 AGEPHOTOGRAPHY/ISTOCK/GETTY IMAGES PLUS
AGEPHOTOGRAPHY/ISTOCK/GETTY IMAGES PLUS
Managing Dental Unit Water Systems
Ensuring safe treatment water for routine and surgical procedures requires dental teams to implement effective management strategies for dental unit water systems.
Part 1 of a two-part series. This is the first article in a two-part series exploring management strategies for dental unit waterlines. Appearing in a future issue, Part 2 will focus on specific approaches and recommendations for waterline maintenance and testing to ensure safe treatment.
Fueled by research and backed by practical recommendations from the United States Centers for Disease Control and Prevention (CDC) and professional dental organizations, such as the Organization for Safety, Asepsis and Prevention (OSAP), the topic of dental safety is gaining prominence among practitioners and patients. Safe treatment during routine and surgical procedures requires dental teams to implement effective protocols—and a trifecta for action is in place. First, dental risks for infection are increasingly understood. Second, oral health professionals have actionable solutions for managing those risks. Third, professional guidance, accepted standards, and legal directives are available. Within this context, management of dental water quality is a necessary and expected component of every dental visit.
Unfortunately, not all offices have implemented protocols that meet today’s standards for maintaining, treating, and testing water systems to ensure safe treatment. In this first installment of a two-part series, this article will present an overview of dental unit waterline (DUWL) management recommendations and resources to assist offices in complying with dental water system safety standards.
Naturally occurring waterborne floating (ie, planktonic) microorganisms form biofilms on virtually every moist surface, including lakes and rivers, plants and soil, and live and dead tissue. These biofilms foul environments and structures, including plumbing, heating/ ventilation systems, and equipment.1–9 Biofilms are communities of mixed bacterial and fungal species attached by a self-produced, slimy, and primarily polysaccharide-based matrix, and release microbes and their by-products to passing fluids.10,11 Not all biofilms are harmful, as some benefit ecosystems and may be vital to the microbiomes of living hosts.12 Purposeful management of specific biofilms to accomplish environmental- and health-related goals is a growing area of research and product development.
Management of biofilm contamination of dental equipment should be considered within the context of a much larger topic—the inevitable and natural growth of biofilm where conditions support it. While public drinking water has been treated with filtration and chlorination for many years, outbreaks of waterborne illnesses continue to be reported from water used for drinking, recreation, heating, and cooling, as well as water-related equipment and devices.4–7 Most cases of health care-related waterborne illnesses are reported in hospitals; however, reports of exposures related to dental unit water are increasingly common.13,14
CONDITIONS THAT PROMOTE BIOFILM
Dental irrigants flow slowly and intermittently through long and complex, narrow-diameter plastic tubing, enhancing the release of biofilm organisms into the fluid. The large surface area of the tubing relative to the small volume of liquid facilitates contact of fluids to the tubing surfaces. Essentially, DUWLs are biofilm incubators due to narrow-bore plastic tubing and slow or stagnant water movement—all of which amplify microbial growth. The use-patterns of dental handpieces, air/ water syringes, and scalers create stagnant water within DUWLs 94.5% to 99.6% of the time, even in lines that are used daily. In addition, nonsmooth or discontinuous tubing promotes biofilm attachment and growth.13,15 The complex configuration of waterlines inside dental units includes joints, bends, and turns where biofilms easily attach. This confluence of intersecting pathways leads to the establishment of biofilms in areas that remain hidden from flushing and/ or regular water flow or treatment efforts with antimicrobial agents. Dental water systems may also contain “dead legs” or unused/ capped-off lengths of tubing that provide a constant source of biofilm to connected lines.
