Optical Coherence Tomography
This advanced imaging technology may help improve treatment outcomes, as well as support patient education.
In dentistry, optical coherence tomography (OCT), a type of digital imaging, is used to support patient diagnosis, treatment planning, and education. Providing a localized image in a real-time setting, this technique can be used to detect caries, support the diagnosis of periodontal diseases, indicate tooth fractures, evaluate the margins of oral lesions, and measure cavity preparations for restorations created by computer-aided design/computer-aided manufacturing (CAD/CAM) technology.
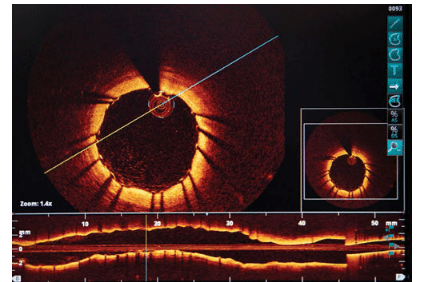
OCT was developed into a cross-sectional imaging modality in medicine by Huang et al1 in 1991. The imaging technique was first applied in ophthalmology with a focus on the retina, optic nerve, and coronary arteries.1 In 1997, Sergeev et al2 presented OCT applications in vivo for the respiratory mucosa, gastrointestinal, urinary, and genital tracts. Today, OCT is used in the diagnosis and treatment of glaucoma, during guided surgical procedures, and for intracoronary imaging (Figure 1).
OCT was first used in dentistry during the late 1990s. Baumgartner et al3 used the technique to better understand the cross-sectional imaging of dental structures. In 2000, Otis et al4 described the use of OCT in imaging hard and soft tissues, as well as restorative materials. In 2002, the United States Food and Drug Administration approved the use of OCT in dentistry.5
OCT produces images in a three-dimensional (3D) format. In comparison to two-dimensional radiography with its limited contrast and resolution, dental OCT offers improved resolution and increased contrast among areas of examination.6 OCT uses electromagnetic radiation, which does not emit the same type of mutagenic interaction as do traditional radiographs.7
TECHNIQUE
An OCT unit consists of a small, wand-like apparatus with a tip that is used to acquire a specific image. For an image to be produced within the unit, a broadband light source is released and then separated, with one light source directed to a mirror and the other pointed to the specified area in the oral cavity. A reflection is then created from the mirror and the tissue of the oral cavity. This reflection is recombined at the original splitter to produce a transmission that is sent to a receptor. The receptor configures the transmission and creates an image of the dental tissue via the computer.6 As with digital radiography, computer software enables manipulation of the image for optimal viewing.
CLINICAL APPLICATIONS
OCT can be a valuable tool for the early detection of demineralization due to decay.6 Its use can be particularly helpful in evaluating the occlusal surfaces of posterior teeth, which are some of the most difficult areas to assess for caries. What may appear as a stain could actually be the early progression of caries. During a clinical exam, the use of an explorer may not be adequate for the detection of early caries lesions. Because of their limited resolution and contrast, traditional radiographs may not indicate this initial progression of demineralization. OCT provides a real-time image of the specific area in a more detailed format. The presentation of this image enables the dental team to better evaluate the area for specific treatment. OCT can also help determine if recurrent decay is present after placement of restorations. Fractures within the tooth can be better examined, as well.8
Oral health professionals can also use OCT to ensure the success of sealants. As the surfaces to be sealed must be free of early demineralization, OCT can be used to further evaluate the tooth surface and verify that demineralization is not present.9 It may also be helpful after sealant or restoration placement to determine whether recurrent decay is present, as OCT can provide good visualization of a restoration’s margin. In some instances, caries can progress under a sealant. OCT provides an enhanced view of questionable areas that may not be seen visually or radiographically.
Periodontal health status can be further evaluated with OCT. Probing depths, clinical visualization, and radiographs are key contributors to the assessment of patients’ periodontal health. Bone height and periodontal ligament structure may be altered, yet not interpreted due to limited accessibility to these areas. Traditional radiography may not demonstrate the bone loss on one side of the dentition due to the superimposition of one bone surface being higher than the other.10 OCT allows the 3D examination of alterations in the bone structure to determine where periodontal issues are specifically occurring.
