Provide Comprehensive Care for Patients with Marfan Syndrome
Dental hygienists can support the early diagnosis and effective treatment of this genetic disorder.
This course was published in the June 2014 issue and expires June 30, 2017. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Define Marfan syndrome and explain its hereditary pattern.
- Describe the etiology of Marfan syndrome.
- Identify the systemic and orofacial manifestations of this disorder.
- Discuss the considerations for managing patients with Marfan syndrome during delivery of oral health care.
Marfan syndrome is a relatively rare disorder of the body’s connective tissue that causes life-threatening complications.1 Predominantly an inherited disorder, 25% of Marfan syndrome cases are caused by genetic mutations.2 It can affect multiple organ systems—but mostly impacts the connective tissue of the cardiovascular, ocular, and skeletal systems.1,2 The cardiovascular system is the most commonly affected.1
Marfan syndrome follows the autosomal dominant pattern of genetic inheritance,1,2 meaning there is 100% vertical transmission from one generation to the next.2 The offspring of a parent with Marfan syndrome has a 50% chance of inheriting the condition.2 Early diagnosis of the syndrome is crucial to preventing or delaying life-threatening complications and premature death.1 Unfortunately, diagnosing Marfan syndrome is challenging because it is highly variable in severity and manifestations of identifiable features.1 The prevalence of Marfan syndrome worldwide is between five and eight people per 100,000.3 There is no gender or racial predilection.3
Marfan syndrome is frequently diagnosed during adolescence or young adulthood—as physical features often remain unnoticeable during early childhood.1 The average life expectancy for untreated patients with Marfan syndrome is 32. Patients who receive treatment, however, can attain normal life expectancy.4
Oral health professionals are key members of the multidisciplinary team that helps individuals with Marfan syndrome maintain their health, and they may be able to spot the first signs and symptoms of the disease among those patients who are undiagnosed.
ETIOLOGY
A deficiency in the glycoprotein fibrillin-1 causes the disordered connective tissue indicative of Marfan syndrome.1 The deficiency is caused by a mutation of the fibrillin-1 gene, which is located on chromosome 15.2,5 This gene functions with elastin to form the elastic fibers found in connective tissue.5 The mutation of the fibrillin-1 gene also increases the likelihood that the microfibrils, which supply connective tissue with strength and flexibility, will become fragmented.5 This process is what causes the most common life-threatening complications associated with Marfan syndrome.5
DIAGNOSIS
The diagnosis of Marfan syndrome is achieved through a universally accepted systematic methodology called the modified Ghent criteria.5 The criteria are based on whether there is a positive family history of the condition, involvement in any of the three main organ systems (cardiovascular, ocular, or skeletal), and the reliability of the identified clinical features.1 For example, aortic dilation—which can be detected early using echocardiography—is a highly reliable sign present in more than 90% of Marfan syndrome cases. On the other hand, mitral valve prolapse is considered a weak sign because of its high prevalence among the general population.1
Positive diagnosis is made when there is involvement of at least two organ systems with at least one major manifestation, such as aortic dilation or ectopic lentis, in the presence of an affected first-degree relative.1,5 Though there is extensive development in understanding the molecular and genetic aspects of Marfan syndrome, the diagnosis is dependent on the clinical features and the modified Ghent criteria, because fibrillin-1 mutation can cause conditions other than Marfan syndrome.5 Genetic testing is only used as an adjunct for clinical diagnosis.5 Therefore, a multidisciplinary approach—including cardiac, orthopedic, ophthalmologic, and genetic testing—is recommended to confirm all diagnoses.5 A differential diagnosis is necessary when evaluating suspected cases.
