Exploring the Antigingivitis Armamentarium
The regular use of therapeutic mouthrinses may help reduce the risk of gingivitis and, ultimately, periodontal disease.
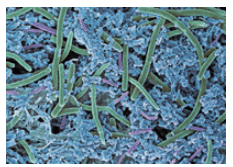
Biofilm is a complex, three-dimensional arrangement of bacteria—both Gram-negative and Gram-positive—that lives communally as a matrix system (Figure 1). When allowed to proliferate, anaerobic bacteria dominate. Oral biofilm is found in the oral cavity, on natural and artificial teeth/prostheses, and in dental unit waterlines. If pathogenic bacteria are allowed to thrive in the mouth, gingivitis is initiated, which can progress to periodontitis. Antimicrobial mouthrinses can be helpful in the effort to control biofilm, especially for patients with limited ability to effectively perform daily oral hygiene tasks.1–11
Toothbrushing and flossing are the traditional methods for controlling oral biofilm. Unfortunately, even with explicit self-care instructions provided by oral health professionals, 65% to 85% of the United States population does not brush effectively or for the recommended time of 2 minutes, instead brushing only between 30 seconds to 60 seconds.12–14 Studies have shown that only about 6% of Americans floss daily.15 As the US experiences a growing population of older adults, many of whom have chronic systemic conditions, designing oral hygiene regimens that can be conducted with limited dexterity is important.4 Mouthrinses can be a helpful adjunct for patients with motor control deficiencies, systemic disease, or poor biofilm control. Dental hygienists are charged with recommending the appropriate formulation for individual patient needs. Monitoring patient compliance is also important. Research has demonstrated that adding therapeutic mouthrinses as an adjunct to a patient’s daily oral health regimen decreases the number and vitality of pathogenic oral biofilm.9–11
There are many types of therapeutic mouthrinses available, either over-the-counter (OTC) or by prescription. The most commonly used active ingredients in therapeutic mouthrinses include chlorhexidine, cetylpyridinium chloride, delmopinol, and essential oils. The mechanism of action for these ingredients can lower the rate of new biofilm formation and decrease existing biofilm by penetrating the hydrophobic portion of the bacterial cell wall.8,9
CHLORHEXIDINE
Chlorhexidine has long been considered the gold standard among antiplaque agents. Multiple studies have demonstrated chlorhexidine’s efficacy against microbes and its substantivity, as well as its antibiofilm/antigingivitis properties.1–17 Chlorhexidine decreases pellicle formation by binding salivary mucins, inhibiting the microbial colonization of nascent biofilms.11 A clinical trial by Yévenes et al7 compared a 0.12% chlorhexidine mouthrinse containing alcohol, 0.12% chlorhexidine mouthrinse containing 0.05% sodium fluoride, 0.05% chlorhexidine mouthrinse containing 0.05% cetylpyridinium chloride, and 0.1% chlorhexidine gel product. Participants’ plaque levels were checked 24 hours after use. The researchers found that all chlorhexidine products were effective. The 0.1% chlorhexidine gel also appeared to be as effective as the 0.12% chlorhexidine mouthrinse, suggesting that multiple forms of chlorhexidine are useful. These results provide clinicians with a variety of options to recommend for chlorhexidine use. With prolonged use (more than 6 months), however, chlorhexidine can cause increased calculus formation, black/brown staining of the teeth, and may even alter taste sensation, any of which may interfere with patient compliance.6–9 Despite these shortcomings, chlorhexidine may be best suited for patients undergoing periodontal therapy, during which intensive short-term biofilm control can be critical.
CETYLPYRIDINIUM CHLORIDE
Cetylpyridinium chloride, a quaternary ammonium compound, has similar properties to chlorhexidine, as it interrupts the bacterial cell membrane, leading to cell death.7–9,11 Cetylpyridinium chloride also has plaque- and calculus-inhibiting effects. With broad antimicrobial action, cetylpyridinium chloride kills Gram-positive pathogens and yeast via disruption of bacterial cell membranes.1,2 It is most effective in concentrations between 0.045 ppm and 0.10 ppm. The higher the concentration, the greater reductions seen in plaque-induced gingivitis.8 The substantivity of cetylpyridinium chloride is approximately 3 hours to 5 hours, somewhat shorter than chlorhexidine.8,17 For patients who do not need chlorhexidine’s greater substantivity, an OTC cetylpyridinium chloride mouthrinse can be effective for daily use.
