 LIGHTFIELDSTUDIOS/ISTOCK/GETTY IMAGES PLUS
LIGHTFIELDSTUDIOS/ISTOCK/GETTY IMAGES PLUS
Improving Visual Acuity
Whether age or digital exposure is affecting a clinician’s vision, strategies are available to improve eyesight.
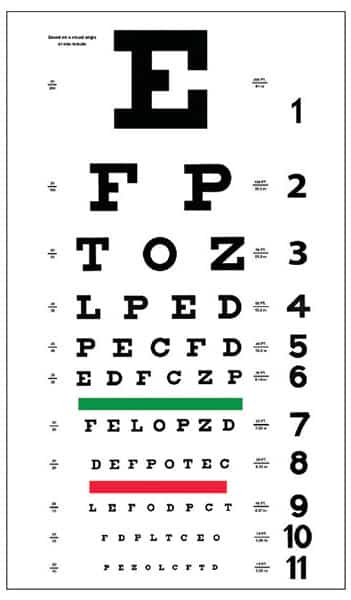
Visual acuity is defined as the clarity or sharpness of vision measured at a distance of 20 feet.1 Typically, the clarity of vision is measured by the ability to distinguish different sized letters or shapes at a fixed distance, usually with a Snellen chart (Figure 1).2 Normal visual acuity is rated as 20/20 vision.1,2 Visual impairment is defined as acuity less than 20/60, and blindness as visual acuity worse than 20/400.3,4
In dentistry, optimal visual acuity is vital for the assessment and treatment of patients. It is imperative to have a clear and a focused field of vision to be able to evaluate oral tissue conditions, accurately evaluate periodontal measurements, assess radiographs, and detect oral disease. Oral health professionals, such as dentists and dental hygienists, are at risk for increased eyestrain and reduced visual acuity over the course of their careers due to the influence of age on visual functioning and the increased use of technology in the dental setting, which causes digital eyestrain.5,6 Thus, oral health professionals need to be aware of visual acuity changes that can occur throughout their lifetimes and make necessary adjustments to maintain optimal clinical performance.
CAUSES OF VISUAL IMPAIRMENT
Visual impairment and blindness increase substantially with age.4 Presbyopia is an age-related vision condition in which the eye gradually loses the ability to focus on near objects.7 A refractive error of the eye, presbyopia indicates that the eye does not correctly bend light, resulting in a blurred image.8 Other refractive errors include myopia (nearsightedness), hyperopia (farsightedness), and astigmatism (asymmetric cornea curvature).8 Refractive errors can be easily diagnosed, measured, and corrected with glasses to attain normal vision.9 If they are not corrected or the correction is inadequate, however, refractive errors become a major cause of low vision and blindness.3,4
Oral health professionals need good visual acuity to focus at a short distance (27 cm to 50 cm) on the oral cavity.10 Moreover, the eye must be able to quickly accommodate (change its focus) to an intermediate distance (40 cm to 90 cm) to instruments, records, and radiographs in a fixed location, such as a table or a computer screen.10 Refractive errors impede the clinician from the flexibility to visually adapt, and, thus, optical assistance becomes necessary.10
STRATEGIES TO IMPROVE VISUAL ACUITY
The most common occupational hazard in dentistry is eyestrain.10 Research shows that 87% of dentists will experience some type of eyestrain, and 90% will require visual assistance at some point.10 Visual deficiencies can be compensated with the use of optical magnification aids such as loupes. Galilean loupes are common in dentistry, with magnification ranging from 2.5 x to 3.5 x, and an adjustable working distance to meet the clinician’s ergonomic needs.5,11 Galilean loupes, however, offer a limited field of view. Conversely, Keplerian or prismatic loupes allow for various magnifications and working distances with a preferred range of 3.5 x to 6 x, but they are heavier and usually higher priced than Galilean loupes.5,11 According to Perrin et al,11 there is a trade-off between optics and ergonomics when choosing loupes. Galilean loupes offer mainly ergonomic advantages for younger clinicians and compensate presbyopia in clinicians older than 40.11 Whereas, the Keplerian loupe enables significantly better detail detection in all age groups.11 Also, a new type of loupe is available that claims to provide 3.5 x magnification with a large field of view.
The angulation and alignment of loupes must be custom fit to the clinician to help prevent eyestrain. Additionally, illumination is an important factor. Enhanced illumination increases both the depth of field and visual acuity.5,11 Although oral health professionals with presbyopia can compensate by using magnification devices, they may not be able to achieve the same visual acuity as they had in their youth.5,11
Today, with an increase in technology use, many individuals experience symptoms of digital eyestrain.6 Nearly 80% of Americans report using digital devices for more than 2 hours daily, and 59% attest to experiencing digital eyestrain.6 The most common indicators of digital eyestrain are headaches, dry eyes, blurred vision, and neck and shoulder pain.6 Increasingly, oral health professionals are using technology when treating patients. Digital radiography, intraoral scans, electronic health records, and prescription and insurance databases are used in the day-to-day functions of the dental team. The combined use of these technologies in the dental practice increases computer screen time, which may raise digital eyestrain risk.
