
Medical Emergencies in the Dental Setting
Knowledge of medical emergency etiology and strategies for their efficient handling is key to supporting successful outcomes.
This course was published in the April 2023 issue and expires April 2026. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
AGD Subject Code: 142
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- List the most common medical emergencies that occur in dental settings.
- Discuss the importance of medical emergency prevention training and protocols.
- Explain how simulation training is essential for proper medical emergency management training.
While fairly rare, medical emergencies do occur in dental settings, and oral health professionals need to be prepared. Cardiac events, syncope (fainting), diabetic complications, and allergic reactions are possible emergencies that dental professionals may encounter.
Medical emergencies may occur due to reaction to medications, anxiety, local anesthesia complications, or pre-existing conditions.1 Tooth extractions and pulp expirations are the most common dental procedures that precede emergencies.2 Approximately 37% of medical emergencies occur during dental treatment, 23% happen prior to treatment being rendered, and 20% follow local anesthesia administration.2
Preparedness Is Crucial
More than half of oral health professionals will need to manage some form of a medical emergency during their professional careers.3 The most common medical emergency in the dental office is syncope (more than 50%), followed by mild allergic reaction (8%), angina pectoris (8%), postural hypotension (8%), and seizures (5%).1,3–7 Approximately 75% of dental professionals will witness or manage syncope in their careers.8
Some of the least common medical emergencies reported in dental offices are diabetic complications, foreign body aspiration, and anaphylactic shock.4–6 Frequently, overlap occurs between the most and least common medical emergencies. For example, diabetic complications may be the most common in one dental office but the least common at a nearby office. The patient populations served and the most frequently performed procedures impact the type of medical emergencies most likely to occur in individual dental offices. Due to these variations, dental professionals should be prepared to manage any type of emergency.
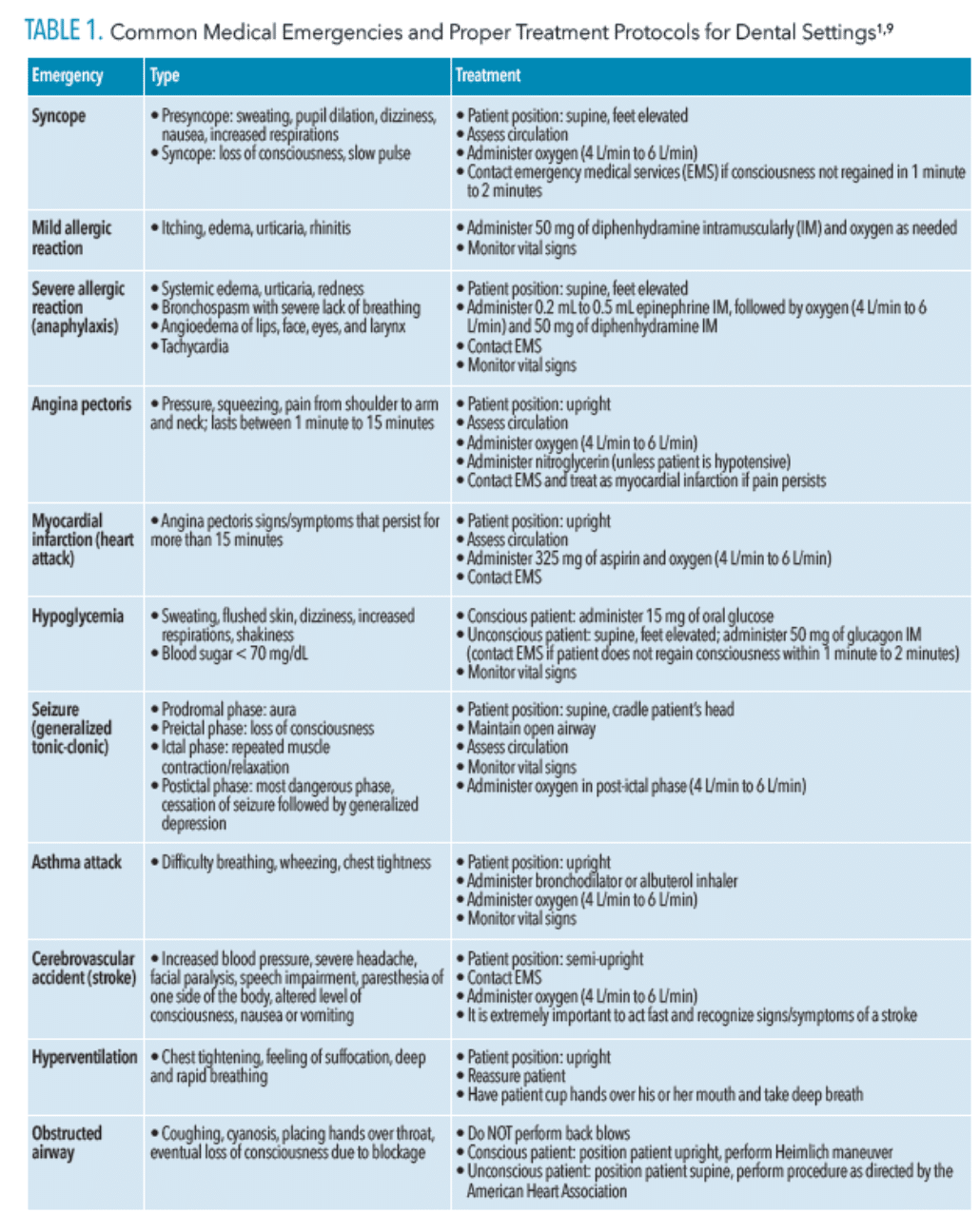
Oral health professionals need to be knowledgeable about the different medical emergencies that may occur based on their office’s specific patient populations. Table 1 reviews medical emergencies that occur in dental settings and their treatment protocols.1,9
Status of Management Skills
Knowledge and preparedness for medical emergency management in the dental office are crucial to carrying out proper protocols for each event. Vaughan et al3 report that oral health professionals’ confidence in medical emergency management is directly related to the amount of training they have received.
In another study, de Bedout et al8 found that dental providers who graduated more recently had a 75% confidence rate for managing medical emergencies compared to those with more distant graduation dates, who had a 50% confidence rate. Approximately 65% of general dentists do not feel comfortable managing medical emergencies—including cardiac arrest, seizures, and anaphylactic shock—in pediatric patients.10
