Root Caries Prevention and Treatment
Oral health professionals need to be knowledgeable about this common oral condition and understand which patient populations are at greatest risk.
While tooth loss was common just a generation ago, today most older adults in the United States retain their natural dentition throughout their lifetimes.1 The prevalence of gingival recession, however, increases with age.2 Many factors contribute to gingival recession, including the normal aging process, poor oral hygiene, and the presence of periodontal diseases. Individuals with gingival recession are at increased risk of root caries as recession exposes the root surfaces to the oral environment. The high prevalence of xerostomia among older adults also raises the risk of root caries in this population.
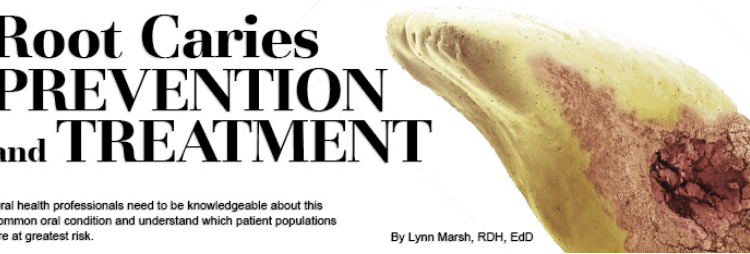
Root caries are typically found on the root surface of a tooth, generally at or below the cementoenamel junction. In the US, the prevalence of root caries among individuals older than 75 is more than 50%, and among those age 65 to 75, the prevalence is approximately 25%.3 As the number of older adults in the US continues to grow, oral health professionals will be treating more geriatric patients in private practice, senior centers, assisted living communities, and long–term care facilities.4 As such, clinicians need to provide this patient population with education on the prevention and treatment of root caries.
ROOT CARIES PREVENTION
Caries risk assessment is integral to preventing root caries. A comprehensive examination that utilizes the caries management by risk assessment (CAMBRA) approach to older patients is an appropriate first step.5 Thorough biofilm removal is critical to reducing root caries risk. Oral health professionals should provide guidance on dietary risk factors and education on effective oral hygiene strategies, including the use of chemotherapeutics, to aid in root caries prevention. Fluoride application is key, as it reduces biofilm proliferation and encourages remineralization.6 For patients at elevated risk of root caries, the in-office application of fluoride varnish four times annually as well as the use of prescription fluoride products (containing 5,000 ppm) may be helpful.6
Evidence supporting the role of chlorhexidine in caries prevention is mixed, but for frail patients who need help performing oral hygiene, chlorhexidine mouthrinse or the application of a chlorhexidine-thymol varnish may aid in reducing root caries risk.6,7
Silver diamine fluoride, which has just recently become available in the US, is particularly effective against root caries because it arrests or significantly slows the demineralization of dentin.6 A study of 227 older adults who had at least five exposed root surfaces found the group that received an annual application of silver diamine fluoride and oral health education every 6 months experienced the greatest reduction in new root caries lesions and more effective arrest of existing root caries compared with controls.8
For patients who are unable to access professional dental care, a literature review suggests that daily self-application of a 250 ppm amorphous calcium phosphate paste and daily use of a 1,110 ppm sodium fluoride dentifrice with triclosan may help reduce caries risk.9
Remineralization can be helpful in managing root caries surface lesions. Baysan et al10 demonstrated that the use of a 5,000 ppm fluoride dentifrice was significantly more effective in remineralizing tooth structure than dentifrice containing 1,100 ppm of fluoride. For incipient root caries, surface recontouring of the root structure may be indicated to excavate softened dental tissues and create a smooth surface. The new surface will more effectively absorb fluoride treatments, inhibit biofilm retention, and may encourage patients to comply with their oral health care regimens.11
THE ROLE OF XEROSTOMIA
Individuals with xerostomia or salivary gland hypofunction may experience an increased risk of oral infections and dental caries. When assessing root caries risk, a patient’s medication usage should be reviewed. Clinicians should also use patient medical histories to determine if a patient has an autoimmune disease, which may also increase the risk of dry mouth.