To alleviate digital eyestrain, eyewear—including contact lenses with magnification, blue-light filtering, and anti-reflective capabilities—are recommended.6 In addition, other solutions to reducing digital eyestrain include: taking frequent breaks, reducing overhead lighting to decrease screen glare, increasing text font, and maintaining proper viewing distance from the digital device.6 Oral health professionals should have near vision tested regularly, and discuss their digital activities with an eye care provider to relieve eyestrain and to support visual acuity.
LOUPES IN DENTAL HYGIENE CURRICULA
The addition of magnification loupes in dental hygiene curricula should be considered, as their use may enable students to better assess clinical details, as well as the overall oral health status of patients.12 Although loupes are being used in private clinical practice to improve ergonomics, reduce musculoskeletal disorders, and to enhance visual acuity, historically, they have not been routinely implemented in dental hygiene educational programs.13
Research suggests that injuries caused by musculoskeletal disorders can be minimized or prevented with the use of appropriate equipment such as loupes and lights. This combination can also reduce cognitive and physical stress by creating a safe, healthy, and comfortable workspace for dental hygienists. Additionally, loupes help visual acuity and diminish the potential decline in the dental hygienists’ vision over time with the early incorporation of loupes, when properly fitted to each individual dental hygienist.13
Consequently, loupes may better prepare future dental hygienists to meet the progressively multifaceted oral health care needs of the public and influence student and faculty retention via the promotion of musculoskeletal health, quality of work, and a productive work-life balance.12 The use of loupes and lights may benefit both students and faculty in dental hygiene programs. Loupes can aid in reinforcing proper ergonomics, musculoskeletal health, and greater visual acuity with less eyestrain. This could result in prolonged physical health, longer dental hygiene careers, and greater visual acuity.12
CONCLUSION
Using magnification aids, such as loupes, helps increase visual acuity. The influence of age, eyestrain, and leading causes of visual impairment and blindness suggest that the visual performance, detail detection, and precision of oral health professionals could be in jeopardy throughout their professional careers.3,4,11 Clinicians should be aware of methods to compensate for visual deficiencies and improve visual acuity. Additionally, Maillet et al14 found that implementing the early use of loupes could lead to improved ergonomics and visual acuity for dental hygiene students. While, there are additional financial implications, all dental hygiene students and faculty should be provided with loupes at the start of their dental hygiene curricula.14
REFERENCES
- American Optometric Association: Visual Acuity FAQs. Available at: aoa.org/patients-and-public/eye-and-vision-problems/glossary-of-eye-and-vision-conditions/visual-acuity/visual-acuity-faqs. Accessed May 16, 2019.
- Miller-Keane Encyclopedia and Dictionary of Medicine, Nursing, and Allied Health. Visual Acuity. Available at: https://medical-dictionary.thefreedictionary.com/visual+acuity. Accessed May 16, 2019.
- Resnikoff S. Pascolini D, Mariotti SP, Pokharel GP. Global magnitude of visual impairment caused by uncorrected refractive errors in 2004. Bull World Health Organ. 2008;86:63–70.
- Sommer A. Visual impairment. Access Science. Available at: accessscience.com/content/visual-impairment/734050. Accessed May 16, 2019.
- Eichenberger M, Perrin P, Neuhaus K, Lussi A, Bringolf U. Influence of loupes and age on the near visual acuity of practicing dentists. J Biomed Opt. 2011;16:035003.
- The Vision Council. Digital Eyestrain. Available at: thevisioncouncil.org/content/digital-eye-strain. Accessed May 16, 2019.
- American Optometric Association. Glossary of Common Eye and Vision Conditions. Available at: aoa.org/patients-and-public/eye-and-vision-problems/glossary-of-eye-and-vision-conditions#presbyopia. Accessed May 16, 2019.
- Kellogg Eye Center. Refractive Errors. Available at: umkelloggeye.org/conditions-treatments/refractive-errors. Accessed May 16, 2019.
- The World Health Organization. Blindness and Vision Impairment. Available at: who.int/en/news-room/fact-sheets/detail/blindness-and-visual-impairment. Accessed May 16, 2019.
- Burton JF, Bridgman GF. Eyeglasses to maintain flexibility of vision for the older dentist: the Otago dental lookover. Quintessence Int. 1991;22:879–882.
- Perrin P, Eichenberger M, Neuhaus KW, Lussi A. Visual acuity and magnification devices in dentistry. Swiss Dent J. 2016;126:222–235.
- Congdon LM, Tolle SL, Darby M. Magnification loupes in U.S. entry-level dental hygiene programs—occupational health and safety. J Dent Hyg. 2012;86:215–222.
- Arnett M, Gwozdek A, Ahmed S, Beaubien H, Yaw K, Eagle I. Assessing the use of loupes and lights in dental hygiene educational programs. J Dent Hyg. 2017;91:15–20.
- Maillet J, Millar M, Burke J, Maillet M, Maillet W, Neish N. Effect of magnification loupes on dental hygiene student posture. J Dent Educ. 2008.72:33–44.
From Dimensions of Dental Hygiene. June 2019;17(6):21–22,24.