DELMOPINOL HYDROCHLORIDE
Delmopinol hydrochloride, while not considered an antimicrobial due to its inability to kill bacteria, interferes with the formation of biofilm—reducing the number of bacteria that attach to teeth surfaces. This results in less adherence of bacteria to each other and to the teeth.18 Research has shown that the regular use of a mouthrinse containing 0.2% delmopinol hydrochloride reduces plaque, bleeding on probing, and gingivitis.19–21 Clinicians may want to recommend a delmopinol mouthrinse to patients with heavy plaque biofilm accumulation, those undergoing orthodontic treatment, or patients in periodontal maintenance.22
ESSENTIAL OILS
Essential oils—including thymol, menthol, eucalyptol, and methyl salicylate—are able to disrupt cell membranes and work rapidly and nonselectively against Gram-positive and Gram-negative bacteria and fungi.11 Studies have shown that patients who used an essential oil mouthrinse as an adjunct to daily care experienced reduced bacterial loads.23,24 The substantivity of essential oils is less than chlorhexidine and cetylpyridinium chloride, so patients may need to use this mouthrinse more frequently to experience prolonged bactericidal activity.6 Charles et al6 found that chlorhexidine mouthrinse was significantly more effective against biofilm formation and gingivitis occurrence after 3 months and 6 months of use compared to a mouthrinse containing essential oils. However, the group that used the chlorhexidine mouthrinse experienced significantly more calculus and supragingival stain formation than the group that used the essential oils mouthrinse. Additionally, essential oils mouthrinses decrease oral malodor and the bacterial load surrounding dental implants. They have also been used as a subgingival irrigant and following periodontal surgery to encourage oral wound healing.25
ADDITIONAL OPTIONS
Other ingredients are also being tested for antimicrobial benefits, including chlorine dioxide, extract of pomegranate, pilu, bibhitaka, nagavalli, gandhapura taila, ela, peppermint satva, yavani satva, and lippia sidoides from the chamomile family.26 As additional research is conducted, more options may become available for OTC care.
Another interesting area of study is in 2-methacryloyloxyethyl phosphorylcholine, or MPC. These molecules possess polar phospholipids that act like a naturally occurring biomembrane, thereby reducing adsorption of proteins and adhesion of bacteria.27,28 MPC is currently used in cosmetics and contact lenses. One study demonstrated that an MPC mouthrinse reduced streptococcal adhesion to enamel.29 More research is needed, but MPC may provide an additional mouthrinse option.
INCLUSION OF ALCOHOL
Pharmaceutical alcohol (a highly purified aqueous solution typically containing 96% ethanol) is commonly added to mouthrinses to activate various ingredients and prolong shelf-life of the product.7,30,31 The debate over a possible association between alcohol in mouthrinses and oral cancer has been ongoing for more than 30 years. However, more than 18 epidemiologic studies regarding the use of mouthrinses containing alcohol and the risk of oral cancer found no statistically significant link between the two, regardless of frequency of use.31,32 Mouthrinses containing alcohol are contraindicated for patients younger than 12 and those with current or previous alcohol addiction.33,34 For individuals who prefer to avoid it, alcohol-free versions of chlorhexidine, cetylpyridinium chloride, and essential oil mouthrinses are available.
CONCLUSION
Clinicians must weigh the risks and benefits of mouthrinses as an adjunct for each patient’s oral self-care regimen. Recommendations should be tailored to individual patient needs. It should also be stressed to patients and caregivers that mouthrinses are not substitutes for daily toothbrushing and flossing.
REFERENCES
- Gurenlian JR. The role of dental plaque biofilm in oral health. J Dent Hyg. 2007;81(Suppl 1):116.
- Haps S, Slot D, Berchier C, Van der Weijden G. The effect of cetylpyridinium chloride?containing mouth rinses as adjuncts to toothbrushing on plaque and parameters of gingival inflammation: a systematic review. Int J Dent Hyg. 2008;6:290–303.
- Harris-Kojetin L, Sengupta M, Park-Lee E, Valverde R. Long-term care services in the United States: 2013 Overview. Vital Health Stat. 3. 2013;37:1–107.
- Ward BW. Prevalence of multiple chronic conditions among US adults: estimates from the National Health Interview Survey, 2010. Prev Chronic Dis. 2013;25:10.
- Rambhade S, Chakarborty A, Shrivastava A, Patil UK, Rambhade A. A survey on polypharmacy and use of inappropriate medications. Toxicol Int. 2012;19:68–73.
- Charles C, Mostler K, Bartels L, Mankodi S. Comparative antiplaque and antigingivitis effectiveness of a chlorhexidine and an essential oil mouthrinse: 6?month clinical trial. J Clin Periodontol. 2004;31:878–884.
- Yévenes I, Alvarez SR, Jara MN, Wolfenson PM, Smith LP. Comparison of mouthrinses containing chlorhexidine and other active agents with chlorhexidine mouthrinse gel: effects on de novo plaque formation. Revista Odonto Ciência. 2007;24(4):345–348.
- Versteeg P, Rosema N, Hoenderdos N, Slot D, Van der Weijden G. The plaque inhibitory effect of a CPC mouthrinse in a 3?day plaque accumulation model–a cross?over study. Int J Dent Hyg. 2010;8:269–275.
- Walters P, Sagel L. Brush, floss, and rinse: A third critical tool to improve gingival health. Contemporary Oral Hygiene. 2006;8(5):39–43.
- Weinberg M, Westphal C, Froum S, Palat M, Schoor R. Comprehensive Periodontics for the Dental Hygienist. Upper Saddle River, New Jersey: Prentice Hall; 2014.
