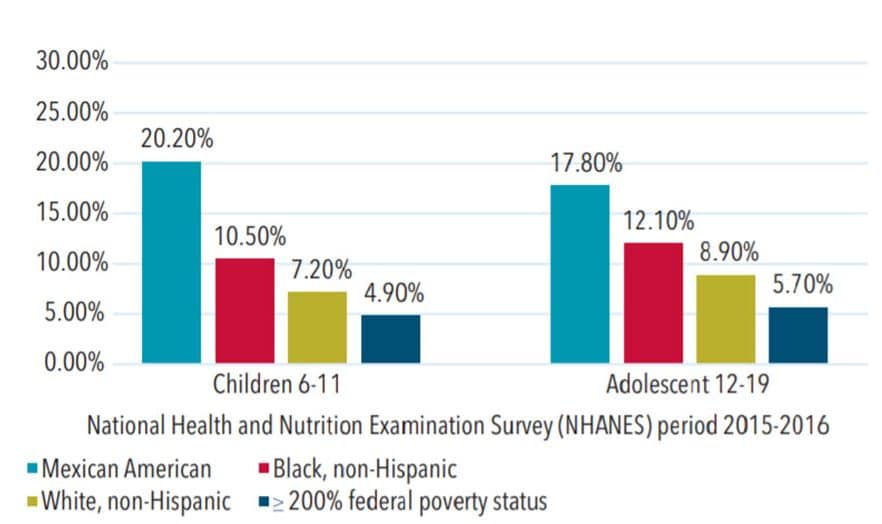
The CDC’s Oral Health Division monitors the use of sealants by identifying and reporting the number of children and adolescents with at least one sealed permanent molar. The CDC’s 2019 Oral Health Surveillance Report showed an average sealant prevalence increase for children and adolescents from 31% during 1999-2004 to 42% during 2011-2016 for all sociodemographic characteristics. Further investigation of each specific sociodemographic characteristic revealed a wide range of increased sealant prevalence for children and adolescents (Figure 2).12 Sealant prevalence for adults and seniors is not part of this survey and therefore not reported. Limited current research is available regarding sealant prevalence among these populations.
Research has also investigated the correlation between sealant retention and caries prevention in resin-based and glass ionomer (GI) sealant materials.13–16 In previous studies, resin-based sealant materials have been considered superior due to higher retention rates and proven cariostatic effect.14 In contrast, GI sealants had lower retention rates and inferred lower cariostatic effect.13,15 Current studies confirm resin-based sealant materials have higher retention rates compared with GI sealant materials.13–16 However, further investigation specific to caries development in teeth with retained or nonretained resin-based sealant materials compared to GI sealant materials showed no significant differences. This may be due to fractured GI sealants leaving small particles embedded with fluoride in the pits and fissures, which act as a reservoir, preventing caries development without the GI sealant being retained.13,15
Continuous review of the literature is necessary to make evidence-based decisions related to sealants for individualized patient care. Research has proven GI sealants and resin-based sealants are effective means in caries prevention.17 When selecting sealant materials, factors related to sealant placement—such as individual patient characteristics; physical modality of sealant placement (dental office, community site); moisture barrier abilities; and staffing (use of four-handed dentistry)—should be considered.13
Resin-based sealants have high retention rates but some require cumbersome placement technique.14 Due to the need for moisture control when placing some resin-based sealants, the use of four-handed dentistry is recommended. As such, traditional dental settings may be best equipped for resin-based sealants.6 A resin-based sealant is available, however, that does not require a dry field for placement.
In comparison, GI sealant materials have hydrophilic properties that do not require complete moisture control, making them a good option for community-based settings.14 These sealants can also be placed on a large number of high-risk patients in a short time frame.13
Regardless of the sealant material selected, oral health professionals should increase efforts to provide this key caries-prevention technique to all high-risk populations.12 Various modalities for sealant delivery have evolved over the years. Currently, most community-based sealant programs occur in schools.
MODES OF SEALANT DELIVERY
School-based sealant programs to prevent caries are strongly endorsed by organizations and governmental agencies, including the American Dental Association’s Council on Scientific Affairs, Association of State and Territorial Dental Directors, and CDC Division of Oral Health.6,18–20 Teledentistry is presenting a new way to provide preventive oral healthcare. Most school-based sealant programs place sealants on as many children as possible while on-site for a limited time.20 In contrast, teledentistry programs have a continuous presence on-site, allowing frequent monitoring of sealant retention and tooth eruption.21,22 In addition to school-based settings, teledentistry is used to increase access to preventive oral healthcare in a variety of settings for patients of all ages.