MAJOR SYSTEMIC MANIFESTATIONS
The most serious life-threatening condition associated with Marfan syndrome is aortic dissection/rupture.1–5 Aortic rupture is the most common cause of premature death in patients with untreated Marfan syndrome.5 In most cases, the ascending aorta is affected—as it is most exposed to the hemodynamic force of the left ventricle, and has the greatest amount of fibrillin-deficient elastic fibers.1 The aortic rupture is caused by increased proteolysis and associated fragmentation of the elastic fibrils in the aortic wall.5 Once aortic dilation is identified, prophylactic treatment with selective beta-adrenergic blockers and lifestyle modification to restrict physical activity are used to manage the condition.1 Selective beta-adrenergic blockers—predominantly atenolol, which binds to the beta-1 receptor in the cardiac muscle—are used to decrease the heart rate and force of contractility. This reduces the hemodynamic force exerted on the ascending aorta and other blood vessels, ultimately delaying the progression of dilation.6
Recent clinical trials have explained the additional benefit and rationale of using an angiotensin II receptor blocker (ARB) in addition to the beta-selective blocker for prophylactic treatment of aortic dilation in patients with Marfan syndrome.7 ARBs interfere with the microscopic events in the underlying pathophysiology of aortic dilation as compared to beta blockers, which only act to reduce the hemodynamic force on the aortic walls.7
Changes in the aortic wall are monitored using magnetic resonance imaging, which is an indispensable tool in diagnosing cardiac complications in patients with Marfan syndrome.1 Mitral valve prolapse is also common, affecting about 75% of those with Marfan syndrome, and the risk of developing infective endocarditis is also increased.1
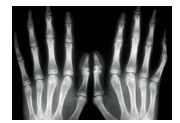
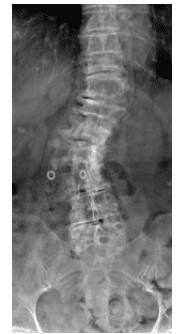
Patients affected by Marfan syndrome are usually tall and thin, with disproportionately long limbs, fingers, and toes (Figure 1).1,2,4,8 Arachnodactyly is the scientific term for the condition of abnormally long, slender fingers and toes.4 These patients also exhibit hypermobility of the joints, which is often associated with dislocation and joint pain.1,2,4,8 Kyphoscoliosis, an abnormal curvature of the spine both in coronal and sagittal plane, is characteristic of Marfan syndrome, and the incidence varies between 40% and 75% (Figure 2).1 Other common skeletal manifestations include excavatum, or hollowed chest; pectus carinatum, or pigeon chest; and dural ectasia, or bulging of the dural sac around the spinal cord in the lumbar region. The latter is reported in 60% of patients with the syndrome.1,2,8
The most common ocular anomaly associated with Marfan syndrome is ectopic lentis, which is the dislocation/subluxation of the eye lens.1 It is found in approximately 50% to 80% of those with Marfan syndrome.1 The displaced lens may eventually acquire a cataract or clouding of the eye lens.1 Other ocular manifestations commonly seen in patients with Marfan syndrome include: myopia or nearsightedness; strabismus or squint, which may be unilateral or bilateral; glaucoma due to increased intraocular pressure; and retinal detachment.1,2 Regardless of these complications, the visual acuity of most individuals with Marfan syndrome remains reasonably normal,1 and most ocular problems can be effectively corrected and managed by an optometrist and ophthalmologist.
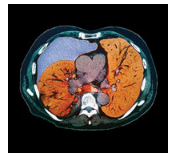
People with Marfan syndrome are more susceptible to pneumothorax—an abnormal collection of air or gas in the pleural space that separates the lung from the chest wall, which exerts pressure on the lung, limiting its capacity—than the general population (Figure 3).1 Individuals with the syndrome may have normal or slightly abnormal lung health but can also experience severe lung tissue defects. Ultimately, these defects may cause respiratory disorders, such as emphysema, asthma, and bronchiectasis (flabby and scarred bronchioles).1,2,7
OROFACIAL MANIFESTATIONS
The orofacial manifestations of Marfan syndrome are highly variable. Patients with Marfan syndrome exhibit a condition called dolichocephalism, or an elongated, narrow face.4 Face length is disproportionately long relative to its width.4 The eyes are sunken inside the orbital cavity, creating a condition called enophthalmos.4 The mid-facial region appears to be underdeveloped, demonstrating hypoplasia of the malar bone.4 Temporomandibular joint (TMJ) disorders are very common in patients with Marfan syndrome.2,3 These patients typically show hypermobility of the TMJ and hyperextensibility of the muscle associated with the mandibular movement, resulting in frequent disarticulation of the TMJ.2,3 A majority of the patients have a protruded mandible, but mandibular retrognathism has also been reported.2,3 In addition, patients with Marfan syndrome display distinctive intraoral and dental features.