Gazal et al11 conclude a moderate level of knowledge of medical emergency management exists among dental professionals. Survey results revealed that 46% could not manage cardiac arrest adequately and approximately 98% of participants showed a need for further training in medical emergency management.
In a study of Polish dentists, participants reported feeling competent in managing cardiac arrest (42%), hypertensive crisis (75%), asthma (55%), anaphylactic shock (55%), and seizures (53%).12 However, a study of dental hygienists found that many participants lacked knowledge about cardiac arrest, with 15% of participants unable to recognize an absence of breathing and 80% unable to note abnormal breathing.5
Prevention is critical to the proper management of medical emergencies in the dental office. In a study of four dental schools where the patient’s medical history was thoroughly evaluated before treatment, clinicians were able to identify predisposing factors for medical emergencies.6 Ali et al13 suggest the best way to manage orthostatic hypotension is to review medical history.
A Belgian study that assessed dental professionals’ awareness and knowledge regarding medical emergency management found that 19% of providers did not review medical history prior to appointments.4 However, in a study that focused on the etiology and management of syncope, Hutse et al7 discovered that medical history review is ineffective at preventing syncope because the risk is linked to psychogenic factors. However, they also note that only 14% of dental professionals knew how to manage syncope properly. A patient’s history of syncope should always be noted in the medical history; this information will help clinicians differentiate between episodes of syncope and other conditions, such as epileptic seizures.7
A clear need exists for further training on medical emergency management among dental providers.3,8,12,14 In a survey of oral health professionals about basic life support (BLS) and medical emergency training, 94% reported that formal BLS training is essential and should be required and 100% agree that simulation training is useful for learning how to manage medical emergency procedures.3
Studies show that students and professionals have positive experiences with simulation training.15,16 Dental and dental hygiene students in the United States are required to achieve competence in medical emergency and BLS training to graduate, according to the Commission on Dental Accreditation.17 BLS training is also required for dental licensures in the US; however, there is no requirement for medical emergency training.
Importance of Medical Emergency Training
In many countries, medical emergency training is not part of dental or dental hygiene license requirements.3,18 In the US, BLS courses must be completed to gain licensure.
Dental professionals often only receive medical emergency training in schools. Only 23% of American dentists report having participated in a medical emergency training session after graduation, while 68% said they had participated in at least one medical emergency training session prior to graduation.14
A survey by Stafuzza et al18 found that only 57% of dentists felt comfortable performing first aid and BLS, 28% knew how to manage medical emergency equipment properly, and 67% were prepared for cardiopulmonary resuscitation. Gazal et al11 also found that 90% of the participants showed the need for further training. Due to this lack of confidence, oral health professionals should engage in annual medical emergency training, either through in-person or continuing education activities.