CONCLUSION
Dental sealants—as an optional treatment for caries prevention—should be considered for all high-risk patients. The role of sealants in primary prevention and permanent teeth is well established in the literature.6,10 As modalities for dental care continue to evolve, oral health professionals are well prepared to provide sealants in order to reduce caries prevalence among underserved populations in a variety of settings.
REFERENCES
- National Institute of Dental and Craniofacial Research. Dental Caries (Tooth Decay). Available at: nidcr.nih.g/v/research/data-statistics/dental-caries. Accessed July 15, 2020.
- Fleming E, Afful J. Prevalence of total and untreated dental caries among youth: United States, 2015–2016. NCHS Data Brief. 2018;307:1–8.
- United States Centers for Disease Control and Prevention. Children’s Oral Health. Available at: cdc.gov/oralhealth/basics/childrens-oral-health/index.html. Accessed July 15, 2020.
- Rozier R, White A, Slade G. Trends in oral diseases in the U.S. populationJ J Dent Ed. 2017;81(8s):e97-e109.
- Lee Y. Diagnosis and prevention strategies for dental caries. J Lifestyle Med. 2013 Sep;3:107–109.
- Wright JT, Crall JJ, Fontana M, et al. Evidence-based clinical practice guideline for the use of pit-and-fissure sealants. J Am Dent Assoc. 2016;147:672–682.
- Condò R, Cioffi A, Riccio A, et al. Sealants in dentistry: a systematic review of the literature. Oral (Rome). 2014;6:67–74.
- United States Centers for Disease Control and Prevention. Division of Oral Health at a Glance. Available at: cdc.gov/chronicdisease/resources/publications/aag/oral-health.htm. Accessed July 15, 2010.
- Anusavice KJ, Shen C, Rawls HR. Phillips’ Science of Dental Materials. St. Louis: Elsevier/Saunders; 2013.
- Naaman R, El-Housseiny AA, Alamoudi N. The use of pit and fissure sealants—a literature review. Dent J (Basel). 2017;5:34.
- Cvikl B, Moritz A, Bekes K. Pit and fissure sealants—a comprehensive review. Dent J (Basel). 2018;6:18.
- United States Centers for Disease Control and Prevention. Dental Sealants. Available at: cdc.gov/oralhealth/publications/OHSR-2019-dental-sealants.html. Accessed July 15, 2020.
- Alirezaei M, Bagherian A, Shirazi AS. Glass ionomer cements as fissure sealing materials: yes or no? J Am Dent Assoc. 2018;149:640–649.
- Praveen B, Prathibha B, Reddy P, et al. Sealants revisited: An efficacy battle between the two major types of sealants—a randomized controlled clinical trial. Dent Res J. 2019;16:36–41.
- Mickenautsch S, Yengopal V. Caries-preventive effect of high-viscosity glass ionomer and resin-based fissure sealants on permanent teeth: a systematic review of clinical trials. Plos One. 2016;11:e0146512.
- Al-Jobair A, Al-Hammad N, Alsadhan S, et al. Retention and caries-preventive effect of glass ionomer and resin-based sealants: an 18-month-randomized clinical trial. Dent Mater J. 2017;36:654–661.
- Wright JT, Crall JJ, Fontana M, et al. Evidence-based clinical practice guideline for the use of pit-and-fissure sealants. American Academy of Pediatric Dentistry, American Dental Association. Pediatr Dent. 2016;38:E120-E36.
- Association of State and Territorial Dental Directors. Best Practice Approaches for State and Community Oral Health Programs. Available at: astdd.org/docs/sealant-bpar-update-11-2017-final.pdf. Accessed July 15, 2020.
- United States Centers for Disease Control and Prevention. School-based Sealant Programs. Available at: cdc.gov/OralHealth/dent_l_sealant_program. Accessed July 15, 2020.
- United States Centers for Disease Control and Prevention. CDC-Funded States. Available at: cdc.gov/oralhealth/state_programs/cooperative_agreements/index.htm. Accessed July 15, 2020.
- Daniel SJ, Kumar S. Teledentistry; a key to component in access to care. J Evid Base Dent Pract. 2014;14S:201–208.
- Alabdullah JH, Daniel SJ. A systematic review on the validity of teledentistry. Telemed J E Health. 2018;24:639–648.
From Dimensions of Dental Hygiene. July/August 2020;18(7):22-24.

