
Partial Denture Care
A well-designed appliance, regular maintenance visits, and meticulous home care are key to ensuring long-term periodontal health in patients with removable partial dentures.
This course was published in the August 2010 issue and expires 8/31/13. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Discuss the tenets of good removable partial denture (RPD) design.
- Understand how to minimize tooth mobility in patients with RPD appliances.
- Understand how to minimize plaque retention in patients with RPD appliances.
- Describe the dental hygienist’s role in maintaining the oral health of patients with RPD appliances.
- Provide patients with instructions about how to care for their RPD appliances.
Applicance Design
The goal of RPD fabrication is to construct a prosthesis that provides long-term function while supporting the ongoing health of oral structures. To meet this goal, the prosthesis must be able to withstand the patient’s biting forces, which fall into three categories: vertical dislodging forces, horizontal-lateral forces, and vertical seating forces. A successful RPD appliance provides retention, stability, and support to counteract these forces.
Different parts of the RPD appliance offer the resistance needed to provide retention, stability, and support. Retention resists vertical forces and is achieved with the placement of direct retainers and indirect retainers on the prosthesis. Stability resists horizontal, lateral, and torsional forces and is provided by minor connectors, proximal plates, rigid portions of clasps, lingual plates, rests, and denture bases. Support resists vertical seating forces and is accomplished with rests, major connectors, and the denture base (Figure 1).
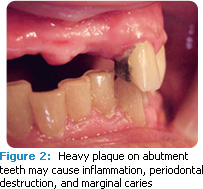
The tissue supporting the prosthesis should also be considered. The RPD appliance must be designed to limit the retention of plaque and damage to oral tissue. Studies show that plaque index scores of RPD abutment teeth are higher than those of nonabutment teeth.7,8 This suggests a correlation between wear of the RPD appliance and biofilm accumulation. The covering of marginal gingival tissue by the RPD appliance may contribute to plaque accumulation and gingival inflammation of abutment teeth (Figure 2).9 An open, more hygienic design may minimize adverse effects on remaining teeth and periodontium.9,10 The use of larger RPD embrasures is also helpful in minimizing plaque retention.2
Minimizing Tooth Mobility
In toothborne prostheses, occlusal forces are transferred to abutment teeth through occlusal rests. With ideal design, these forces are directed parallel to the long axis of the abutment tooth, minimizing tipping or torquing forces that might contribute to the mobility of the abutment tooth over time.
In RPD appliances where the occlusal load of distal extension is borne by the edentulous ridge, it is important to minimize the movement of extension bases. The more intimate the interface between the denture base and edentulous ridge, the better support the ridge provides. This close adaptation decreases forces on abutment teeth.7 Potential residual ridge resorption should be monitored closely, and distal extension RPD bases should be relined as needed to maintain optimal distribution of forces.
Caries Incidence
Just as plaque retention and periodontitis are related, so are RPD abutment teeth and dental caries. The risk of root caries is significantly increased when an RPD appliance shows signs of wear.2,11 Tooth surfaces with attachment loss that are in contact with RPD components are at particular risk. Regular application of topical fluoride is recommended to prevent caries in these areas.2
RPD Materials and Plaque Retention
For a biofilm to be viable, the component microorganisms must adhere to the associated environmental surfaces. In RPD appliances, the amount of biofilm adhesion is related to the type of material used in its design. Different artificial tooth materials have different levels of bacterial adherence. Polymethyl methacrylate (PAMA) teeth have a lower level of Streptococcus mutans adherence while artificial teeth made of filler-supplemented resin have a higher level of bacteria adhesion.12 As such, the use of PAMA material may be the best choice.
To minimize plaque retention, the following principles should be considered in the creation of an RPD:
- An open, hygienic design
- Minimized contact with gingival tissues
- Use of PAMA acrylic resin denture teeth
- Well-fitting distal extension denture bases
- Well-adjusted clasps for optimal retention, resistance, and stability
- Regular topical fluoride application on abutment teeth
Importance of Oral Health Maintenance
Although the design of the RPD is important, it alone cannot prevent plaque accumulation. Research indicates that RPD wear contributes to periodontitis in patients with poor oral hygiene who infrequently visit an oral health care provider.13 Adequate plaque control and regular recare visits, including reinforcement of oral health care instruction, scaling and root planing where appropriate, and appliance maintenance, are critical to preserving the health of abutment teeth.2,7,9 The most significant predictor of periodontal destruction of abutment teeth is the delay of maintenance intervals beyond 6 months.7,9 The remaining dentition must be evaluated for potential caries and residual alveolar ridge resorption.