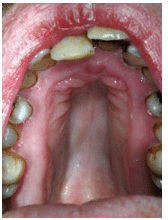
Intraorally, high/deep arched palate is identified in 50% of the patients with Marfan syndrome (Figure 4).2,4 The teeth are usually long and narrow with severe crowding.2,3 Other malrelations of the teeth, such as crossbite and open bite, are also common.2 DeCoster et al3 reported the presence of local enamel hypoplastic spots among patients with Marfan syndrome, which may increase their risk of caries—especially when found in the primary dentition.3 Supernumerary teeth, root deformities, and pulpal anomalies are also frequently reported among patients with Marfan syndrome.2,3 Other possible but rarely reported dental manifestations include complete/partial anodontia, amelogenesis, dentinogenesis imperfecta, and developmental odontogenic cysts.2 Variable evidence exists to illustrate the relationship between the fibrillin deficiency in Marfan syndrome and the risk for other dental diseases, such as gingivitis, caries, and periodontitis.
As Marfan syndrome is a connective tissue disorder characterized by the deficiency of the protein fibrillin-1, it is possible that the mutation predisposes patients to periodontal diseases. Staufenbiel et al9 conducted a study in Germany that looked at whether the mutated or disordered elastic fibers in the periodontal ligament of individuals with Marfan syndrome increased the susceptibility to periodontal diseases. A comprehensive periodontal examination was performed on 82 study subjects, 51 of whom had Marfan syndrome and 31 healthy controls, that included assessment of probing depth, gingival recession, clinical attachment level, and bleeding on probing. The researchers found no statistically significant differences between the two groups. Staufenbiel et al concluded that patients with Marfan syndrome did not show a higher prevalence of periodontitis than the general population. They did find, however, that the crowding of the teeth in patients with Marfan syndrome may increase the risk of gingival inflammation. The study authors concluded that patients with Marfan syndrome should undergo professional oral prophylaxis frequently to reduce the other risks for periodontitis.9
SCIENCE PHOTO LIBRARY / SCIENCE SOURCE IMAGES
De Coster et al3 did find incidence of severe periodontitis among Marfan syndrome patients, as well as higher rates of severe gingivitis compared to controls, in a case-control study. Straub et al10 and Shiga et al11 also found that patients with Marfan syndrome were at increased risk for severe periodontitis, but the evidence is unclear as to the exact relationship between the two. Additional research is needed to understand the true effect of disordered elastic fibers on the initiation, progression, and severity of periodontal diseases in individuals with Marfan syndrome.
De Coster et al3 also assessed caries risk among Marfan syndrome patients, but found no significant difference between those with Marfan syndrome and their control group in overall decayed, missing, filled teeth index scores. The study did find an increased risk of caries present among patients with Marfan syndrome younger than 18.3 The increased presence of calculus can be attributed to the inadequate removal of bacterial biofilm, possibly due to crowded dentition.
MANAGEMENT CONSIDERATIONS DURING DENTAL TREATMENT
Patients with Marfan syndrome are at greater risk of developing mitral valve prolapse and infective endocarditis than the general population.1–3 According to the American Heart Associations’ revised 2007 guidelines for antibiotic premedication, patients at risk for mitral valve prolapse no longer require antibiotic premedication.12,13 On the other hand, the guidelines state that patients with congenital heart disease or artificial heart valves should be premedicated before invasive dental procedure.12,13 As the evidence is inconclusive, patients’ cardiologists should be consulted regarding the need for antibiotic prophylaxis.
