
Implementing the 2017 Periodontal Classification System
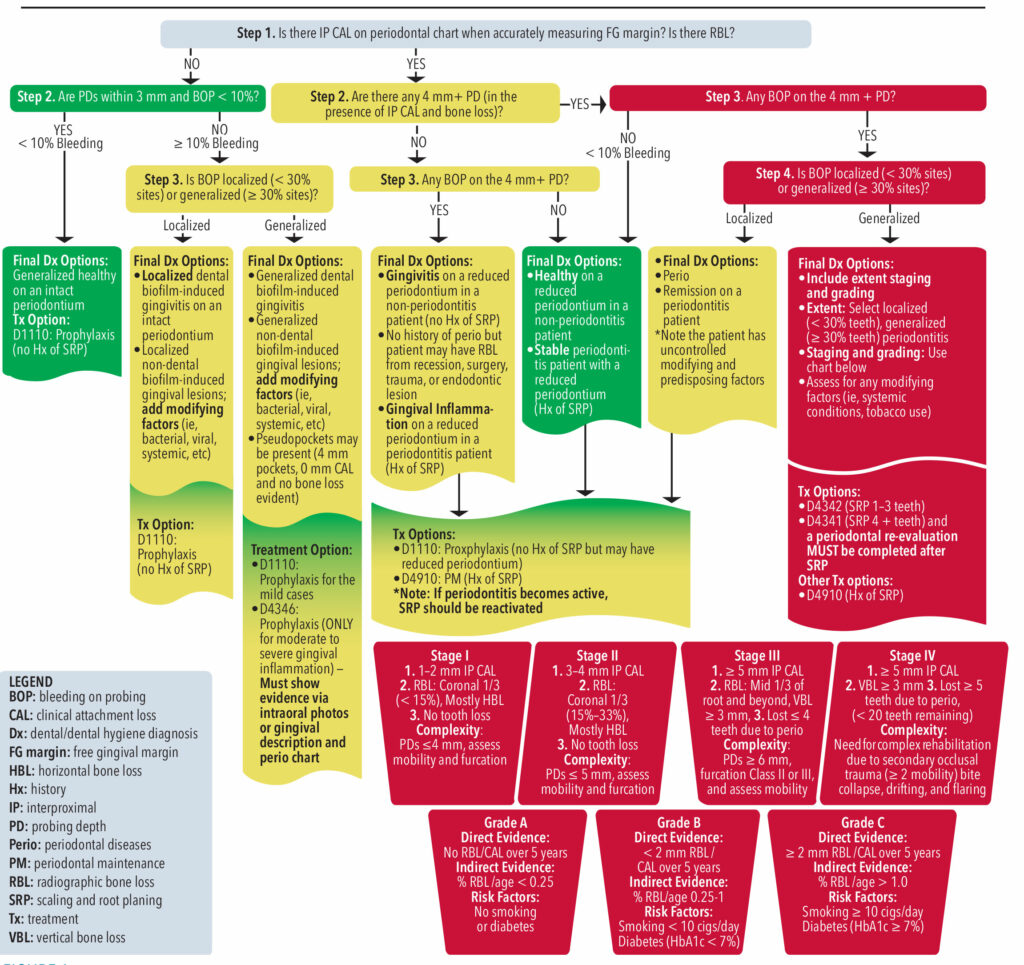
This chairside guide is designed to help clinicians classify and treatment plan according to these guidelines.
The “2017 American Academy of Periodontology (AAP) and European Federation of Periodontology Classification of Periodontal Diseases and Conditions” was created to guide the classification and treatment of periodontal diseases using clinical data.1 The classification system evaluates the extent, severity, and progression of periodontal diseases to help clinicians provide patient-specific care.2
As dental hygienists adapt to the new classification matrix, a call for more guidance on the interpretation and application of the system is needed to manage cases appropriately with correct treatment approaches. The chairside guide on page 18 is designed to simplify the use of the guidelines.
Step 1 asks whether there is evidence of clinical attachment loss (CAL) and/or radiographic bone loss (RBL). Steps 2 to 3 evaluate the presence of probing depths (PD) and bleeding on probing (BOP). The clinical data obtained from steps 1 through 3 help clinicians assign a periodontal classification, as well as formulate a treatment plan to best treat the given state of the periodontium.
Each of the steps appears in one of three colors: green meaning healthy, yellow noting gingival inflammation, and red representing active periodontitis
Green — Healthy
Periodontal health can be divided into two sub-categories: healthy with an intact periodontium (no CAL) and healthy on a reduced periodontium (presence of CAL).