Low salivary flow caused by xerostomia renders tooth structures more vulnerable to acidic challenges from food, beverages, and plaque bacteria.12 As a result, demineralization is initiated, leading to tooth decay. Saliva offers buffering capabilities that protect the teeth from acid challenges, especially on exposed root surfaces.13 Saliva also acts as a reservoir for the calcium ions and phosphate ions needed to remineralize the tooth surface.12 Patients with low salivary flow do not enjoy these caries protective benefits. Alternative measures may be required to support the remineralization process. Patients with xerostomia should use a prescription-strength fluoride toothpaste. The addition of a calcium phosphate product to patients’ oral hygiene regimens may be helpful because they provide more calcium and phosphate ions, thereby encouraging remineralization.
TREATMENT STRATEGIES
Root caries should be assessed with clinical and radiographic examinations. Radiographs are also helpful in determining the extent of root caries. Restorative treatment is often necessary when the root surface lesion is extensive.11 Dental materials used in restoring root surface caries should provide a good seal between the restoration and the tooth, acceptable esthetics, simplicity in placement, and continuous fluoride release.11 Some evidence suggests that glass-ionomer cement may be best for restoring root caries lesions, especially if they are located subgingivally.14 Glass ionomer cement does not cause pulpal irritation, contains 20% fluoride release, is relatively easy to place, offers esthetic benefits, is anticariogenic and antibacterial, and adheres easily to root structures in a moist field.11
Composite restorations, which are esthetically pleasing, are also frequently used. However, they do not have anticariogenic properties. They are not recommended for patients with poor oral hygiene because they pose a risk for recurrent decay.11 Amalgam, due to its poor esthetics, is not typically used to restore root caries.
CONCLUSION
Prevention education, treatment planning, and restoring root caries should be provided on an individual basis. A comprehensive assessment of root caries etiology and risk factors provides a sound basis for prevention.15 The initiation of root caries might be significantly reduced by the implementation of preventive dental programs and the application of chemotherapeutic agents by oral health professionals.1
REFERENCES
- National Institute of Dental and Craniofacial Research. Oral Health in America: a Report of the Surgeon General. Available at:?nidcr.nih.gov/DataStatistics/ SurgeonGeneral/Report/ExecutiveSummary.htm. Accessed September 30, 2015.
- Wierichs R, Meyer-Luecke H. Systematic review on noninvasive treatment of root caries lesions. J Dent Res. 2015;94:261–271.
- Centers for Disease Control and Prevention. Public health and aging: retention of natural teeth among older adults–United States, 2002. MMWR Morb Mortal Wkly Rep. 2003;52:1226–1229.
- Bowen D. Prevention of root caries. J Dent Hyg. 2011;85:78–82.
- Hurlbutt M, Young DA. A best practices approach to caries management. J Evid Based Dent Pract. 2014;14(Suppl):77–86.
- Gregory D, Hyde S. Root caries in older adults. J Calif Dent Assoc. 2015;43:439–445.
- Slot DE, Vaandrager NC, Van Loveren C, Van Palenstein Helderman WH, Van der Weijden GA. The effect of chlorhexidine varnish on root caries: a systematic review. Caries Res. 2011;45:162–173.
- Zhang W, McGrath C, Lo EC, Li JY. Silver diamine fluoride and education to prevent and arrest root caries among community-dwelling elders. Caries Res. 2013;47:284–290.
- Gluzman R, Katz R, Frey B McGowan R. (2013). Prevention of root caries: A literature review of primary and secondary preventive agents. Spec Care Dent. 2013;33:133–140.
- Baysan A, Lynch E, Ellwood R, Davies R, Peterson L, Boorsboom P. Reversal of primary root caries using dentifrices containing 5,000 and 1,100 ppm fluoride. Caries Res. 2001;35:41–46.
- Gupta B, Marya C, Juneja V, Dahiya V. Root caries: an aging problem. Available at: ispub.com/IJDS/5/1/5636. Accessed September 30, 2015.
- Nan S, Marek, C, Ching V, Grushka M. Caries prevention for patients with dry mouth. J Can Dent Assoc. 2011;77:85.
- Jensen SB, Pedersen AM, Reibel J, Nauntofte B. Xerostomia and hypofunction of the salivary glands in cancer therapy. Support Care Cancer. 2003;11:207–225.
- Vehkalahti M, Rajala M, Tuominen R, Paunio I. (1983). Prevalence of root caries in the adult Finnish population. Community Dent Oral Epidemiol. 1983;11:188–190.
- Strassler H. Caries: Treatment options based upon etiology of the lesion. Available at:?dentalaegis.com/id/2005/10. Accessed September 30, 2015.
From Dimensions of Dental Hygiene. October 2015;13(10):21–22.