An example of this is a slow-speed handpiece line: 50% of these lines have a waterline that is capped off at the terminal end (near the handpiece connector). Stagnant water resides in the line and will seed the system with biofilm organisms. Older dental units may have been repaired, adjusted, or reconfigured over time. Capped-off or abandoned tubing is likely to contain established biofilm.16 Temperature may also encourage microbial water contamination, as heated irrigant systems are known to encourage microbial growth.16 These physical features partially explain three issues. First, treating DUWL contamination may not be 100% successful every time. Second, there is a need to test and validate the effectiveness of the office’s DUWL maintenance protocol. Third, dental unit design precludes the delivery of sterile water through dental units; hence, surgical procedures must be performed using sterile fluids delivered through sterile devices that bypass the dental unit altogether.13,15
There is documented risk from exposure to DUWLs.13,17,18 Microbial contamination in recently installed DUWLs can reach ≤ 200,000 colony forming units per milliliter (CFU/ ml), and the route of exposure from DUWLs is primarily inhalation/ aspiration and lavage.18 While human-derived organisms have been reported in the literature, most DUWL contaminants are natural in aquatic environments and are considered harmful in high concentrations, especially when susceptible individuals are exposed.18 Opportunistic human pathogens found in DUWLs include Pseudomonas aeruginosa, nontuberculous mycobacteria, and Legionella species. Cases of infections from each of these bacterial species derived from DUWLs have been reported, resulting in two well-documented deaths from Legionella exposure. Beyond these cases, two clusters of serious infections with Mycobacterium abscessus following pediatric pulpotomies involved more than 127 patients in Anaheim, California, and Atlanta. Infected patients faced abscesses, surgeries, long hospitalizations, and intravenous antibiotics, with serious side effects that included loss of sections of jawbone.19–21 In addition to infections, Gram-negative heterotrophic biofilm species may release high levels of lipopolysaccharides (LPS, or endotoxins) that can be linked with asthma, skin rashes, gastrointestinal reactions, and delayed wound healing. Presence of LPS may be related to live or dead organisms.15
PROFESSIONAL STANDARDS, RECOMMENDATIONS, AND LAWS
Public awareness, professional consensus, and regulatory changes directly related to the aforementioned cases have impacted standards of practice by providing evidence to justify dental treatment water recommendations and regulations.15,22,23
The CDC provides the most widely recognized and frequently referenced comprehensive body of research and recommendations for dental safety.22,23 In its Guidelines for Infection Control in Dental Health-Care Settings—2003, the CDC suggests that dental teams:
- Use water that meets the CDC-recommended limit for dental procedural water (ie, < 500 CFU/ ml of heterotrophic water bacteria) for routine dental treatment
- Consult with the dental unit manufacturer regarding appropriate methods, agents, and equipment for maintaining CDC-recommended dental water quality
- Follow recommendations for monitoring water quality, as provided by the manufacturer of the unit or waterline treatment product
- Discharge waterlines and air lines for a minimum of 20 seconds to 30 seconds after each patient, from any device connected to the dental water system that enters the patient’s mouth (eg, handpieces, ultrasonic scalers, and air/ water syringes)
- Consult with the dental unit manufacturer on the need for periodic maintenance of antiretraction mechanisms
- In case of a boil-water advisory, avoid using water from the municipal water system through dental equipment, or for handwashing or contact with any patient-care items until the advisory is lifted and post-advisory flushing and disinfection instructions are followed. Engineering solutions (such as separate water reservoirs that isolate dental devices from municipal water systems) may be used.22
The 2016 update to that document, the CDC’s Summary of Infection Prevention Practices in Dental Settings: Basic Expectations for Safe Care 2016, includes a dental waterline section with additional recommendations. The update also offers dental teams a mobile app and checklist that are useful in managing clinical water safety protocols:
- All dental units should use systems that treat water to meet safe drinking water standards (ie, < 500 CFU/ ml of heterotrophic water bacteria) for routine dental treatment. Independent reservoirs—or water-bottle systems—alone are not sufficient.
- Commercial products and devices can improve the quality of water used in dental treatment; consult with the dental unit manufacturer for appropriate water maintenance methods and recommendations for monitoring dental water quality.
- During surgical procedures, use only sterile solutions as a coolant/ irrigant, delivered with an appropriate device, such as a sterile bulb syringe, sterile tubing that bypasses DUWLs, or sterile, single-use devices. Examples of surgical procedures include biopsy, periodontal surgery, apical surgery, implant surgery, and surgical extractions of teeth.
- Written policies and procedures should be available outlining the office’s response to a community boil-water advisory.23
Both the CDC’s 2003 recommendations and 2016 summary should be foundational elements of every facility’s written infection prevention program. These recommendations specify outcomes (such as water quality standards) and standard operating procedures (step-by-step directions to comply). It is important that each member of the dental team understands how to perform each step and why it is important. Additionally, clinicians may wish to communicate this standard to patients in a way that informs them of the office’s commitment to safe treatment.
Some state dental boards have adopted, or are in the process of adopting, laws for dental water management, and these rules can be expected to reference the CDC recommendations—and, in some cases, add specific required protocol to meet CDC outcomes.
MAINTENANCE AND MONITORING
Regular DUWL maintenance and clinical monitoring of water quality should be performed to confirm success, or identify failures in protocol and potential problems. The CDC and OSAP recommend using DUWL tests as action limits (ie, to measure and prompt maintenance procedures, including shocking).15 Waterline cleaners and germicides fall into two main categories: shock products used to remove established, attached biofilm, and low-level germicides used to reduce planktonic organisms and retard biofilm attachment and growth. Available in various systems, the latter treatments are safe to use during patient care and should be a constant presence in properly maintained DUWLs.
