How to Treat Intrinsic Stain
Ronald E. Goldstein, DDS, discusses the etiology and treatment of intrinsic stain, from fluorosis to tetracycline staining.
Q. How is microabrasion used to treat intrinsic stains?
A. Intrinsic stains are discolorations of the tooth structure resulting from ingestion of certain drugs during critical periods of tooth development, excessive exposure to fluorides, or exposure to certain dental restorative materials. Intrinsic stains are entirely contained within the tooth and cannot be eradicated with scaling or prophylaxis.
Dental fluorosis is the brownish enamel discoloration caused by over-exposure to systemic fluoride during tooth eruption. Dental fluorosis may respond to intense bleaching performed in-office, but in my opinion, the best treatment is a combination of microabrasion and bleaching therapy. Inventor Ted Croll, DDS, developed a technique that is available for dental offices* to remove this type of stain; it entails using a slow running handpiece with a pumice composed of a mild form of hydrochloric acid that can remove microns of enamel. When microabrasion is combined with bleaching, fluorosed stains can be either eliminated or reduced. In some patients with a mild form of fluorosis, one treatment may be enough, although multiple treatments may be necessary to remove darker stains and improve the tooth color significantly.
To be an effective modality, the patient should have sufficient thickness of enamel. If the enamel is too thin, the resulting shade may not be pleasing to the patient. One reason for this may be the underlying dentin showing through. Thus, a better treatment choice may be to suggest porcelain laminates to mask the tooth discoloration and provide the patient with the tooth color of his or her choice.
 Q. What about hypocalcified areas?
Q. What about hypocalcified areas?
A. Hypocalcified areas are discolorations of the teeth caused by a developmental interference with the normal matrix formation or calcification of the enamel. They are extra white stains and can look just as unsightly as fluorosis stains because they stand out like flood lights. If the surface stains are not too deep, they can be removed with microabrasion. Hypocalcified areas can sometimes be improved with cosmetic contouring or reshaping the enamel surface with a very fine micron diamond stone.**
The intra-oral camera with its intense bright light can transilluminate the tooth to determine how deep the stain may be. This procedure is useful to help discover any hidden microcracks in the enamel surface that may play a role when trying to eradicate these intrinsic stains. Bleaching over an extended period of time— up to 1 year—may be successful in improving the overall tooth shade. However, this is not guaranteed, since bleaching can also make the hypocalcified areas appear even whiter. When a patient presents with many hypocalcified areas, bonding with composite resin or masking with porcelain laminates may produce a more pleasing result for the patient.
 Q. How do you treat tetracycline staining?
Q. How do you treat tetracycline staining?
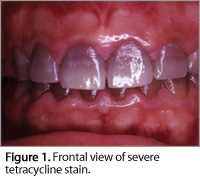
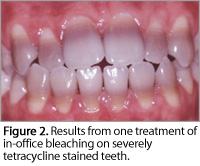
A. Tetracycline is a commonly used antibiotic that can cause severe tooth staining, either in early childhood when the teeth are in the development stages or in embryo (Figure 1). These are the most difficult stains to bleach. Children (up to 8 years old) can experience intrinsic darkening from ingesting a single dose. However, research by Medical College of Georgia School of Dentistry researcher Van Haywood, DMD, and others from the University of North Carolina, Chapel Hill, showed that in certain cases bleaching for up to 1 year may be effective in obtaining a lighter color in these types of stains (Figure 2).1-4 Haywood was the first to discover that extended periods of nightguard vital bleaching can make a difference.
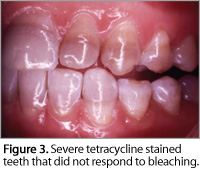
The bottom line is that tetracycline stained teeth can lighten with bleaching but the results may not meet the patient’s expectations; in some cases a grayish color may result as opposed to the desired white (Figure 3).
 If a year-long bleaching protocol is the treatment choice, I recommend using a sequence of bleaching gel that is composed of increasing concentrations of the whitening agent. For example, starting off with 10% carbamide peroxide, moving to 15%, and then finishing with 20%, if hypersensitivity isn’t a concern. If the patient has large pulps, using a 20% or even 15% bleaching gel might create too much sensitivity. Even if patients need to bleach every other day with a lower concentration due to sensitivity, bleaching up to a year does make a difference and can eliminate mild to moderate tetracycline stains. Now with newer compounds added to some of the bleaching formulas, such as amorphous calcium phosphate, sensitivity can be less of an issue.
