 AGSANDREW / ISTOCK / THINKSTOC
AGSANDREW / ISTOCK / THINKSTOC
Modifying Behavior to Improve Outcomes
An individualized approach to behavior modification may be the most successful in improving compliance with treatment and self-care regimens.
This course was published in the October 2016 issue and expires October 31, 2019. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Discuss why behavior modification is important to improving oral health.
- Identify the most common psychological interventions used to encourage patient behavior change.
- Explain the four interventions used to facilitate behavior change.
INTRODUCTION
be most effective in facilitating behavior change. While it is essential for patients to have good oral hygiene habits in order to maintain their oral and overall health, the task of persuading patients to adhere to self-care regimens is often difficult. The use of interactive resources, such as Colgate’s Gum Health Physical Tool (available at: gumhealthphysical.com), can help dental professionals improve the oral health of their patients.
This article reviews the most common theories and psychological interventions implemented to achieve behavior change at the individual patient level. The Colgate-Palmolive Company is delighted to have provided an unrestricted educational grant to support “Modifying Behavior to Improve Outcomes” in collaboration with the American Academy of Periodontology.
— Matilde Hernandez, DDS, MS, MBA
Scientific Affairs Manager
Professional Oral Care
Colgate Oral Pharmaceuticals
FROM THE AMERICAN ACADEMY OF PERIODONTOLOGY
When a patient comes in for a visit, the periodontist and dental hygienist are charged with providing the highest quality of care based on the patient’s individual case. But as dental professionals of all types understand, the treatment administered during an office visit can be inadequate without the patient’s commitment to consistent self-care. As such, the clinician’s role includes the reinforcement of periodontal health maintenance.
In this article, Diana Bronstein, DDS, MS, MS, takes a look at the psychology behind patient behavior and provides insights on how dentists and dental hygienists can individualize their approaches to educating patients on the value of self-care. The American Academy of Periodontology is proud to work with Dimensions of Dental Hygiene and the Colgate-Palmolive Company to bring you information that can aid in keeping your patients’ gums and smiles healthy for a lifetime.
— Wayne Aldredge, DMD
President, American Academy of Periodontology
Maintaining periodontal health is key not only to oral health, but also to overall health. Periodontal diseases serve as bidirectional risk factors for numerous systemic inflammatory diseases that affect the cardiovascular, respiratory, endocrine, musculoskeletal, and reproductive systems.1–8 Patients’ negative habits, such as smoking and poor diet, hurt both oral and systemic health.
The predictability and long-term success of periodontal treatment is largely dependent on patient compliance.9 Studies show that patients’ commitment to periodontal maintenance recare schedules, as well as implementation of lifestyle changes may help prevent disease manifestation or recurrence.10–13
Behavior modification in patients with periodontal diseases is necessary to improve periodontal treatment success. However, the behaviors affecting periodontal disease progression are often the most difficult to change.14 Even when targeted behaviors are modified, it may take weeks or months to see the results of those changes.15 This lack of instant gratification may be discouraging for some patients. Clinicians may want to liken patients’ efforts to improve their oral health to running a marathon vs a sprint.
Improved oral hygiene in patients with gingivitis or periodontitis may initially be accompanied by pain and bleeding. These symptoms are transient, yet they may discourage uninformed patients. When giving oral hygiene instructions to patients with severely inflamed gingiva, they should be prepared for initial discomfort during self-care and urged to proceed with the prescribed protocol. The initial pain and bleeding experienced during mechanical plaque removal is normal and will likely subside when the plaque-induced inflammation diminishes, as long as the patient is compliant with the overall treatment plan.
