Managing Sjögren Syndrome
Dental professionals play a vital role in identifying, managing, and improving the quality of life for patients with this autoimmune disorder.
This course was published in the January/February 2025 issue and expires February 2028. The author has no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
AGD Subject Code: 149
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Discuss the diagnostic process for Sjögren syndrome (SS).
- Identify the role of the dental professional in the management of patients with SS.
- List the available treatment strategies for SS and their side effects.
Sjögren syndrome (SS) is a prevalent chronic inflammatory autoimmune disorder primarily affecting women ages 40 to 60.1-8 It affects approximately 0.5% to 1% of the United States population, equating to about 3.1 million individuals.1,2-5,9 The likelihood of diagnosis increases with age.10
SS has two classifications: primary and secondary. This article will discuss primary SS, which results from lymphocytic infiltration of the oral salivary and lacrimal glands. Secondary SS occurs in the presence of other systemic conditions and among geriatric populations and patients undergoing head and neck radiation therapy.5,6,9,13
The production and consistency of saliva are crucial for maintaining good oral health. Patients with SS experience hypofunction or dysfunction of the salivary glands, leading to dry mouth (Figure 1) and are at increased risk for decay, candidiasis, periodontal diseases, burning mouth, and complications in speech and swallowing.4,5,6,11,13

Saliva is a complex and necessary oral fluid secreted by the major and minor salivary glands; it contains enzymes for digestion, aids in the remineralization of enamel, and helps protect against tissue destruction by periodontal pathogens.14 Serous and mucous are the two forms of saliva. Serous saliva is a watery, amylase-enriched substance containing antibacterial, antifungal, antiviral agents, and enzymes and the ability to buffer pH to regulate saliva. In contrast, mucous saliva is thicker in composition and forms a protective layer over the teeth and oral mucosa.7,15
The typical unstimulated salivary flow for an individual without SS is 0.3 to 0.4 ml per minute, with a pH of 6 to 7.14,15 Patients with SS who present with hyposalivation have a salivary flow of less than 0.1 ml per minute.14,15 Insufficient saliva production increases biofilm accumulation and reduces the protective dental pellicle, making teeth more susceptible to demineralization by acidogenic bacteria.7,13-15
Xerostomia is one of the most common manifestations in patients with SS . Although 47% of the population will experience dry mouth symptoms at some point, only 10% are diagnosed with SS.9 Key indicators include lack of saliva pooling in the floor of the mouth and the buccal labial mucosa sticking to the examination mirror and teeth.1,3,4 The symptoms and severity of dry mouth in patients with SS extend beyond the patient’s reports of oral dryness or the clinical assessment when examining for salivary flow.9 Diagnosis of SS requires specific salivary and parotid gland testing, which is typically recommended after a patient presents with ocular or oral dryness for more than 3 months. Additional clinical findings that may suggest the need for further testing include swollen parotid glands, extreme fatigue, peripheral neuropathy, abnormal serologic tests, or an unknown reason for increased caries activity.4