Two testing methods are available: in-office sampling and laboratory testing. In-office methods are simple, convenient, and cost less than lab tests, but have been found to provide more limited and less reliable results.24,25 Available from dental supply companies, in-office tests may prove useful as quick checks for well-managed waterlines between more reliable lab tests to provide early warning of protocol failures.13,15,24,25
When using professional laboratories for testing, dental offices must follow directions for aseptic collection of samples and shipping to the lab. The lab should process the samples and provide results similar to sterilizer monitoring reports. With either testing method, DUWL test records should be logged. Professional dental waterline testing companies and universities may provide consulting services that assist offices in correcting errors, and it has been shown that repeated testing with professional guidance leads to improved test results.
RESOURCES FOR DENTAL TEAMS
One of the most current and comprehensive papers on dental waterline contamination and management was recently published in the Journal of Dental Infection Control and Safety, “Dental Unit Water Quality: Organization for Safety, Asepsis and Prevention White Paper and Recommendations—2018.”15 Designed to update and replace previous 1997 and 2000 OSAP white papers on DUWLs, it represents an internationally recognized voluntary consensus standard, as developed by experts from OSAP, CDC, US Environmental Protection Agency (EPA) and US Food and Drug Administration (FDA).15 While not law, it establishes best practices and guidance to manufacturers, regulatory agencies, and clinicians. Agencies with regulatory authority, including the EPA and FDA, may use voluntary consensus standards in lieu of government-specific documents (except where inconsistent with law or otherwise impractical).
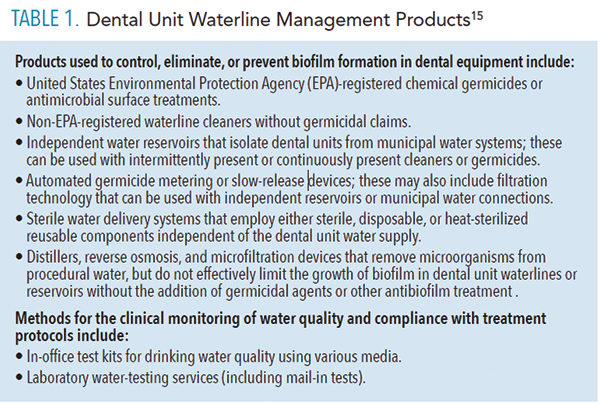
Most DUWL maintenance recommendations refer clinicians to the manufacturer’s instructions for use. Dental manufacturers are responsible for providing equipment and products that promote DUWL safety assurance; however, many have yet to prepare complete instructions for waterline care. Additionally, directions regarding testing and initial or routine shocking and treatment are inconsistent between manufacturers. Because dental teams are ultimately responsible for patient safety and liable for unsafe treatment water, it is incumbent on each practice to implement DUWL maintenance, treatment, and testing protocols that meet today’s standard of care (Table 1).
 While the frequency of dental water testing is not currently regulated and manufacturers may not offer consistent instructions, CDC and OSAP recommendations provide general guidance relating to events, use patterns, and test results.13,15,22,23 Although few laws directly govern dental water quality to date, the abundance of information, acknowledgement of risk and liability, and increased awareness of clinician and patient safety are driving improved compliance.
While the frequency of dental water testing is not currently regulated and manufacturers may not offer consistent instructions, CDC and OSAP recommendations provide general guidance relating to events, use patterns, and test results.13,15,22,23 Although few laws directly govern dental water quality to date, the abundance of information, acknowledgement of risk and liability, and increased awareness of clinician and patient safety are driving improved compliance.
CONCLUSION
Managing DUWLs consistently and effectively requires a culture of safety, investing in a system for maintenance and treatment, and assessing the results through regular testing. In clinical practice, dedication to waterline management is just one example of a dental team’s commitment to providing the safest care possible.
BOTTOM LINE
- In order to provide safe care during routine and surgical dental procedures, effective management of dental water quality is a necessary and expected component of every oral health visit.
- Dental unit waterlines (DUWLs) are biofilm incubators due to narrow-bore plastic tubing and slow or stagnant water movement—all of which amplify growth of potentially pathogenic microorganisms.
- Dental water systems may also contain “dead legs” or unused/capped-off lengths of tubing; stagnant water resides in these lines and will seed the system with biofilm organisms.
- Equipment design precludes the delivery of sterile water through dental units; hence, surgical procedures must be performed using sterile fluids delivered through sterile devices that bypass the dental unit altogether.13,15
- Regular DUWL maintenance and clinical monitoring of water quality should be performed to confirm success or identify failures in waterline management protocols.
- Because dental teams are ultimately responsible for patient safety, it is incumbent on each practice to implement DUWL maintenance, treatment, and testing protocols that meet today’s standard of care.