Over time, patient compliance with self-care regimens may falter without consistent reinforcement by clinicians.9,11,16 The chronicity of periodontitis and its associated systemic health conditions may not be perceived as immediately dangerous by patients.17 As such, clinicians may want to further explore patient-specific beliefs, thoughts, and attitudes that may affect the adoption of improved self-care behaviors. Identifying interventions that produce the best long-term results is challenging.17
Uitenbroek et al18 assessed the influence of dental hygienists in the private practice setting regarding patient education, motivation, self-care, and patient’s perception of change. Study participants who visited a dental hygienist scored better on all scales. This difference remained even when the data were adjusted for social demographic variables and the dentist’s influence. Dental hygienists play key roles in patient education and behavior modification. And the stakes are high. Patients with existing periodontal diseases may increase their morbidity with poor self-care. According to the World Health Organization even “increasing the effectiveness of adherence interventions may have a far greater impact on the health of the population than any improvement in specific medical treatments.”19
Evidence-based interventions adapted from well-researched psychological models may help oral health professionals predict their patients’ oral health behaviors.20 Social cognition models help clinicians understand which factors determine patient compliance. Whether individuals will change their behavior is influenced by their attitudes and beliefs. These models are continuously researched and adapted to improve today’s increasingly complex and comprehensive patient care. An analysis of the most successful models for behavior modification and their practical implementation in the dental setting may help clinicians determine the most effective approaches to encourage positive treatment outcomes. Behavior can be changed through a number of psychological interventions. Dental professionals who have a deep understanding of the social cognitive theories commonly used in patient management are well prepared to help their patients achieve successful outcomes.21
HEALTH BELIEF MODEL
The Health Belief Model is a psychological model used to alter patient behavior through the explanation and prediction of health-related behaviors based on patients’ beliefs about what is healthy (Figure 1).22–24 For example, if the goal is to implement better oral hygiene, improving patient education is integral to the process. In other words, patients make better health decisions when they are better informed on healthy behaviors by clinicians.25
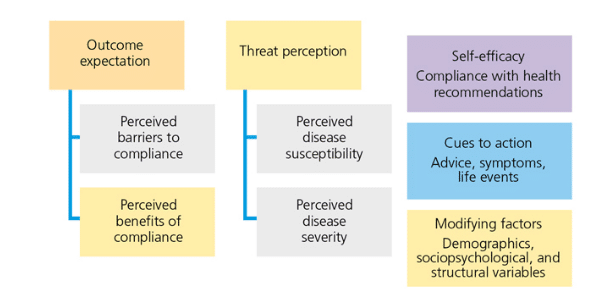
The Health Belief Model was developed by the United States Public Health Service to explain health-related behaviors and to predict health behavior change by focusing on individuals’ attitudes and beliefs. The goal of this model is to inspire patients to change their health behaviors and to predict engagement in health-supporting behaviors.23
A patient’s belief in the need and success of preventive treatment is directly related to compliance. Kühner and Raetzke26 found that patient understanding of disease susceptibility and perceived benefits gained through compliance helped improve oral hygiene behaviors.