Simulation training for BLS and medical emergency management is crucial for dental professionals because it increases knowledge and accuracy of medical emergency management.3 Those trained with simulation training scored significantly higher on post-assessments than those without simulation training.
High-fidelity simulation is essential to helping dental hygiene students feel prepared to manage medical emergencies.19 This type of training uses lifelike, realistic patient encounters where manikins are used to simulate emergency scenarios such as cardiac distress, breathing problems, and seizures. With simulation training, 95% of dental hygienists correctly managed their given emergency scenarios.15
In one study, students were asked to locate emergency equipment.20 Only 10% of the students who had not received simulation could locate seven of the nine emergency items. Of the students who received simulation training, 100% could locate seven of the nine emergency items.
Studies show that simulation training is the gold standard for competence among dental professionals in managing medical emergencies.16,20,21 Simulation training increases practitioner confidence and students rate simulation training more favorably than didactic training alone.16,21
Experience with simulation training is directly proportional to a dental professional’s confidence in managing medical emergencies.3 Oral health professionals should engage in simulation training annually or once every 2 years to keep current on medical emergency protocols, which continue to evolve. For example, recent evidence shows that ammonia inhalants should not be used to treat vasovagal syncope in the dental setting because they can irritate the respiratory tract and lungs.22
Dental offices should review their medical emergency protocols annually. Offices that do are more likely to experience better outcomes with medical emergency management than those that don’t.23
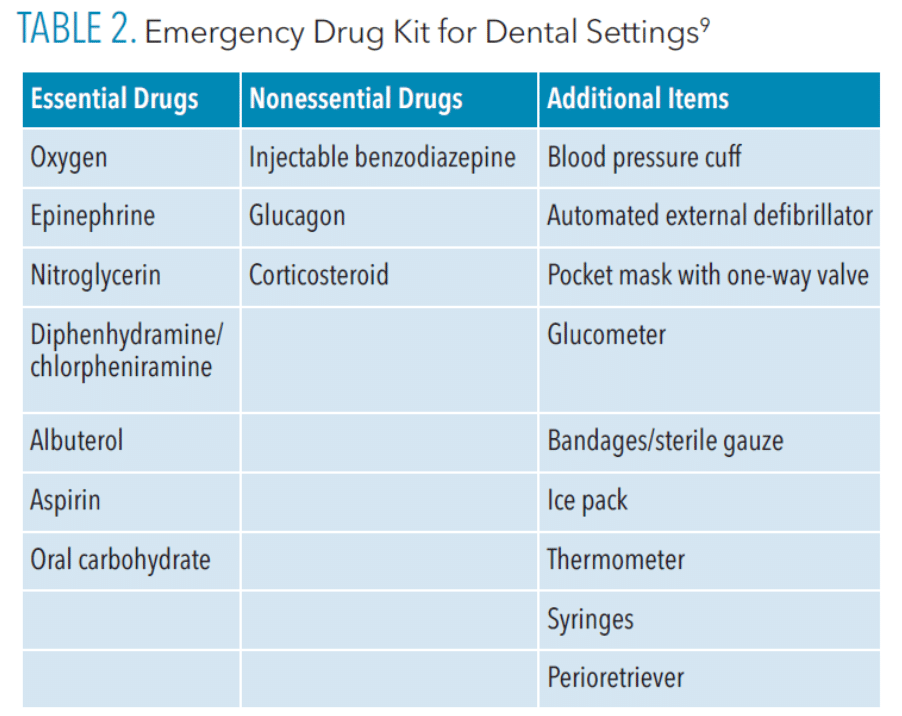
Emergency drug kits should be accessible to all dental team members and consistently restocked to ensure medications are not expired and that equipment is working properly.9
Table 2 lists the Items that should be included in an emergency drug kit. Reviewing medical history and medications before patient appointments, taking vital signs, and maintaining competence in medical emergencies are key components of proper management of medical emergencies in the dental setting.
![]() Conclusion
Conclusion
Oral health professionals need to be prepared to handle medical emergencies in the dental setting and it appears that there is need for ongoing training in this area. Additional research is need on the medical emergency requirements for dental professionals by state and dental hygienists’ knowledge and preparedness for medical emergency management.
