 DRAZEN_/E+/GETTY IMAGES PLUS
DRAZEN_/E+/GETTY IMAGES PLUS
The Mysteries of Noncarious Cervical Lesions
The etiology of these lesions remains unknown, but clinical judgment and documentation of signs and symptoms can help clinicians determine an appropriate course of action.
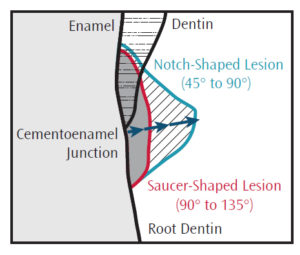
Noncarious cervical lesions (NCCLs) are small saucer-shaped or notch-shaped losses of tooth structure at the cementoenamel junction that present most often on the facial surface of teeth (Figure 1). These lesions are not at increased risk of caries because they are generally accessible for self and professional cleaning. NCCLs generally present in middle-aged to older adults, with highly variable prevalence ranging from 5% to 90%.1–5
Evidence shows that the etiology of NCCLs is multifactorial. Abfraction due to occlusal stress, erosive tooth wear, or a combination of factors are all possible etiologies of NCCLs.6,7 While NCCLs don’t necessarily require restoration, patients typically seek treatment based on a desire for improved esthetics. The decision to restore and/or manage NCCLs depends on the theory assumed responsible for their origin.8
Originally, NCCLs were attributed solely to excessive abrasion caused by harsh toothbrushing and/or the use of abrasive dentifrices. On their own, toothbrushes do not produce mechanical damage during brushing; however, excessive brushing force and highly abrasive toothpastes can cause permanent wear of dentin.9 Generally, this problem is associated with poor oral hygiene methods, such as horizontal brushing technique along the cervical margins of teeth in line with the margins of gingival tissue. While brushing with too much force and using an abrasive toothpaste may seem logical causes of NCCLs, several factors shed doubt on these explanations. NCCLs often appear on a single tooth, which is difficult to produce with brushing motions. Additionally, NCCLs have been observed in a nonbrushing population of lepers who experienced acidic food exposures, parafunction, and some xerostomia.10 NCCLs have also been noted in some ancient teeth found in archeological digs from five different geographical sites.11 NCCLs are not generally sensitive, which seems counterintuitive if they were caused by continued abrasion of the dentin.2
A second theory is that NCCLs are caused by the tensile stress created by occlusion. Although this theory was first described in 1984,12 it did not receive much attention until 1991, when Grippo coined the term “abfraction” to describe this phenomenon.13Abfractions are presumed to arise in the presence of heavy working contacts and associated occlusal stresses.14,15 Teeth under stress involve compression on lingual surfaces and tension on buccal surfaces. Tension leads to micromorphological fatigue and contributes to loss of superficial tooth structure during mastication and/or brushing. Tooth stresses occur during normal occlusion, but are greater during malocclusion. This often results in occlusal wear facets.
Several thousand loading cycles occur each day during chewing and swallowing, causing small amounts of fatigue damage that accumulates over years. The first visual evidence is a saucer-shaped lesion. NCCLs occur on facial surfaces because the normal loading of teeth causes flexure patterns with tension on the facial surface. This process, however, has not been well documented.6,16,17 While artificial lesions can be produced in the laboratory, there has been no monitoring of lesion development over an extended period due to the high cost of this type of clinical trial.
Erosion is an etiologic factor in the development of NCCLs. Erosion is the degradation of tooth structure due to physicochemical action of acidic or corrosive agents.18,19 There are two basic categories of erosion: intrinsic and extrinsic. Lesions from extrinsic erosion tend to occur on the labial surfaces of the anterior teeth and buccal or occlusal surfaces of the posterior teeth.20 Extrinsic erosion is caused by the regular exposure to acidic foods and beverages. Many foods and beverages have low pH, including soft drinks, sports drinks, fruits, juices, vinegar, salad dressing, and white wine.21 Erosion softens the surface enamel, which, when subjected to abrasion or abfraction, causes further progression of the lesion. The main signs are cupping of cusp tips, loss of dental anatomy, and restorations “standing proud” due to the erosive loss of enamel surrounding the restoration. Early signs of erosion must be recognized so successful preventive strategies can be initiated and the necessity for extensive, expensive restorative care can be avoided.