The Health Belief Model is a staged approach, in which each step toward compliance is based on the previous belief. Patients must understand that they are susceptible to periodontitis, agree that periodontitis is dangerous to their overall health and well-being, realize their need to undergo treatment to arrest disease progression, and acknowledge that barriers can be eliminated when commitment is present. Each step builds on the previous concept. While patient education is important, however, understanding alone may not always lead to behavior modification.25
SOCIAL LEARNING THEORY
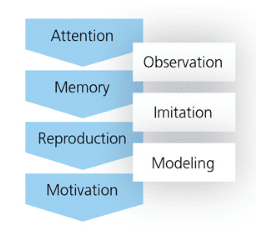
Social learning theories are based on individuals learning from each other through observation, imitation, and modeling. Interventions based on social learning include goal setting, behavior cues, and feedback on performance. Three studies conducted on social learning constructs showed that such interventions were effective in producing changes in patients’ periodontal status.20
Bandura’s Social Learning Theory (Figure 2) bridges behaviorism—or the idea that behavior can be explained in terms of conditioning as opposed to thoughts and/or feelings—and the Cognitive Learning Theory—the thought process that identifies thinking/mental processes and how they are impacted by internal and external factors in the context of human learning—because it includes attention, memory, and motivation.27
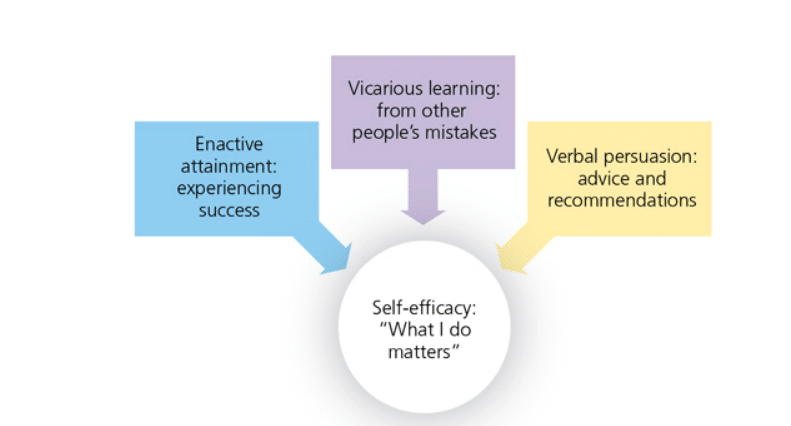
The construct of social cognitive theories includes self-efficacy, or the belief that the outcome is affected by one’s choices (Figure 3).14,27–29 The self-efficacy construct appears to be a reliable predictor of oral health behavior modification.30
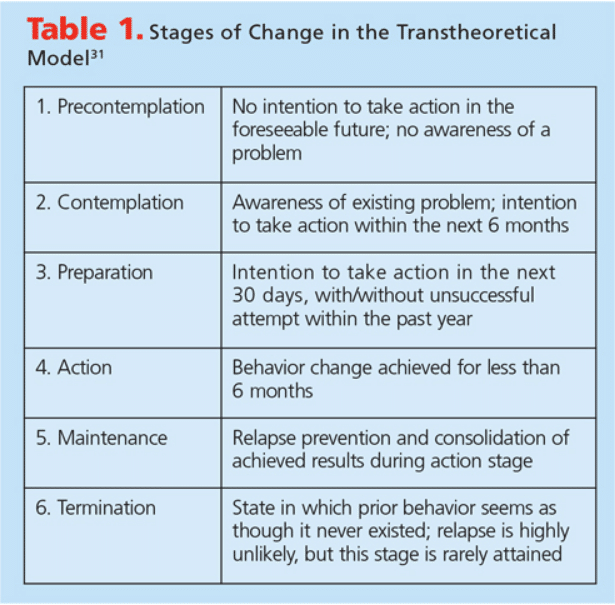
STAGES OF CHANGE MODEL
The Transtheoretical Model is a system of behavior modification that evaluates individuals’ readiness to change and provides strategies to help them achieve the desired change and/or end result. In this model, the behavior change is perceived as a long-term process, and not as an event. The Transtheoretical Model is based on the stages of change: precontemplation, contemplation, preparation, action, maintenance, and termination (Table 1).31
Using tobacco cessation as an example, in the stage of precontemplation, providing information may initiate the patient to consider change. At this point, the patient has no intention of changing his or her habits and may not be aware that the behavior is causing negative health consequences. While some longtime smokers will reject any attempt to quit tobacco use, research shows that even broaching the subject makes an impression and may lead the patient to enter the contemplation stage.
During the contemplation stage, the patient weighs the pros and cons of the behavior change, as well as the benefits and costs of making a change. Available resources are explored and community and public health programs may be engaged in assisting the patient in smoking cessation. If the available options seem beneficial and appropriate, the next stage of preparation is reached. A date to quit smoking may be set.
During the preparation stage, concrete plans are solidified to make the change happen and intended action is scheduled. During this phase, the patient may enroll in a smoking cessation program. As the patient moves through the stages, change becomes more realistic.
In the action stage, the patient has changed his or her behavior to the desired outcome and the change is implemented. In the maintenance stage of this model, the change has been continuous for the past 6 months. In the termination stage, the patient may become a facilitator for those who seek to change their behavior in a similar manner.