In summary, simulation training should be implemented routinely so oral health professionals are confident to manage a wide array of medical emergencies. Oral health professionals must remain current on medical emergency protocols and recognize that prevention is the best way to prepare for medical emergencies in the dental setting.
References
- Sadi HK, Rosenberg M. Managing medical emergencies. Dimensions of Dentaly Hygiene. 2015;13(1):52–55.
- Malamed, Stanley F. Medical Emergencies in the Dental Office. 8th ed. Philadelphia: Elsevier Mosby; 2022.
- Vaughan M, Park A, Sholapurkar A, Esterman A. Medical emergencies in dental practice – management requirements and international practitioner proficiency. A scoping review. Aust Dent J. 2018;63:455–466.
- Marks LAM, Van Parys C, Coppens M, Herregods L. Awareness of dental practitioners to cope with a medical emergency: a survey in Belgium. Int Dent J. 2013;63:312–316.
- Smereka J, Aluchna M, Aluchna A, et al. Medical emergencies in dental hygienists’ practice. Medicine (Baltimore). 2019;98:e16613.
- Sorenson AD, Marusko RM, Kennedy KS. Medical emergencies in the dental school setting. J Dent Educ. 2021;85:1223–1227.
- Hutse I, Coppens M, Herbelet S, Seyssens L, Marks L. Syncope in dental practices: a systematic review on aetiology and management. J Evid-Based Dent Pract. 2021;21:101581.
- de Bedout T, Kramer K, Blanchard S, et al. Assessing the medical emergency preparedness of dental faculty, residents, and practicing periodontists: an exploratory study. J Dent Educ. 2018;82:492–500.
- Grimes, Ellen B. Medical Emergencies: Essentials for the Dental Professional. 2nd ed. New York: Pearson; 2013.
- Čuković-Bagić I, Hrvatin S, Jeličić J, et al. General dentists’ awareness of how to cope with medical emergencies in paediatric dental patients. Int Dent J. 2017;67:238–243.
- Gazal G, Aljohani H, Al-Samadani KH, Nassani MZ. Measuring the level of medical-emergency-related knowledge among senior dental students and clinical trainers. Int J Environ Res Public Health. 2021;18:6889.
- Smereka J, Aluchna M, Aluchna A, Szarpak Ł. Preparedness and attitudes towards medical emergencies in the dental office among Polish dentists. Int Dent J. 2019;69:321–328.
- Ali A, Ali NS, Waqas N, et al. Management of orthostatic hypotension: a literature review. Cureus. 2018;10:e3166.
- Solanki C, Geisinger ML, Luepke PG, et al. Assessing readiness to manage medical emergencies among dental students at four dental schools. J Dent Educ. 2021;85:1462–1470.
- Bilich LA, Jackson SC, Bray BS, Willson MN. High-fidelity simulation: preparing dental hygiene students for managing medical emergencies. J Dent Educ. 2015;79:1074–1081.
- McKenzie CT, Tilashalski K, Abou-Arraj R, Peterson DT, White ML. Students’ evaluations of simulations in dentistry: a multiple cohort study at a U.S. dental school. J Dent Educ. 2019;83:1142–1150.
- Commission on Dental Accreditation. Accreditation Standards for Dental Hygiene Education Programs. Chicago: American Dental Association; 2022:45.
- Stafuzza TC, Carrara CFC, Oliveira FV, Santos CF, Oliveira TM. Evaluation of the dentists’ knowledge on medical urgency and emergency. Braz Oral Res. 2014;28:S1806-83242014000100240.
- Kanjirath P, Williams L, Ramos M. High-fidelity simulation training for management of dental emergencies. Gen Dent. 2018;66:14–15.
- Pinsky HM, Le JM, Sweier DG, Marti K. Dental students’ ability to locate emergency equipment-lessons learned from aviation. Eur J Dent Educ Off J Assoc Dent Educ Eur. 2018;22:e19–e25.
- Manton JW, Kennedy KS, Lipps JA, Pfeil SA, Cornelius BW. Medical emergency management in the dental office (MEMDO): a pilot study assessing a simulation-based training curriculum for dentists. Anesth Prog. 2021;68:76–84.
- Goodchild JH, Donaldson M. Is it time to omit ammonia inhalants from dental emergency kits? Gen Dent. 2022;70:6–9.
- McGuinness MA. Preparing for medical emergencies. Dimensions of Dental Hygiene. 2019;17(4):30–33.
From Dimensions of Dental Hygiene. April 2023; 21(4):28-31.


 Conclusion
Conclusion