The Saxon test, a stimulated salivary flow test, measures saliva production. Patients are given a weighted sponge to chew on for 2 minutes without swallowing while it collects pooled saliva. The sponge is then weighed to measure the amount of saliva produced. Less than 2.75 grams is considered an indicator of SS and requires additional testing to confirm a diagnosis.4 Further testing recommendations include, diagnostic images, blood samples to evaluate for serologic positive anti-RO/SSA and anti-LA/SSB antibodies, and a labial salivary gland biopsy if antibodies yield a weak positive result.2,4
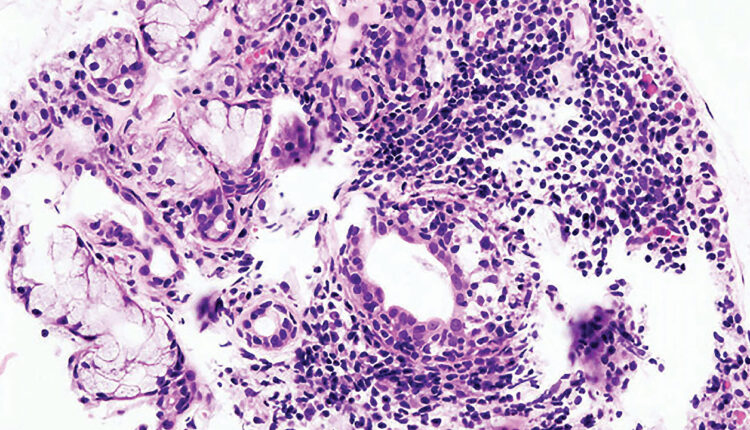
Biopsy of the labial salivary gland identifies SS by evaluating the degree of lymphoid infiltration, which is determined by measuring tightly aggregated lymphocytes, known as the focus score. Fifty or more tightly aggregated lymphocytes, which is equivalent to one focus score, is indicative of higher lymphoid infiltration and is observed in 66% to 89% of patients with SS.4 The focus score is also used as a prognostic marker, as the higher the score, the greater risk for lymphoma in this patient population.4
 Ultrasounds, computed tomography (CT), and magnetic resonance imaging are used to identify parenchymal abnormalities (distortions, narrowing, or dilation of the ducts), hypoechoic areas with convex borders (masses) and abnormal fat build-up and glandular cysts commonly observed in individuals with SS. CT scans can also note possible diffuse punctate calcifications (sphere-shaped, round, radiopaque calcifications that are small and vary in size), which are specific to SS.4
Ultrasounds, computed tomography (CT), and magnetic resonance imaging are used to identify parenchymal abnormalities (distortions, narrowing, or dilation of the ducts), hypoechoic areas with convex borders (masses) and abnormal fat build-up and glandular cysts commonly observed in individuals with SS. CT scans can also note possible diffuse punctate calcifications (sphere-shaped, round, radiopaque calcifications that are small and vary in size), which are specific to SS.4
The Schirmer test is conducted by an ophthalmologist to examine tear production; less than 5 mm of tear production occurring within 5 minutes is indicative of SS.2,8,10 With SS, salivary and lacrimal glands are often destroyed. Dysfunctional exocrine glands, lymphocytic infiltration, and B-cell hyperactivity further impair these glands, leading to decreased secretion flow.4,10 The reduced tear production from the lacrimal glands can cause significant discomfort.
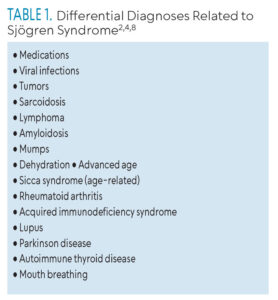
These examinations are used not only to diagnose SS but to distinguish it from differential diagnoses such as age-related sicca syndrome, which also produces a decline in saliva and tear production (Table 1). Additionally, several medications are known to cause dry mouth, particularly antihypertensives, antidepressants, antihistamines, and diuretics.4,9
Role of the Dental Professional
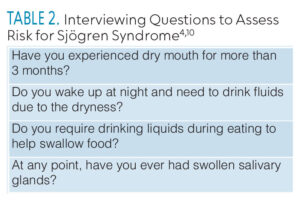
Dental professionals are uniquely positioned to improve the quality of life for patients with SS by recognizing, educating, and helping to manage symptoms and prevent dental caries and periodontal diseases.2,7 Conducting a thorough medical history and using a chairside guide to ask guided questions is essential to managing patients’ care and providing appropriate referrals (Table 2).
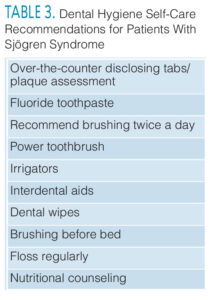
Specific evidence-based self-care recommendations should be implemented to manage oral dryness, difficulty swallowing, and swelling of the salivary glands (Table 3).2 Patients also need the following: recare visits every 3 to 6 months for dental prophylaxis, annual bitewing images to check for carious lesions, and oral hygiene instructions re-assessed at each visit.7,16 Patients with SS benefit from a routine caries risk assessment and product recommendations to alleviate symptoms, increase saliva production, and prevent decay.