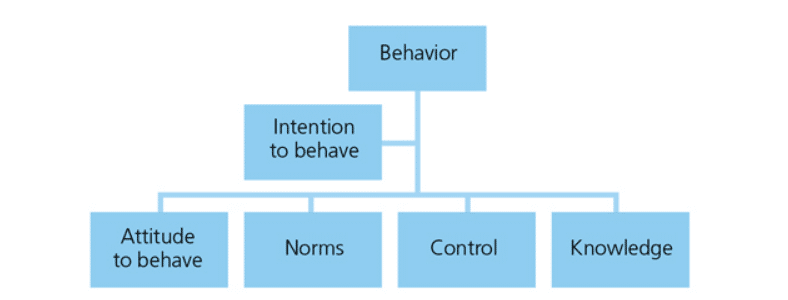
THEORY OF PLANNED BEHAVIOR
The Theory of Planned Behavior associates beliefs with behaviors (Figure 4). It acts as a mediator between the attitude and the action. After the available resources are filtered for information, intentions solidify. The intention to enact a behavior is the most reliable predictor of that behavior. However, attitudes toward how much control is perceived over the behavior and what the social norms are determine the intention. In other words, when good oral hygiene is highlighted in the media, it becomes more socially accepted. For instance, football fans who watched Carolina Panthers quarterback Cam Newton floss his teeth while sitting on the bench during the first televised game of the 2016/2017 season may be more inclined to adhere to an interdental cleaning regimen.
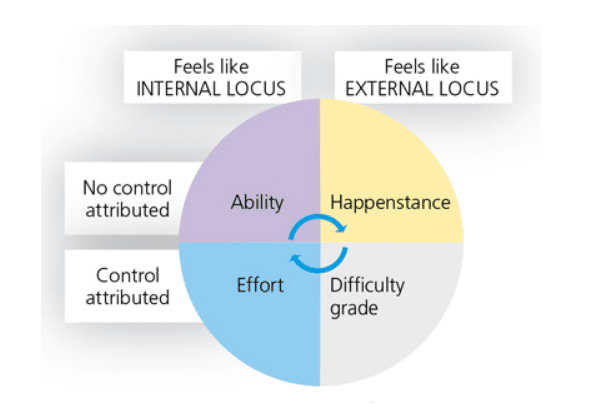
LOCUS OF CONTROL
In personality studies, the locus of control refers to the distribution of power (Figure 5). In this context, the power to determine results is by directly impacting happenings. When patients’ loci of control are internal, they believe they are in charge of their own fate and take responsibility for the outcome of what happens to them. When the loci of control are external, patients tend to blame outside sources for their failures and successes.32–34 If patients believe they can control their oral health and that they have the tools and capability to eliminate the etiology of their disease, the focus becomes internal. Patients need to understand the benefits of daily oral hygiene so they are empowered to be in charge of their own oral health.
IMPLEMENTATION INTENTIONS
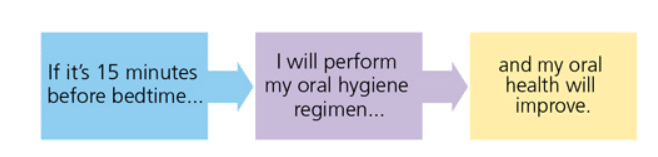
For most social cognition models, motivation is the most immediate behavior predictor; however, it is not the only factor in behavior change. There is a distinction between the intentions aimed toward a goal itself and the intentions toward implementing the goal.
The implementation intentions are the concrete steps necessary to achieve a desired objective. Within the implementation plan, the more automatic the steps become, the more likely the goal will be achieved. A schedule provides the dates, times, and location of steps and introduces regularity into a behavior. Stern et al33 conducted groundbreaking studies on this model, finding that even anxiety-relieving properties in the implementation intentions eliminate critical goal pursuit obstacles. Figure 6 provides an example of an implementation intention for patients who want to obtain or maintain periodontal health.33
PRACTICAL APPLICATION
No one psychological model has been successful in predictably achieving clinically significant behavior modifications in patients.34 Clinicians may experience the best results if they incorporate a variety of interventions, creating an individualized patient education approach.