Preprocedural rinsing of the oral cavity with an antimicrobial mouthrinse may decrease the bacterial load in the mouth, thereby reducing the likelihood of transient bacteremia. This step should be considered before treating individuals with Marfan syndrome.
Hirota et al14 reported that patients with Marfan syndrome should be carefully monitored when a local anesthetic containing the vasoconstrictor epinephrine is administered. This study showed that epinephrine enhanced cardiac output, even at the low concentrations found in local anesthetic solutions.14 When administering epinephrine, patients with Marfan syndrome should be treated under the same protocols used for patients with cardiovascular disease. Among patients taking atenolol—a medication that treats high blood pressure—there are no such concerns regarding the use of local anesthetic solutions with epinephrine.6
Patients with Marfan syndrome may need multiple extractions in a single appointment under general anesthesia because of extensive crowding of the teeth and the presence of supernumerary teeth. Individuals with Marfan syndrome are at increased risk for mortality and morbidity under general anesthesia.1,2 Difficulties in intubating these patients have also been reported because of narrow airways and high palatal vault.1 Hence, dental professionals should conduct a thorough preoperative assessment, and consult with the patient’s cardiologist and an experienced anesthesiologist before administering general anesthesia to this population.1,2
According to Hirota et al,14 the inhalation of 40% nitrous oxide yielded psychosedation and stabilization of blood pressure in a patient with Marfan syndrome. Nitrous oxide may reduce or prevent undesirable hemodynamic changes that may be induced by stressors such as pain, anxiety, and fear during dental treatment.14 As such, nitrous oxide sedation can be safely used during dental treatment with standard precautions, and has been demonstrated to stabilize blood pressure in patients with Marfan syndrome.
The beta receptor blocker or ARB medications used by individuals with Marfan syndrome can cause orthostatic hypotension—a sudden and marked decrease in blood pressure when their position in the dental chair is changed abruptly.6 For this reason, adjusting the position of the dental chair should be done slowly and patients should be asked to sit upright for a few minutes before rising.6
A major drug interaction is possible when nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen and naproxen sodium, are prescribed to patients with Marfan syndrome who also take a beta blocker or ARB prophylaxis.6 NSAIDs can decrease the action of beta blockers or ARBs if used together for more than 5 days.6 Dental professionals should make sure that patients taking atenolol are not prescribed NSAIDs for more than 5 days. Also, patients should be educated about the drug interaction, as they will be using a beta-1 blocker or ARB throughout their lifetime.
Xerostomia is less frequently reported with beta blockers and ARBs.6 However, the flow of saliva should be assessed during the intraoral examination, and appropriate recommendations should be provided with oral hygiene instructions on an individual basis.
Precautions should be taken for positioning patients with glaucoma.15 The patient’s head should be placed higher than the feet throughout the treatment procedure because tilting back may cause pain and pressure in the eyes.15 The dental light should be positioned so that it does not glare into the patient’s eyes, as many ophthalmic conditions cause sensitivity to light.15 Oral hygiene instructions should be given slowly and face-to-face, as patients with ophthalmic disorders may have limited or no peripheral vision.15
A slight tendency toward bleeding was reported in a few patients with Marfan syndrome. De Coster et al3 detected a slight separation of the middle layer of blood vessels (tunica media) and dilation of blood vessels in the pulp and gingiva among patients with Marfan syndrome. However, there is no evidence to support an association between the condition and excessive bleeding. Nevertheless, dental professionals should take this into consideration, and be able to achieve hemostasis in the event of excessive bleeding during surgical procedures.