Although performing an intraoral and extraoral exam is the standard of care, 15% to 25% of patients report not having a thorough exam during routine dental visits.17 Approximately half of all patients with SS will experience swelling of the parotid and/or submandibular glands.2,4 Conducting a proper evaluation of the salivary glands and saliva production requires a technique-sensitive examination. During an intraoral exam, the clinician stands behind or to the side of the patient. The clinician should place both palms of the hands with fingers extended on the entire cheek bilaterally using a circular motion and gently pressing against below the zygomatic bone. If there are any observed signs of parotid gland enlargement (Figure 2 and 3) or if the patient reports tenderness or pain, further investigation is recommended, and a referral should be provided.18

Methods of Improving Salivary Flow and Discomfort
Patients with SS often produce thick (mucous) or absent saliva. Increasing saliva flow helps with oral tissue movement and patient comfort.3,11 Mixing a small amount of oil (monitor the acidity) with water or artificial saliva can help moisturize and coat oral tissues. Dissolving cevimeline powder in water stimulates saliva production.3 Salivary substitute products and over-the-counter moisturizing solutions contain antibacterial enzymes that can alleviate the uncomfortable feeling of a dry mouth.5,6,9,13,14 Other alternatives are products containing xylitol, sugar-free hard candies, sugar-free gum, small sips of water, or “gleeking” to self-express saliva during times of need.3,6,11,14 Avoiding caffeine and limiting antihistamines are recommended.10,11
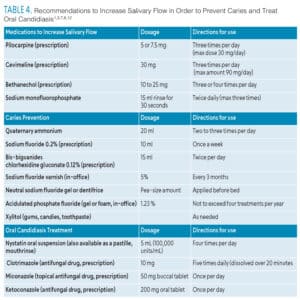
A recent study of 100 participants ranging in age from 22 to 79 found that mouthrinses with cetylpyridinium chloride (CPC) were more effective in minimizing discomfort and moisturizing the oral cavity for a longer duration period above other over-the-counter mouthrinses and water sipping (Table 4 provides options to treat and alleviate symptoms and effects of SS).6
Treatment and Prevention of Caries
SS significantly increases the risk of dental caries due to reduced protective salivary production, which causes biofilm to remain on the teeth, creating an acidic environment in the oral cavity.3,7,13,14 Caries Management by Risk Assessment, or CAMBRA, is an assessment tool that can assist clinicians with determining a patient’s caries risk and provide recommendations for management.2
Dietary sugars must be reduced or eliminated, fluoride toothpaste should be used, and those at high risk should also implement products that deliver calcium and phosphate to teeth, which enhance fluoride applications and aid in remineralization.3,4,13 Gold standard products include sodium fluoride 0.5% neutral rinses, casein phosphopeptides, amorphous calcium phosphate, professionally applied or patient-applied paste or gel, chlorhexidine rinses, and fluoride varnish application every 3 months.3,13
Rinses containing chlorhexidine, pilocarpine, and stannous fluoride are often recommended for patients with SS who are experiencing decreased saliva (Table 4). Chlorhexidine oral rinse has been shown to decrease Streptococcus mutans and other cariogenic bacteria.3,13
Pilocarpine rinse can aid in increasing salivary flow, maintaining a balanced or neutral pH, preventing caries, and reducing oral lesions in cases of moderate glandular dysfunction, where stimulated whole salivary flow ranges from 0.1 to 0.7 ml per minute.3,5,8,9,13,12 Pilocarpine does have side effects, including sweating, nausea, vomiting, diarrhea, rhinitis, headache, chest pain, abdominal cramps, dizziness, palpitations, increased urinary frequency, and increased tear production.8,12 Patients should consult their physician before using it.
Products containing high levels of fluoride should be recommended for daily use in those with dry mouth.13 Stannous fluoride rinses of 0.63% have about 1,512 ppm of fluoride and, when mixed with 5% xylitol, can help prevent caries.13
Treatment of Oral Candidiasis
Normal salivary flow acts as an antibacterial, antifungal, and antiviral agent.7 Patients with SS experience a higher occurrence of oral lesions due to decreased salivary flow in the oral cavity compared to those without SS.1,3 Treatments for oral candidiasis include antifungal rinses or lozenges,and denture-soaking agents such as diluted sodium hypochlorite or chlorhexidine (Table 4).1,3
Oral candidiasis is more likely to occur when salivary flow decreases. The most common oral lesions are angular cheilitis, along with atrophic glossitis, tongue fissures, and recurrent ulcerations.1,3,5 In primary or secondary SS, an inverse relationship exists between salivary flow and candidiasis; as saliva decreases, the risk for these lesions increases.1 Edentulous or partially edentulous patients with SS who wear removable dentures may be at risk of developing angular cheilitis, a burning sensation of the oral tissues, and fungal lesions more often.3
![]() Conclusion
Conclusion
The effective management of SS requires a comprehensive evaluation by oral health professionals with a proficient understanding of the syndrome’s symptomatology, progression, and management to minimize the impact on oral and overall health and quality of life. Providing routine dental care every 3 months, performing intra- and extraoral exams, and evaluating the saliva function and salivary glands are key to managing SS. Dental and medical professionals must collaborate to monitor and evaluate treatment responses. Further research on SS is needed to better understand oral health complexities, allowing dental hygienists to provide individualized care and recommend the best self-care regimens to manage the condition.