After reviewing the available psychological interventions, four main interventions can be classified in a conceptual framework:35
- Intervention content: particular brushing technique, interproximal oral hygiene
- Construct/vehicle: education about health benefits to achieve belief change, recommending a power toothbrush
- Education modality: one-on-one interaction, video, pamphlet, patient self-education
- Outcome assessment: patient self-evaluation, plaque index, bleeding on probing
The goal of intervention is to achieve a long-term change in the patient’s behavior, as current behavior supports disease. The intervention may be direct or indirect, primary or secondary, and may incorporate several components, such as education, demonstration, follow-up, and maintenance support. Techniques used to deliver each component may vary. Depending on the intervention, the delivery may require devices or tools. Each patient is an individual, and so is his or her disease. The intervention should be tailored to the phenotype of the condition treated.
Using the learning theories provided by educational psychology may help improve behavior modification and patient education. However, some critics do not believe such theories are necessary.36 Clinicians must use their own judgment when deciding on appropriate strategies for improving behavior modification in their patients. Developing a custom-fit approach to individual patient needs is always the most effective.
To help patients clearly understand the benefits of improving oral hygiene-related behaviors, patients must understand the seriousness of their periodontal disease, as well as the negative oral and overall health consequences.37
The professions of dentistry and dental hygiene are goal oriented and based on efficient problem solving. Whether the use of psychological interventions works in achieving behavior modifications remains unclear, as no conclusive data univocally support one approach. Clinicians are best served by learning about the most utilized theories and implementing the aspects most relevant to their patient’s situation.
ACKNOWLEDGEMENTS
The author would like to thank Christopher Aloise and Rachel Rabins for their assistance with this manuscript
REFERENCES
- Pizzo G, Guiglia R, Lo Russo L, Campisi G. Dentistry and internal medicine: from the focal infection theory to the periodontal medicine concept. Eur J Intern Med. 2010;21:496–502.
- Williams RC, Barnett AH, Claffey N, et al. The potential impact of periodontal disease on general health: a consensus view. Curr Med Res Opin. 2008;24:1635–1643.
- Anil S, Al-Ghamdi HS. The impact of periodontal infections on systemic diseases. An update for medical practitioners. Saudi Med J. 2006;27:767–776.
- Kinane DF, Marshall GJ. Periodontal manifestations of systemic disease. Aust Dent J. 2001;46:2–12.
- Schenkein HA, Loos BG. Inflammatory mechanisms linking periodontal diseases to cardiovascular diseases. J Clin Periodontol. 2013;40(Suppl 14):S51–S69.
- Watt RG, Petersen PE. Periodontal health through public health—the case for oral health promotion. Periodontol 2000. 2012;60:147–155.
- Cetin I, Pileri P, Villa A, Calabrese S, Ottolenghi L, Abati S. Pathogenic mechanisms linking periodontal diseases with adverse pregnancy outcomes. Reprod Sci. 2012;19:633–641.
- Sadighi M, Shamami M, Shamami S, Amini S. Periodontal disease and tooth loss as risks for cancer: a systematic review of the literature. Iran J Cancer Prev. 2011;4:189–198.
- Merin RL. Supportive periodontal treatment. In: Newman M, Takei H, Klokkevold P, Carranza F, eds. Carranza’s Clinical Periodontology. 12th ed. 2012:746-755.
- Van der Weijden F, Slot DE. Oral hygiene in the prevention of periodontal diseases: the evidence. Periodontol 2000. 2011;55:104–123.
- Wilson TG Jr. How patient compliance to suggested oral hygiene and maintenance affect periodontal therapy. Dent Clin North Am. 1998;42:389–403.
- Hancock EB, Newell DH. The role of periodontal maintenance in dental practice. J Indiana Dent Assoc. 2002;81:25–30.
- Gokulanathan S, Balan N, Aravind RJ, Thangavelu K. Patient compliance and supportive periodontal therapy: Study among young adults of Namakkal district. J Pharm Bioallied Sci. 2014;6: S171–S173.
