
Musculoskeletal Health: When to Seek Professional Help
Oral health professionals should understand the common signs and symptoms of musculoskeletal health problems and when intervention is needed.
According to the National Institute for Occupational Safety and Health, work-related musculoskeletal disorders are common and may result in pain, limited motion, and weakness in the spine and extremities.1 Dental hygienists are susceptible to musculoskeletal pain, especially in the neck, shoulder, and hand/wrist regions.2,3 It is believed that awkward, prolonged working posture—such as bending, reaching, and standing—contribute to these conditions.4,5 Like other health care professionals, dental hygienists experience psychological stress and anxiety at work.6,7 Studies suggest that the psychological stress experienced by dental hygienists is related to musculoskeletal symptoms.6,8 Studies on oral health professionals found that 58% of dentists have experienced headaches and dental hygienists may also be susceptible to tension headaches due to the nature of their work.9,10
Though prevention of musculoskeletal pain is preferred, sometimes pain and dysfunction are unavoidable. Dental hygienists should learn to recognize the common signs and symptoms associated with these pathologies. Better awareness of musculoskeletal problems and their treatments may result in improved long-term outcomes. Research has demonstrated that individuals who seek early intervention for musculoskeletal pain are eight times less likely to develop chronic pain.11
COMMON MUSCULOSKELETAL PROBLEMS
Muscle pain, or myalgia, is a common condition that affects most people at some point. It can vary from mild aches to severe, incapacitating muscle spasms.12 A muscle spasm is an involuntary contraction of one or more muscles. Muscle spasms are frequently referred to as “muscle cramps,” which may be related to dehydration, poor circulation, or lack of minerals in the diet. However, muscle spasms are also the result of overuse and excessive strain of the muscle unit.13 The prolonged standing and awkward reaching postures commonly performed by dental hygienists, for example, may result in muscle tension in the spine and neck areas.
Tendonitis occurs when there is inflammation of the muscle tendon, or the muscle’s attachment to the bone. It often happens after excessive, repetitive motions such as gardening, painting, and playing tennis. It is common in the upper extremities, especially the base of the thumb, elbow, and shoulder; although it affects the lower extremities, as well.14Tendonitis is frequently included in descriptions of cumulative trauma disorders, also known as repetitive strain injuries, which are the largest cause of occupational disease in the United States.15 Repetitive upper extremity motions routinely performed by dental hygienists may predispose this group to inflammatory conditions.
Bursitis is inflammation of the bursae, or the fluid-filled sacks in the body designed to reduce friction. Trauma to the area or excessive motion can lead to increased amounts of fluid in the bursae, causing pain. Bursitis is common in the elbow, shoulder, and hips.16 The inflamed bursae often can be palpated as a fluid-filled sack, thus distinguishing it from tendonitis. As the bursae is not directly in series with contractile tissue, the pain may not be reproduced with muscle contraction or stretching. However, the area is typically extremely sensitive to touch and these criteria help a trained clinician reach an accurate diagnosis.
According to the Arthritis Foundation, more than 50 million Americans experience some form of arthritis; it is the number one cause of disability in this country. Osteoarthritis or “wear and tear” arthritis is the most common form. Osteoarthritis results from an erosion of the normal cartilage within a joint, reducing the joint space available for normal motion. Common symptoms include morning stiffness or stiffness after prolonged rest, and pain and swelling in the joints after use. There is no specific cause of osteoarthritis; however, genetics, obesity, injury, and overuse may be contributing factors.17 The repetitive movements involved with dental hygiene practice may make these professionals more susceptible.
Fibromyalgia is a condition that can result in widespread chronic pain that frequently presents as musculoskeletal symptoms. It is not a specific disease but rather a group of symptoms that also include memory problems, fatigue, and mood changes. Unlike osteoarthritis, it does not lead to joint or muscle damage. Fibromyalgia affects nearly 4 million Americans most of whom are women between the ages of 40 and 75. Fibromyalgia is diagnosed when a certain identifiable pattern of symptoms is present, when pain has lasted at least 3 months, and when no other medical diagnosis explains these symptoms.17
Tension-type headache is the most common type of headache and affects more women than men.18,19 Research suggests that psychological stress in dental hygienists may be related to musculoskeletal pain.20,21 In addition to headache, individuals may sense tension in the neck, upper shoulders, and back.