The dental hygienist plays an important role in the prevention process by monitoring and maintaining the patient’s oral health. This is achieved by assessing the patient for the following problems:1
- Signs of intraoral tissue trauma related to the RPD appliance
- Increased mobility of abutment teeth
- Poor adaptation of RPD clasps
- Residual ridge resorption and resulting space between the ridge and the denture base
- Presence of decalcification or caries, particularly in abutment teeth
Patient education and motivation to care for both the RPD appliance and remaining teeth are imperative for long-term success of the RPD (see sidebar for a list of patient instructions). The periodontal maintenance interval must be evaluated and adjusted to help the patient prevent the deleterious effects of plaque accumulation on the periodontium, and protect the health of the abutment teeth. Patient comfort is also important to consider. Mouth irritations caused by RPD appliances can be treated with agents designed to oxygenate and cleanse wounds. Any resulting pain can be addressed with products that provide an anesthetic effect to oral tissues.
Periodic Maintenance
Regular recare visits for patients with RPD appliances are crucial to maintaining oral health. At the recare visit, dental hygienists need to: review the health and dental history; perform an intraoral/extraoral soft tissue examination; take radiographs if needed; remove calculus and plaque; review home care instructions; and assess the RPD for stability, retention, and function. Table 1 provides a list of important points to consider when performing an assessment.
Conclusion
A well-constructed RPD appliance supported by sound abutments, a regular periodontal maintenance program, and impeccable selfcare will minimize the risk to existing periodontal health in patients with RPD appliances.1 The dentist, dental hygienist, and patient must work together to ensure the success of this treatment modality. Careful prosthetic treatment planning, consistent oral hygiene instruction, good oral hygiene, and regular recare visits are vital to the longterm health of the tissues and teeth that support the RPD appliance.
References
- Umar S. Use of removable partial dentures and progression of periodontal disease. Canadian Journal of Dental Hygiene. 2009;43(3):113-116.
- Mine K, Fueki K, Igarashi Y. Microbial risk for periodontitis of abutment teeth in patients with removable partial dentures. J Oral Rehabil. 2009;36:696-702.
- Carr AB, McGivney GP, Brown DT. McCracken’s Removable Partial Prosthodontics. 11th ed. St. Louis: Elsevier Mosby; 2005:243-244, 370-371.
- Grasso JE, Miller EL. Removable Partial Prosthodontics. 3rd ed. St. Louis: Mosby; 1991:254-262.
- Kratochvil FJ. Partial Removable Prosthodontics. Philadelphia: W.B. Saunders Co; 1988:164-167.
- Phoenix RD, Cagna DR, DeFreest CF. Stewart’s Clinical Removable Partial Prosthodontics. 4th ed. Hanover Park, Ill: Quintessence Publishing Co; 2008:443-445, 456.
- Jorge JH, Giampaolo ET, Vergani CE, Machado AL, Pavarina AC, Cardoso de Olivaera MR. Clinical evaluation of abutment teeth of removable partial denture by means of Periotest method. J Oral Rehabil. 2007;34:222-227.
- Zlataric DK, Celebic A, Valentic-Peruzovic M. The effects of removable partial dentures on periodontal health of abutment and non-abutment teeth. J Periodontol. 2002;73:137-144.
- Yeung ALP, Lo ECM, Chow TW, Clark RKF. Oral health status of patients 5-6 years after placement of cobalt-chromium removable partial dentures. J Oral Rehabil. 2000;27:183-189.
- Owall B, Budtz-Jorgensen E, Davenport J, et al. Removable partial denture design. Int J Prosthodont. 2002;15:371-377.
- Budtz-Jörgensen E. Restoration of the partially edentulous mouth—a comparison of overdenture, removable partial dentures, fixed partial dentures and implant treatment. J Dent. 1996;24:237-244.
- Hahnel S, Rosentritt M, Burgers R, Handel G. Adhesion of streptococcus mutans NCTC 10449 to artificial teeth: an in vitro study. J Prosthet Dent. 2008;100:309-315.
- Kern M, Wagner B. Periodontal findings in patients 10 years after insertion of removable partial dentures. J Oral Rehabil. 2001;28:991-997.
From Dimensions of Dental Hygiene. August 2010; 8(8): 16-19.