- Renz AN, Newton JT. Changing the behavior of patients with periodontitis. Periodontol 2000. 2009;51:252–268.
- Renz A, Ide M, Newton T, Robinson PG, Smith D. Psychological interventions to improve adherence to oral hygiene instructions in adults with periodontal diseases. Cochrane Database Syst Rev. 2007:2:1–17.
- Wilson TG. Compliance and its role in periodontal therapy. Periodontol 2000. 1996:12:16–23.
- Ciancio S. Improving oral health: current considerations. J Clin Periodontol. 2003;30(Suppl 5):4-6.
- Uitenbroek DG, Schaub RM, Tromp JA, Kant JH. Dental hygienists’ influence on patients’ knowledge, motivation, self-care, and perception of change. Community Dent Oral Epidemiol. 1989;17:87–90.
- World Health Organization. Adherence to Long-Term Therapies—Evidence for Action. Available at: apps.who.int/medicinedocs/en/d/Js4883e/5.html. Accessed September 8, 2016.
- Abraham C, Kelly MP, West R, Michie S. The UK national institute for health and clinical excellence public health guidance on behaviour change: a brief introduction. Psychol Health Med. 2009;14:1–8.
- Huffman JC, DuBois CM, Millstein RA, Celano CM, Wexler D. Positive psychological interventions for patients with type 2 diabetes: rationale, theoretical model, and Intervention Development. J Diabetes Res. 2015;2015:428349.
- Rosenstock I. The health belief model and preventive health behavior. Health Education Monographs. 1974;2:354–386.
- Luszczynska A, Schwarzer R. Social cognitive theory. In: Conner M, Norman P, eds. Predicting Health Behaviour. Maidenhead, UK: Open University Press; 2005:127–169.
- Straker D. Health Belief Model. Available at: changingminds.org/explanations/belief/health_belief_model.htm. Accessed September 8, 2016.
- Barker T. Role of health beliefs in patient compliance with preventive dental advice. Community Dent Oral Epidemiol. 1994;22:327–336.
- Kühner MK, Raetzke PB. The effects of health beliefs on the compliance of periodontal patients with oral hygiene instructions. J Periodontol. 1989;60:51–56.
- Hollister MC, Anema MG. Health behavior models and oral health: a review. J Dent Hyg. 2004;78:6.
- Bandura A. Social cognitive theory: An angentic perspective. Annu Rev Psychol. 2001;52:1–26.
- Bandura A. Self-Efficacy: the Exercise of Control. New York: Freeman; 1997.
- Little SJ, Hollis JF, Stevens VJ, Mount K, Mullooly JP, Johnson BD. Effective group behavioral intervention for older periodontal patients. J Periodontal Res. 1997:32:315–325.
- Prochaska JO, Redding CA, Evers KE. Health Behavior and Education. San Francisco: Jossey Bass; 1997.
- Prochaska JO, DiClemente CC, Norcross JC. In search of how people change. Am Psychol. 1992:47:1102–1114.
- Stern C, Cole S, Gollwitzer PM, Oettingen G, Balcetis E. Effects of implementation intentions on anxiety, perceived proximity, and motor performance. Pers Soc Psychol Bull. 2013;39:623–635.
- Werner H, Hakeberg M, Dahlström L, et al. Psychological Interventions for poor oral health: a systematic review. J Dent Res. 2016;95:506–514.
- Hodges L, Walker J, Kleiboer A, et al. What is a psychological intervention? A meta-review and practical proposal. Psycho-Oncology. 2011;20:470–478.
- Greenberg D. A New Look at Learning, The Sudbury Valley School Experience. Framingham, Massachusetts: Sudbury Valley School; 1987.
- Newton T, Asimakopoulou K. Managing oral hygiene as a risk factor for periodontal disease: a systematic review of psychological approaches to behaviour change for improved plaque control in periodontal management. J Clin Periodontol. 2015;42:36–46.
From Dimensions of Dental Hygiene. October 2016;14(10):45—50.