REFERENCES
- Mortensen KP, Conley SN. Film fill fouling in counterflow cooling towers: mechanisms and design. CTI J. 1994;15:10.
- Väisänen OM, Weber A, Bennasar A, Rainey FA, Busse HJ, Salkinoja-Salonen MS. Microbial communities of printing paper machinesJ J Appl Microbiol. 1998;84:1069–1084.
- Wirtanen G, Salo S. Disinfections in food processing—efficacy testing of disinfectants. Rev Environ Sci and Bio Technol. 2003;2:293–306.
- Olliver B, Magot M. Petroleum Microbiology. Washington DC: ASM Press; 2005.
- Coetser SE, Cloete TE. Biofouling and biocorrosion in industrial water systems. Crit Rev Microbiol. 2005;31:213–232.
- Costerton JW, Stewart PS, Greenberg EP. Bacterial biofilms: a common cause of persistent infections. Science. 1999;284:1318–1322.
- Hall-Stoodley L, Costerton JW, Stoodley P. Bacterial biofilms: from the natural environment to infectious diseases. Nat Rev Microbiol. 2004;2:95–108.
- Percival SL, Bowler P, Woods EJ. Assessing the effect of an antimicrobial wound dressing on biofilms. Wound Repair Regen. 2008;16:52–57.
- US Centers for Disease Control and Prevention. Mycobacterium abscessus in Healthcare Settings. Available at: http/ :/ / www.cdc.gov/ hai/ organisms/ mycobacterium.html. Accessed February 26, 2019.
- Donlan RM, Costerton JW. Biofilms: survival mechanisms of clinically relevant microorganisms. Clin Microbiol Rev. 2002;15:167–193.
- Costerton JW. Overview of microbial biofilms. J Ind Microbiol. 1995;15:137–140.
- Hirschfeld J. Dynamic interactions of neutrophils and biofilms. Oral Microbiol. 2014;6:26102.
- Dewhirst N, Molinari JA. Treating and monitoring dental water. Compend Contin Educ Dent. 2018;eBook:11–21.
- Craun GF, Brunkard JM, Yoder JS, et al. Causes of outbreaks associated with drinking water in the United States from 1971 to 2006. Clin Micro Rev. 2010;23:507–528
- Mills SE, Porteous N, Zawada J. Dental unit water quaility: Organization for Safety, Asepsis and Prevention white paper and recommendations—2018. Available at: https:/ / osapjdics.scholasticahq.com/ article/ 5075-dental-unit-water-quality-organization-for-safety-asepsis-and-prevention-white-paper-and-recommendations-2018. Accessed February 26, 2019.
- Mills SE. Dental unit water and air challenges. In: Molinari JA, Harte JA, eds. Cottone’s Practical Infection Control in Dentistry. 3rd ed. Philadelphia, Pa: Wolters Kluwer/ Lippincott Williams and Wilkins; 2010:63–75.
- Ricci ML, Fontana S, Pinci F, et al. Pneumonia associated with a dental unit waterline. Lancet. 2012;379:684.
- Molinari JA. The ongoing challenge of waterborne infections. Inside Dent. 2017;13:52–58.
- Peralta G, Tobin-D’Angelo M, Parham A, et al. Notes from the field: Mycobacterium abscessus infections among patients of a pediatric dentistry practice—Georgia, 2015. MMWR Recomm Rep. 2016;65:355–356.
- Hatzenbuehler LA, Tobin-D’Angelo M, Drenzek C, et al. Pediatric dental clinic—associated outbreak of Mycobacterium abscessus infection. J Pediatric Infect Dis Soc. 2017;6:e116–e22.
- American Dental Association. Nontuberculous Mycobacterial Infection Linked to Pulpotomy Procedures and Possible Dental Waterline Contamination Reported in California and Georgia. (September 21, 2016).
- Kohn WG, Collins AS, Cleveland J, Harte JA, Eklund KJ, Malvitz DM. Guidelines for Infection Control in Dental Health-Care Settings—2003. MMWR Recomm Rep. 2003;52(RR17):1–61.
- US Centers for Disease Control and Prevention. Summary of Infection Prevention Practices in Dental Settings: Basic Expectations for Safe Care. Available at: https:/ / www.cdc.gov/ oralhealth/ infectioncontrol/ guidelines/ index.htm. Accessed February 26, 2019.
- Karpay RI, Plamondon TJ, Mills SE. Comparison of methods to enumerate bacteria in dental unit water. Curr Microbiol. 1999;38:132–134.
- Momeni SS, Tomline N, Ruby JD, Dasanayake AP. Evaluation of in-office dental unit waterline testing. Gen Dent. 2012;60:e142–e147.
From Dimensions of Dental Hygiene. March 2019;17(3):16–18,21–22.