CONCLUSION
Marfan syndrome is an inherited connective tissue disorder with numerous manifestations in multiple organ systems with variable expressivity, but mainly affecting the heart, eyes, and skeleton.1–5,7,8,9,10,14,16 Affected individuals are usually tall and thin with long limbs, fingers, and toes and elongated faces.1,2,4,8 The most serious, progressive complication is aortic dissection/rupture, which is common in undiagnosed individuals.1–5,7,8,9,10,14,16 There is no cure for Marfan syndrome; however, early diagnosis and treatment are critical for preventing or delaying complications.1,2,4
Marfan syndrome exerts a myriad of dental problems that manifest at an early age. Oral health professionals are well positioned to note the early signs and symptoms of this condition and can play a significant role in identifying undiagnosed individuals and referring them for definitive diagnosis and treatment.
Oral health professionals are an important part of the multidisciplinary team that identifies and manages complications caused by Marfan syndrome, as they provide preventive dental therapy and carefully treat dental conditions. They also address esthetic concerns, thereby contributing to patients’ quality of life. However, more awareness of the syndrome is necessary to effectively manage the oral health conditions of patients with Marfan syndrome that will contribute to their overall quality of life.
REFERENCES
- Child AH, Briggs M, eds. The Marfan Syndrome, A Clinical Guide. London: British Heart Foundation; 2002.
- Marfan Trust. Dental aspects of Marfan syndrome-Information for dentists. Available at: marfantrust.org. Accessed May 6, 2014.
- De Coster PJ, Martens LC, De Paepe A. Oral manifestations of patients with Marfan syndrome: a case-control study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;93:564–572.
- Tsang AK, Taverne A, Holcombe T. Marfan syndrome: a review of literature and case report. Spec Care Dentist. 2013;33:248–254.
- Ammash NM, Sundt TM, Connolly HM. Marfan syndrome—diagnosis and management. Curr Probl Cardiol. 2008;33:7–39.
- Weinberg MA, Westphal Theile CM, Fine JB. Oral Pharmacology for the Dental Hygienist. 2nd ed. Upper Saddle River, NJ: Pearson Education Inc; 2008.
- Detaint D, Aegerter P, Tubach F, et al. Rationale and design of a randomized clinical trial (Marfan Sartan) of angiotensin II receptor blocker therapy versus placebo in individuals with Marfan syndrome. Arch Cardiovas Dis. 2010;103:317–325.
- Marfan Trust. Psychosocial Aspects of Marfan Syndrome—Information for Child Psychiatrists and Child Psychologists. Available at: marfantrust.org. Accessed May 6, 2014.
- Staufenbiel I, Hauschild C, Kahl-Nieke B, et al. Periodontal conditions in patients with Marfan syndrome—a multicenter case control study. BMC Oral Health. 2013;13:59.
- Straub AM, Grahame R, Scully C, Tonetti MS. Severe periodontitis in Marfan’s syndrome: a case report. J Periodontol. 2002;73:823–826.
- Shiga M, Saito M, Hattori M, et al. Characteristic phenotype of immortalized periodontal cells isolated from a Marfan syndrome type 1 patient. Cell Tissue Res. 2008;331:461–472.
- American Dental Association. American Heart Association Issues New Guidelines for Preventing Infective Endocarditis. Available at: ada.org/3146.aspx. Accessed May 6, 2014.
- The Marfan Foundation. Endocarditis Prophylaxis for People with Marfan Syndrome. Available at: marfan.org/resource/fact-sheet/endocarditis-prophylaxis-people-marfan-syndrome#.Ux3I_vldWa8. Accessed May 6, 2014.
- Hirota Y, Sugiyama K, Niwa H, Matsuura H. Systemic management of Marfan’s syndrome during dental treatment: a case report. Anesth Pain Control Dent. 1993;2:162–170.
- Wilkins EM. Clinical Practice of the Dental Hygienist. 11th ed. Philadelphia: Lippincott Williams & Wilkins; 2013.
- Ting BL, Mathur D, Loeys BL, Dietz HC 3rd, Sponseller PD. The diagnostic value of the facial features of Marfan syndrome. J Child Orthop. 2010;4:545–551.
From Dimensions of Dental Hygiene. June 2014;12(6):48–52.