Patients who are “healthy with an intact periodontium” will have the following characteristics: • No CAL, • No RBL,• BOP < 10% of sites, and • PDs: 1 to 3 mm.
Patients who are “healthy on a reduced periodontium” can be further divided into two subcategories: healthy on a reduced periodontium (no history of periodontitis) and stable periodontitis patient (history of periodontitis).
Patients who are “healthy on a reduced periodontium” and have no history of periodontitis present with the following characteristics: • Presence of CAL due to other factors (recession, surgery, trauma, endodontic lesion, etc), • Presence of RBL, PDs: 1 to 3 mm, • BOP < 10% sites with controlled modifying and predisposing factors
Patients who are “stable periodontitis” will meet the following criteria: • History of periodontitis, • Presence of CAL, • Presence of RBL • PDs: 1 to 4 mm and • Controlled modifying and predisposing factors.
There are two treatment options for the “healthy” category. For patients who are “healthy on an intact periodontium” or “healthy on a reduced periodontium” without a history of periodontitis, prophylaxis is recommended (D1110). However, if patients are diagnosed as “stable periodontitis,” periodontal maintenance is recommended (D4910).
Yellow — Gingival Inflammation
Gingival Inflammation can be present on an intact and reduced periodontium. Patients with “gingivitis on an intact periodontium” will exhibit the following characteristics: • No CAL, • No RBL, • BOP ≥ 10% of sites PDs: 1 to 4 mm, and • Uncontrolled modifying or predisposing factors
Patients with “gingival inflammation on a reduced periodontium” can be divided into three subcategories: gingivitis on a reduced periodontium (no history of periodontitis), gingivitis on a reduced periodontium with stable periodontitis (history of periodontitis), and periodontal disease remission (history of periodontitis).
Patients who are classified as “gingivitis on a reduced periodontium” without a history of periodontitis will exhibit the following characteristics: • Presence of CAL, • Presence of RBL, • PDs: 1 to 3 mm, • BOP ≥ 10% sites, and • Uncontrolled modifying and predisposing factors
Patients classified as “gingivitis on a reduced periodontium with stable periodontitis” will exhibit the following characteristics: • Presence of CAL, • Presence of RBL, • PDs: 1 to 3 mm, • BOP ≥ 10% sites, and • Controlled modifying and predisposing factors.
Patients who are “periodontal disease remission” will exhibit the following characteristics: • Presence of CAL, • Presence of RBL, • PDs: 1 to 4 mm, • BOP ≥ 10% sites, and • Uncontrolled modifying and predisposing factors.
For patients who exhibit “mild gingival inflammation on an intact periodontium,” prophylaxis is recommended (D1110). For patients who exhibit “moderate to severe gingival inflammation on an intact periodontium,” scaling in the presence of generalized moderate to severe gingival inflammation (D4346) is recommended. Periodontal maintenance (D4910) is recommended for patients who are “gingivitis on a reduced periodontium with stable periodontitis” or “periodontal disease remission.”
Patients in the yellow category generally have uncontrolled modifying or predisposing factors that put them at an increased risk for periodontal disease progression. These may include smoking, diabetes, obesity, genetic factors, medications, nutrition, chronic depression, lack of sleep, and chronic systemic inflammatory conditions.5-9
Red (Active Periodontitis)
Periodontitis exhibits the following characteristics: • Presence of interdental CAL, • Presence of interdental RBL, • Presence of BOP, and • Interdental PDs of ≥ 4 mm.
The presence of interdental PDs of ≥4 mm should be in conjunction with corresponding interdental CAL, RBL, and BOP to classify active periodontitis.
Three components are necessary to classify periodontitis: extent, stage, and grade.
Extent of periodontitis is characterized by localized (< 30% of teeth exhibit characteristics of periodontitis) and generalized (≥ 30% of teeth exhibit characteristics of periodontitis). Stage describes the severity of periodontitis as: • I: slight, • II: moderate , • III: severe, and • IV: severe; needs complex rehabilitation.
Stage I periodontitis exhibits the following characteristics: • 1 to 2 mm CAL, • Up to 15% RBL, and • PDs of ≤ 4 mm with BOP. S
Stage II periodontitis exhibits the following characteristics: • 3 to 4 mm CAL, • 15% to 33% RBL, and • PDs of ≤5 mm with BOP
Stage III periodontitis exhibits the following characteristics: • 5+ mm CAL, • ≥ 33% RBL, • PDs of ≥ 6 mm with BOP, and • Tooth loss due to periodontitis of ≤ 4 teeth.