References
- Serrano J, López‐Pintor RM, González‐Serrano J, Fernández‐Castro M, Casañas E, Hernández G. Oral lesions in Sjögren’s syndrome: A systematic review. Med Oral Patol Oral Cir Bucal. 2018;23:e391-e400.
- Carsons SE. Sjögren Syndrome. Treasure Island, Florida: StatPearls; July 31, 2023.
- Wu AJ. Management of salivary hypofunction in Sjögren’s Syndrome. Current Treatment Options in Rheumatology. 2015;1(3):255-268.
- Baer AN. Diagnosis and classification of Sjögren syndrome. Available at uptod/te.com/contents/diagnosis-and-classification-of-sjogrens-disease. Accessed December 5, 2024.
- Nakagawa Y. Management of dry mouth in Sjögren’s syndrome. Japanese Dental Science Review. 2011;47(2):115-123.
- Jose A, Singh M, Magnuson B, Farag AM, Varghese R, Papas A. A randomized controlled study to evaluate an experimental moisturizing mouthwash formulation in participants experiencing dry mouth symptoms. Oral Surg Oral Med Oral Pathol Oral Radiol. 2018;126:231-239.
- Bolstad AI, Skarstein K. Epidemiology of Sjögren’s syndrome — from an oral perspective. Curr Oral Health Rep. 2016;3:328-336.
- Choudhry HS, Hosseini S, Choudhry HS, Fatahzadeh M, Khianey R, Dastjerdi MH. Updates in diagnostics, treatments, and correlations between oral and ocular manifestations of Sjogren’s syndrome. Ocul Surf. 2022;26:75-87.
- Swick AD, Kimple RJ. Wetting the whistle: neurotropic factor improves salivJ y function. J Clin Investig. 2014;124:3282-3284.
- Mavragani CP, Moutsopoulos HM. Sjögren syndrome. CMAJ. 2014;186:E579-E586.
- Lung CB, Watson GE, Verma S, Feng C, Saunders RH. Duration of effect of Biotène spray in patients with symptomatic dry mouth: a pilot study. Oral Surg Oral Med Oral Pathol Oral Radiol.2021;131:415-421.
- Kapourani A, Kontogiannopoulos KN, Barmpalexis P. A review on the role of pilocarpine on the management of xerostomia and the importance of the topical administration systems development. Pharmaceuticals (Basel). 2022;15:762.
- Su N, Marek CL, Ching V, Grushka M. Caries prevention for patients with dry mouth. J Can Dent Assoc. 2011:77:b85.
- Pärnänen P, Lomu S, Räisänen IT, Tervahartiala T, Sorsa T. Effects of fermented lingonberry juice mouthwash on salivary parameters—a one-year prospective human intervention study. Dent J (Basel). 2022;10:69.
- Lynge Pedersen AM, Belstrøm D. The role of natural salivary defenses in maintaining a healthy oral microbiota. J Dent. 2019;80 Suppl 1:S3-S12.
- American Dental Association. Xerostomia (Dry mouth). Available at ada./rg/resources/ada-library/oral-health-topics/xerostomia#:~:text=A%20thorough%20extraoral%20and%20intraoral,or%20blood%20and%20microbial%20tests. Accessed December 5, 2024.
- The Oral Cancer Foundation. The Role of Dental and Medical Professionals. Available at oralcancerfoundation.org/dental/role-dental-medical-professionals. Accessed December 5, 2024.
- Gehrig JS. Patient Assessment Tutorials: A Step-By-Step Guide for the Dental Hygienist. 4th ed. Burlington, Massachusetts: Jones and Bartlett Learning; 2020.
From Dimensions of Dental Hygiene. January/February 2025; 23(1):32-35.