WHEN TO TAKE ACTION
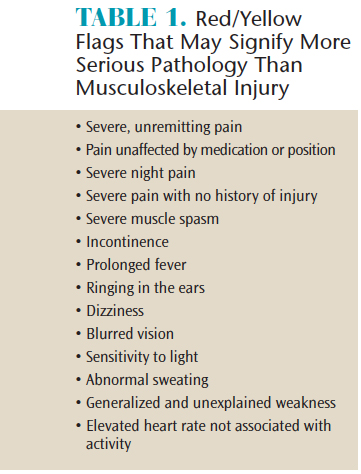
First, some serious medical conditions present as musculoskeletal pain. It is vital that individuals identify certain “red and yellow flags” that may help distinguish between typical musculoskeletal pain syndromes and serious pathology. Some of these signs and symptoms are presented in Table 1.22 Dental hygienists who experience these symptoms should seek immediate assistance from a physician or equivalent medical professional.
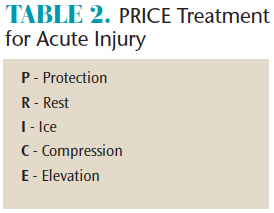
In many situations, musculoskeletal pain is self-limiting. An individual may find he/she experiences pain after excessive activity, then within a few days the symptoms have resolved. Self-treatment can be effective during this time. The “protection, rest, ice, compression, elevation” (PRICE) method is commonly employed for acute musculoskeletal injuries (Table 2).23 The procedure can begin at home or the workplace immediately after perceived symptoms and frequently will be curative for minor injuries. However, should pain, stiffness, or inflammation persist for more than a week, formal intervention may be needed. In addition, if pain is severe in the early stages of injury, individuals should seek medical attention immediately. Other considerations include more atypical symptoms, such as numbness/tingling and muscle weakness, which could be indicative of a significant soft tissue sprain or neurological involvement.
HOW TO TAKE ACTION

When dental hygienists determine the threshold has been met to seek medical assistance for musculoskeletal pain, they have multiple options. For example, they may seek help from a family physician, occupational health physician, orthopedic surgeon, nurse practitioner, physician assistant, chiropractor, massage therapist, or physical therapist. These professionals have varying levels of training and areas of expertise. In rural areas, nurse practitioners and physician assistants may be more accessible.
When dental hygienists seek help through a physician or physician extender, they will typically receive an evaluation that may include X-rays or magnetic resonance imaging (MRI). X-rays are usually included if trauma was involved or if joint space narrowing from arthritis is suspected. MRI is typically ordered to diagnose potentially serious soft tissue injuries, such as herniated discs in the spine or ligament and tendon ruptures in the extremities. Physicians, nurse practitioners, and physician assistants will typically order anti-inflammatory, muscle relaxant, or pain medications as needed. They may refer the patient for physical therapy. Physical therapists are doctoral-trained health care providers who specialize in the evaluation and treatment of movement disorders that may be related to musculoskeletal pain. In addition, physical therapists now have more extensive practice acts in every state, thus allowing patients to directly access their services without a physician referral.
According to the American Physical Therapy Association’s Guide to Physical Therapist Practice 3.0, physical therapists practice according to the Patient Client Management Model: examination, evaluation, prognosis, diagnosis, intervention, and outcomes.24Dental hygienists seeing a physical therapist for their musculoskeletal complaint should expect to be examined and have these findings evaluated by the therapist. They should receive some type of movement-related diagnosis and an associated prognosis, indicating the potential for improvement. Common physical therapy interventions include therapeutic exercise; manual therapy (Figure 1); neuromuscular reeducation; gait training; functional training; work/home reintegration; physical agents, such as therapeutic ultrasound and various forms of electrical stimulation; posture and positioning techniques; and patient education. Finally, the physical therapist should determine outcomes and whether the goals set for treatment were met. Outcomes will typically include short-term measures of pain and physical function, such as range of motion and strength. Long-term impact, such as return to functional activities and normal social roles, is considered vital as they may more closely assess quality of life.
SUMMARY
Dental hygienists are susceptible to musculoskeletal pain secondary to work-related positions and postures. Early detection and treatment may result in better long-term outcomes including decreased re-occurrence and less work absence, resulting in enhanced job satisfaction and improved work longevity. Dental hygienists should seek more knowledge of musculoskeletal pathologies in order to make informed decisions. Multiple treatment options are available to help oral health professionals improve their quality of life with daily and work-related activities if they take the initiative to seek professional help.