The use of OCT may also aid in the detection of oral cancers.6 It can provide information about the stage of a tumor, including premalignant and malignant status. OCT can also assist in determining the extent of a lesion through improved contrast capabilities and the opportunity to evaluate the image in 3D.6 The recurrence risk and predictors of tumor response once treatment begins can also be examined with this technology.6
New studies are looking at the use of OCT to obtain impressions from intraoral preparations, which would help the creation of indirect restorations with CAD/CAM machines.11 After the preparation is complete, an OCT unit scans the tooth, depicts the margins of the preparation, and sends the image to the CAD/CAM machine for immediate fabrication of the restoration. This technology would eliminate the need for impressions, which are often cumbersome, messy, and time-consuming, while also reducing the cost of materials.
PATIENT EDUCATION
Patient education could also be enhanced through the use of OCT. Charting of probing depths, intraoral photos, and radiographic images are all used to educate patients about the presence of periodontal diseases and the treatment plan. Providing an enhanced 3D image further educates patients about their present condition and helps focus on specific areas that may not be visually seen on radiographs. Analyses of both bone and the periodontal ligament could help patients understand the importance of the attachment apparatus. This imaging may assist oral health professionals better explain surgical vs nonsurgical treatment.
As the number of older adults in the US continues to increase, more patients will present to the dental office with their natural dentition intact. The use of OCT may encourage older adults to adhere to proposed treatment plans to help them avoid tooth loss. Many patients are more likely to agree to treatment and comply with the suggested regimen when enhanced visual aids are used.
OCT’s ability to provide the dental team with different vantage points and enhanced imaging supports definitive diagnosis and treatment planning. Although this modality has been available in the dental setting for the past few years, OCT’s use in dentistry has not reached its full potential. As with any new technology, gradual improvements are being made to boost image quality and reduce cost so OCT can be implemented more easily into private dental practice.
REFERENCES
- Huang D, Swanson EA, Lin CP, et al. Optical coherence tomography. Science. 1991;254:1178–1181.
- Sergeev A, Gelikonov V, Gelikonov G, et al. In vivo endoscopic OCT imaging of precancer and cancer states of human mucosa. Opt Express. 1997;1:432–440.
- Baumgartner A, Dichtl S, Hitzenberger CK, et al. Polarization-sensitive optical coherence tomography of dental structures. Caries Res. 2000;34:59–69.
- Otis LL, Everett MJ, Sathyam US, Colston BW Jr. Optical coherence tomography: a new imaging technology for dentistry. J Am Dent Assoc. 2000;131:511–514.
- United States Food and Drug Administration. Introduction to optical coherence tomography (OCT) technology: time-domain and spectral-domain including similarities and differences between these technologies. Available at: fda.gov/downloads/MedicalDevices/NewsEvents/WorkshopsConferences/UCM326717.pdf. Accessed May 22, 2014.
- Hsieh Y, Ho YC, Lee SY, et al. Dental optical coherence tomography. Sensors. 2013;13:8928–8949.
- Azevedo CS, Trung LC, Simionato MR, Freitas AZ, Matos AB. Evaluation of caries-affected dentin with optical coherence tomography. Braz Oral Res. 2011;25:407–413.
- BioOptics World. Optical coherence tomography/dentistry: driving OCT into dentistry. Available at: bioopticsworld.com/articles/ print/volume-7/issue-1/features/optical-coherence-tomography-dentistry-driving-oct-into-dentistry.html. Accessed May 22, 2014.
- Holtzman JS, Osann K, Pharar J, et al. Ability of optical tomography to detect caries beneath commonly used sealants. Lasers Surg Med. 2010;42:752–759.
- Freitas AZ, Zezell DM, Vieira ND Jr, Ribeiro AC, Gomes ASL. Imaging carious human dental tissue with optical coherence tomography. Journal of Applied Physics. 2006;99(2):024906.
- Chityala R, Vidal C, Jones R. Utilizing optical coherence tomography for CAD/CAM of indirect dental restorations. SPIE Proceedings. 2013;8566.
From Dimensions of Dental Hygiene. June 2014;12(6):24–25.