It is equally possible that components of these theories occur together, risk levels change over time, or other events.1 If superficial tooth structure is weakened by micromorphological fractures and erosion, then toothbrush (and dentifrice) abrasion can contribute to the ultimate loss of that material. The very nature of NCCLs makes them difficult to study because the etiology of NCCLs may be different from the factors that cause their progression.
CLINICAL CONSIDERATIONS
The way NCCLs are restored and managed depends on their etiology. If the patient presents with many NCCLs adjacent to each other, some dentinal hypersensitivity, and a horizontal toothbrushing pattern, toothbrush abrasion is likely the cause.
Treatment and management for lesions caused by abfraction require more care. If patients present with lesions on single teeth, obvious wear facets, and/or no hypersensitivity, abfraction may be the cause. In this case, modification of the existing occlusion should be considered prior to restoration of NCCLs. One option is to improve anterior guidance with crowns or veneers, thus eliminating or reducing lateral excursive contacts on posterior teeth. A thorough risk/benefit analysis must be performed before this treatment is initiated. The impact of using nightguards and bite splints to reduce the risk of NCCLs among those with malocclusion has not yet been reported in the literature. However, these treatments would not necessarily affect normal daytime occlusal patterns or stresses.
If the clinical signs point toward erosion as the primary etiology, then the nature of erosion—intrinsic vs extrinsic—will determine the treatment. In the case of lesions on facial surfaces due to extrinsic erosion, a diet analysis is necessary. The key is to provide the patient with an effective protocol to avoid acidic challenges or minimize erosive tooth wear after an acidic challenge. Such an approach may include rinsing with water, followed by rinsing with sodium bicarbonate and an over-the-counter fluoride mouthrinse. Eating cheese after an acidic challenge is useful because this stimulates salivary flow rates and buffering capacity, and the relatively high pH of cheese (6 to 7.4) helps neutralize acidity.22 Thorough care must be taken to implement successful preventive strategies so that extensive, expensive restorative care can be avoided.
RESTORATIVE CARE
If the lesions are esthetically displeasing, become detrimental to pulp health, or if the patient experiences dentinal hypersensitivity, then NCCLs should be restored. The goal is to relieve or eliminate the events contributing to NCCL formation so the lesions do not return after restoration.18 Evidence suggests a material with a low elastic modulus that will accommodate the tooth flexure—such as microfilled, nanohybrid, or nanofilled composite resin, glass ionomer, or resin modified glass ionomer—may be desirable for restoring NCCLs.23 The restoration of NCCLs may involve a regular composite, a low modulus composite, a flowable composite, or a flowable composite liner. Low modulus materials or liners are intended to accommodate tooth flexure; however, the evidence does not show the use of these materials to be necessary.24 Generally, the enamel margins of the lesion are roughened with a flame-shaped diamond to ensure a bevel exists. Staining or leakage along the composite border may become difficult to remove during hygiene procedures. Placing mechanical retention in preparation to restore NCCLs and not relying on adhesives alone should be considered. If the tooth is being crowned, a porcelain-fused-to-metal crown or all-ceramic crown could be extended to include the boundaries of the lesion. If there are occlusal stresses contributing to an abfraction and they persist, the lesions will become refocused at the border of the crown and begin to produce a more apical NCCL. The tooth can be removed from occlusion at the obvious contacts to reduce stress. The occlusion could be shifted from group function to canine guidance. However, most of these effects are temporary.
Generally, NCCLs are not sensitive. The slow progression of NCCLs provide enough time for a vital pulp to lay down sclerotic dentin and naturally occlude the dentinal tubules, thus preventing rapid fluid movement and dentinal hypersensitivity. These surfaces should not be disturbed by explorers, manual scalers, or power scalers during normal hygiene procedures.
All NCCLs should be clinically recorded with photographs of the presence, shape, and relative size of the lesions on facial surfaces, as well as any clues to their presence, such as occlusal wear facets on teeth. A periodontal probe can be used to estimate the widths and depths of tooth surface NCCLs. Comparison of diagnostic casts fabricated from impressions made at different intervals over a few years may also be a valuable diagnostic tool.
NCCLs can arise from toothbrush (and dentifrice) abrasion, abfractions, erosive tooth wear, or multifactorial situations. They are restored for reasons of esthetics, dentinal hypersensitivity, and for pathological progression toward a vital pulp. Generally, tooth stresses need to be mitigated to reduce or eliminate factors contributing to their continued development.