If a year-long bleaching protocol is the treatment choice, I recommend using a sequence of bleaching gel that is composed of increasing concentrations of the whitening agent. For example, starting off with 10% carbamide peroxide, moving to 15%, and then finishing with 20%, if hypersensitivity isn’t a concern. If the patient has large pulps, using a 20% or even 15% bleaching gel might create too much sensitivity. Even if patients need to bleach every other day with a lower concentration due to sensitivity, bleaching up to a year does make a difference and can eliminate mild to moderate tetracycline stains. Now with newer compounds added to some of the bleaching formulas, such as amorphous calcium phosphate, sensitivity can be less of an issue.
In the final analysis, porcelain laminate veneers may be the best solution to adequately mask the stain and create the patient’s desired tooth color. An important element with veneers is the position and inclination of the teeth. For instance, if the patient’s teeth are protruding, veneers will generally not be as effective in masking the stain because as time passes, the underlying darker tooth structure tends to show through the laminates. The best indication for thin laminates are teeth that could benefit from slight “building out.” For teeth that are protruded, a better alternative may be an all ceramic crown, which can totally mask the tooth discoloration.
Q. Do you differentiate stains created from the oral administration of antibiotic tetracycline versus minocycline?
A. Tetracycline stains are incorporated in the dentin during calcification of the teeth. Therefore, adults appear to be able to use the antibiotic without risks of discoloration. However, minocycline, a semisynthetic derivative of tetracycline, causes staining on the teeth of adolescents or adults who take the drug orally for acne treatments. Unlike tetracycline, minocycline is absorbed through the gastrointestinal tract and combines poorly with calcium. Although these stains may be somewhat responsive to bleaching, porcelain laminates may yield a more satisfactory result since the final tooth color can match the patient’s previous tooth color better. Dental hygienists should inform their adult patients of the esthetic damages of taking even a single oral dose of minocycline.
 Q. Are there any other causes of intrinsic stains that dental hygienists may be less familiar with?
Q. Are there any other causes of intrinsic stains that dental hygienists may be less familiar with?
A. A large number of genetic conditions or childhood illnesses can cause various types of intrinsic staining. The dentist or dental hygienist should do a thorough diagnosis and review the patient’s history and radiographs to determine the effectiveness of any bleaching technique.
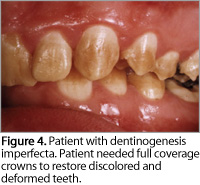
For instance, dentinogenesis imperfecta is a hereditary disorder of dentin development affecting the teeth. It has a variable effect on the color, shape, and wear of both primary and permanent teeth. This condition causes the teeth to be discolored and translucent (Figure 4).
Several childhood diseases may cause tooth discoloration. For example, the bluish-green primary teeth seen in children may be the result of post-natal staining of the dentin by bilirubin or biliverdin. The destruction of an excessive number of erythrocytes in the blood cells due to an RH factor incompatibility between mother and fetus can cause brownish teeth and people with porphyria (inherited or acquired disorders of certain enzymes in the heme biosynthetic pathway) may experience a purplish-brown tooth color caused by excess production of pigment. All of these conditions offer the same treatment dilemmas as tetracycline discoloration.
*Prema® Enamel Microabrasion System, Premier, Plymouth Meeting, Pa
**ET-6 diamond, Brasseler USA, Savannah, Ga
REFERENCES
- Haywood VB, Leonard RH, Dickinson GL. Efficacy of six-months of nightguard vital bleaching of tetracycline-stained teeth. J Esthet Dent. 1997;9:13-19.
- Leonard RH Jr, Haywood VB, Caplan DJ, Tart ND. Nightguard vital bleaching of tetracycline-stained teeth: 90 months post treatment. J Esthet Restor Dent. 2003;15:142-154.
- Haywood VB. Extended bleaching of tetracycline-stained teeth: a case report. Contemporary Esthetics and Restorative Practice. 1997;1:14-21.
- Haywood VB, Pohjola R. Bleaching and esthetic bonding of tetracycline-stained teeth. Contemporary Esthetics and Restorative Practice. 2004;8:16-24.
From Dimensions of Dental Hygiene. May 2007;5(5): 22-23.