Stage IV periodontitis exhibits the same clinical characteristics as Stage III with the need for complex rehabilitation and tooth loss due to periodontitis of ≥ 5 teeth.
Grade is assigned to identify the progression of disease as A: slow, B: moderate, and C: fast.2 Factors that can influence a patient’s grade include the presence and control of risk factors and systemic inflammation.4 The most reliable method of assessing disease progression is by assessing bone loss over time, which can be calculated using indirect evidence of percentage of bone loss divided by age. The bone loss/age ratio can be influenced by the presence of any disease modifiers.
The two risk factors with the most evidence relating to periodontitis are smoking and diabetes, which are included in the grading table. If a patient smokes < 10 cigarettes per day or has diabetes with an HbA1c of 7.0%, B is the minimal grade that can be assigned. If a patient smokes ≥ 10 cigarettes per day or has diabetes with an HbA1c ≥ 7.0%, a grade of C should be assigned.
Clinicians should also consider other risk factors that can be grade modifiers, such as obesity (BMI > 30), chronic inflammatory diseases, chronic depression, genetic factors, medications, nutrition, lack of adequate sleep, and other systemic conditions.5-9
Most “active periodontitis” cases begin with a nonsurgical treatment approach of scaling and root planing, which can be confined to one to three teeth (D4342) or ≥ four teeth (D4342) per quadrant. A periodontal evaluation should be completed 4 to 6 weeks after completing scaling and root planing, even if localized to one quadrant, to assess treatment outcomes and need for a referral to a periodontist. Patients with active periodontitis should be placed on a periodontal maintenance (D4910) schedule once nonsurgical and/or surgical therapy is complete.
Assessment of Early Radiographic Bone Loss
Radiographs provide a map for identifying any damage to the periodontium. Although radiography has limitations, X-rays can provide insight on alveolar bone changes as a result of periodontitis.
Bone loss due to periodontitis is detected on radiographs after the disease has progressed beyond the early stages. Two signs of early bone loss are: crestal irregularities, which indicate fuzziness at the crestal bone and triangulation, which shows the widening of the periodontal ligament space at interdental crestal bone.3
Attachment loss seen on radiographs should be verified clinically by measuring CAL. For active periodontitis cases, bone loss is an important component of determining the grade of a patient, as mentioned in the “active periodontitis” section.
Summary
Categorizing patients’ oral manifestations, etiological factors, and systemic risk factors into groups of “healthy,” “gingival inflammation,” and “active periodontitis” may reduce the confusion associated with using the 2017 AAP Guidelines. The interconnections made between oral cavity conditions and systemic conditions are a vital part of appropriately diagnosing and treatment planning.
References
- Abrahamian L, Pascual-LaRocca A, Barallat L, et al. Intra- and inter-examiner reliability in classifying periodontitis according to the 2018 classification of periodontal diseasesJ J Clin Periodontol. 2022;49:732–739.
- Papapanou PN, Sanz M, Buduneli N, et al. Periodontitis: consensus report of workgroup 2 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J Periodontol. 2018;89(Suppl 1):S173–S182.
- Gehrig JS, Shin DE, Willman DE. Foundations of Periodontics for the Dental Hygienist. 5th ed. Burlington, Massachusetts: Jones & Bartlett Learning; 2019.
- Kornman KS, Papapanou PN. Clinical application of the new classification of periodontal diseases: ground rules, clarifications and “gray zones.” J Periodontol. 2020;91:352–360.
- Suvan J, Petrie A, Moles DR, et al. Body mass index as a predictive factor of periodontal therapy outcomes. J Dent Res. 2014;93:49–54.
- Reynolds MA. Modifiable risk factors in periodontitis: at the intersection of aging and disease. Periodontol 2000. 2014;64:7–19.
- Ciancio SG. Medications as risk factors for periodontal disease. J Periodontol. 1996;67(10 Suppl):1055–1059.
- Martinon P, Fraticelli L, Giboreau A, Dussart C, Bourgeois D, Carrouel F. Nutrition as a key modifiable factor for periodontitis and main chronic diseases. J Clin Med. 2021;10:197.
- Alhassani AA, Al-Zahrani MS. Is inadequate sleep a potential risk factor for periodontitis? PLoS One. 2020;15:e0234487.
From Dimensions in Dental Hygiene. October 2023; 21(9):16-19