REFERENCES
- Levitch LC, Bader JD, Shugars DA, Heymann HO. Non-carious cervical lesions. J Dent. 1994;22:195–207.
- Aw TC, Lepe X, Johnson GH, Mancl L. Characteristics of noncarious cervical lesions: a clinical investigation. J Am Dent Assoc. 2002;133:725–733.
- Borcic J, Anic I, Urek MM, Ferreri S. Prevalence of non-carious cervical lesions in permanent dentition. J Oral Rehabil. 2004;31:117–123.
- Pegararo LF, Scolaro JM, Conti PC, Telles D, Pegararo TA. Non-carious cervical lesions in adults—prevalence and occlusal aspects. J Am Dent Assoc. 2005;136:1694–1700.
- Lai ZY, Zhi QH, Zhou Y, Lin HC. Prevalence of non-carious cervical lesions and associated risk indicators in middle-aged and elderly populations in Southern China. Chin J Dent Res. 2015;18:41–50.
- Bartlett DW, Shah P. Critical review of non-carious cervical (wear) lesions and the role of abfraction, erosion, and abrasion. J Dent Res. 2006;85:306–312.
- Wood I, Jawab Z, Paisley C, Brunton P. Non-carious cervical tooth structure loss: a literature review. J Dent.2008;36:759–766.
- Nascimento MM, Dilbone DA, Pereira PN, Duarte WR, Geraldeli S, Delgado AJ. Abfraction lesions: etiology, diagnosis, and treatment options. Clin Cosmet, and Investig Dent. 2016;8:79–87.
- Dzakovich JJ, Oslak RR. In vitro reproduction of noncarious cervical lesions. J Prosthet Dent. 2008;100:1–10.
- Faye B, Kane AW, Sarr M, Lo C, Ritter AV, Grippo JO. Non-carious cervical lesions among a non-toothbrushing population with Hansen’s disease (leprosy): initial findings. Quintessence Int. 2006;37:613–619.
- Ritter AV, Grippo JO, Coleman TA, Morgan ME. Prevalence of carious and non-carious cervical lesions in archaeological populations from North America and Europe. J Esthet Restor Dent. 2009;21:324–334.
- Lee WC, Eakle WS. Possible role of tensile stress in the etiology of cervical erosive lesions of teeth. J Prosthet Dent. 1984;52:374–380.
- Grippo JO. Abfractions: a new classification of hard tissue lesions of teeth. J Esthet Restor Dent. 1991;3(1):14–19.
- Braem M, Lambrechts P, Vanherle G. Stress-induced cervical lesions. J Prosthet Dent. 1992;67:78–722.
- Sawlani K, Lawson NC, Burgess JO, et al. Factors influencing the progression of noncarious cervical lesions: a 5-year prospective clinical evaluation. J Prosthet Dent. 2016;115:571–577.
- Michael JA, Townsend GC, Greenwood LF, Kaidonis JA. Abfraction: separating fact from fiction. Aust Dent J. 2009;54:2–8.
- Senna P, Del Bel Cury A, Rosing C. Non-carious cervical lesions and occlusion: a systematic review of clinical studies. J Oral Rehabil. 2012;39:450–462.
- Lussi A, Jaeggi T. Dental Erosion—Diagnosis, Risk Assessment, Prevention, and Treatment. Hanover Park, Illinois: Quintessence Publishing; 2011.
- Lussi A, Schaffner M. Progression of and risk factors for dental erosion and wedge-shaped defects over a 6-year period. Caries Res. 2000;34:182–187.
- Nunn JH. Prevalence of dental erosion and the implications for oral health. Eur J Oral Sci. 1996;104:156–161.
- Jarvinen VK, Rytomaa, II, Heinonen OP. Risk factors in dental erosion. J Dent Res. 1991;70:942–947.
- Honório HM, Rios D, Júnior ES, de Oliveira DS, Fior FA, Buzalaf MA. Effect of acidic challenge preceded by food consumption on enamel erosion. Eur J Dent. 2010;4:412–417.
- Heymann HO, Sturdevant JR, Bayne S, Wilder AD, Sluder TB, Brunson WD. Examining tooth flexure effects. J Amer Dent Assoc. 1991;122:41–47.
- Heymann HO, Bayne SC. Current concepts in dentin bonding. J Am Dent Assoc. 1993;124:26–36.
From Dimensions of Dental Hygiene. March 2017;15(3):18, 21-23.