REFERENCES
- Cumulative Trauma Disorders in the Workplace. The National Institute for Occupational Safety and Health (NIOSH). Available at: cdc.gov/niosh/docs/95-119/default.html. Accessed October 16, 2017.
- Hayes MJ, Smith DR, Cockrell D. An international review of musculoskeletal disorders in the dental hygiene profession. Int Dent J. 2010; 60:343–352.
- Hayes M, Taylor J, Smith D. Predictors of work-related musculoskeletal disorders among dental hygienists. Int J Dent Hyg. November 14, 2011 Nov 14. Epub ahead of print.
- Marklin RW, Cherney K. Working postures of dentists and dental hygienists. J Calif Dent Assoc. 2005;33:133–136.
- Noh H, Roh H. Approach of industrial physical therapy to assessment of the musculoskeletal system and ergonomic risk factors of the dental hygienist. J Phys Ther Sci. 2013;25:821–826.
- Gorter RC. Work stress and burnout among dental hygienists. Int J Dent Hyg. 2005;3:88–92.
- Ylipaa V, Szuster F, Spencer J, et al. Health, mental well-being, and musculoskeletal disorders: a comparison between Swedish and Australian dental hygienists. J Dent Hyg. 2002;76:47–58.
- Ylipaa V, Szuster F, Spencer J, et al. Health, mental well-being, and musculoskeletal disorders: a comparison between Swedish and Australian dental hygienists. J Dent Hyg. 2002;76:47–58.
- Myers HL, Myers LB. It’s difficult being a dentist: stress and health in the general dental practitioner. Br Dent J. 2004;197:89–93.
- Tapley H. Help for tension headaches. Dimensions of Dental Hygiene. 2011;9(9):74–77.
- Linton SJ, Hellsing A, Anderson D. A controlled study of the effects of an early intervention on acute musculoskeletal pain problems. Pain. 1993;54:353–359.
- The Mayo Clinic. Muscle Pain. Available at: mayoclinic.org/symptoms/muscle-pain/basics/causes/sym-20050866. Accessed October 16, 2017.
- MedLine Plus. Muscle Cramps. Available at: https://medlineplus.gov/musclecramps.html.Accessed October 16, 2017.
- WebMD. Tendinitis. Available at: webmd.com/fitness-exercise/arthritis-tendinitis#1. Accessed October 16, 2017.
- Connecticut Department of Public Health. Cumulative Trauma Disorders Fact Sheet. Available at: ct.gov/dph/lib/dph/environmental_health/eoha/pdf/ctds_fact_sheet.pdf. Accessed on October 16, 2017.
- Mayo Clinic. Bursitis. Available at: mayoclinic.org/diseases-conditions/bursitis/home/ovc-20345506. Accessed October 16, 2017.
- The Arthritis Foundation. Osteoarthritis. Available at: arthritis.org/about-arthritis/types/osteoarthritis/. Accessed October 16, 2017.
- Crystal SC, Robbins MS. Epidemiology of tension-type headache. Curr Pain Headache Rep. 2010;14:449–454.
- Rasmussen BK, Jensen R, Schroll M, Olesen J. Epidemiology of headache in a general population: a prevalence study. J Clin Epidemiol. 1991;44:1147–1157.
- Gorter RC. Work stress and burnout among dental hygienists. Int J Dent Hyg. 2005;3:88–92.
- Ylipaa V, Szuster F, Spencer J, et al. Health, mental well-being, and musculoskeletal disorders: a comparison between Swedish and Australian dental hygienists. J Dent Hyg. 2002;76:47–58.
- Magee DJ. Orthopedic Physical Assessment. 6th ed. St. Louis: Elsevier; 2014.
- Treating Sports Injuries. Available at: health.harvard.edu/newsletter_article/treating-sports-injuries. Accessed October 16, 2017.
- The American Physical Therapy Association. Guide to Physical Therapist Practice. Available at: apta.org/Guide/. Accessed October 16, 2017.
Featured photo by SEB_RA/ISTOCK/GETTY IMAGES PLUS
From Dimensions of Dental Hygiene. November 2017;15(11):14,16,18.