- DiGangi P, Bendit J. It’s 80-20 with biofilm: update on oral rinses. Dent Today. 2012;31:58–63.
- Zeedyk M., Longbottom C, Pitts N. Tooth-brushing practices of parents and toddlers: a study of home-based videotaped sessions. Caries Res. 2005;39:27–33.
- Saxer U, Barbakow J, Yankell S. New studies on estimated and actual toothbrushing times and dentifrice use. J Clin Dent. 1997;9:49–51.
- McCracken G, Janssen J, Heasman L, Stacey F, Steen N, Heasman P. Assessing adherence with toothbrushing instructions using a data logger toothbrush. Br Dent J. 2005;198:29–32.
- Macgregor I, Balding J, Regis D. Flossing behaviour in English adolescents. J Clin Periodontol. 1998;25:291–296.
- Sekino S, Ramberg P, Guzin Uzel N, Socransky S, Lindhe J. The effect of a chlorhexidine regimen on de novo plaque formation. J Clin Periodontol. 2004;31:609-614.
- Carrilho MR, Carvalho RM, Sousa EN, et al. Substantivity of chlorhexidine to human dentin. Dent Mater. 2010;26:779–785.
- Addy M, Moran J, Newcombe RG. Metaanalyses of studies of 0.2% delmopinol mouth rinse as an adjunct to gingival health and plaque control measures. J Clin Periodontol. 2007;34:58–65.
- Lang NP, Hase JC, Grassi M et al. Plaque formation and gingivitis after supervised mouthrinsing with 0.2% delmopinol hydrochloride, 0.2% chlorhexidine digluconate and placebo for 6 months. Oral Dis. 1998;4:105–113.
- Hase JC, Attstrom R, Edwardsson S, Kelty E, Kisch J. 6-month use of 0.2% delmopinol hydrochloride in comparison with 0.2% chlorhexidine digluconate and placebo. (I). Effect on plaque formation and gingivitis. J Clin Periodontol. 1998; 25:746–753.
- Claydon N, Hunter L, Moran J, et al. 6-month home usage of 0.1% and 0.2% delmopinol mouthwashes. (I) Effect on plaque, gingivitis, supragingival calculus and tooth staining. J Clin Periodontol. 1996;23:220–228.
- Tilliss T. Improve oral health with mouthrinses. Dimensions of Dental Hygiene. 2013;11(5):66–69.
- Stoeken JE, Paraskevas S, Van Der Weijden GA. The long-term effect of a mouthrinse containing essential oils on dental plaque and gingivitis: a systematic review. J Periodontol. 2007;78:1218–1228.
- Fine D, Furgang D, Barnett M, et al. Effect of an essential oilcontaining antiseptic mouthrinse on plaque and salivary Streptococcus mutans levels. J Clin Periodontol. 2000;27:157–161.
- Claffey N. Essential oil mouthwashes: a key component in oral health management. J Clin Periodontol. 2003;30:22–24.
- Shivanand A, Sudhir Shetty V, Devarathnamma MV, Nagappa G, Archana D, Prachi P. Evaluation of antiplaque and antigingivitis effect of herbal mouthwash in treatment of plaque induced gingivitis: a randomized, clinical trial. J Indian Soc Periodontol. 2014;18:48–52.
- Hirota K, Murakami K, Nemoto K, Miyake Y. Coating of a surface with 2-methacryloyloxyethyl phosphorylcholine (MPC) co-polymer significantly reduces retention of human pathogenic microorganisms. FEMS Microbiol Lett. 2005;248:37–45.
- Hirota K, Yumoto H, Miyamoto K, et al. MPC-polymer reduces adherence and biofilm formation by oral bacteria. J Dent Res. 2011;90:900–905.
- Menezes SM, Cordeiro LN, Viana GS. Punica granatum (pomegranate) extract is active against dental plaque. J Herb Pharmacother. 2006;6:79–92.
- . Eldridge KR, Finnie SF, Stephens JA, Mauad AM, Munoz CA, Kettering JD. Efficacy of an alcohol-free chlorhexidine mouthrinse as an antimicrobial agent. J Prosthet Dent. 1998;80:685–690.
- Spolarich A, Gurenlian J. Dispel the myths. Dimensions of Dental Hygiene. 2013;11:20–24.
- . Gandini S, Negri E, Boffetta P, La Vecchia C, Boyle P. Mouthwash and oral cancer risk quantitative meta-analysis of epidemiologic studies. Ann Agric Environ Med. 2012;19:173–180.
- Gagari E, Kabani S. Adverse effects of mouthwash use: a review. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1995;80:432–439.
- . Lachenmeier DW, Gumbel?Mako S, Sohnius E, Keck?Wilhelm A, Kratz E, Mildau G. Salivary acetaldehyde increase due to alcohol?containing mouthwash use: a risk factor for oral cancer. Int J Canc. 2009;125:730–735.
From Dimensions of Dental Hygiene. November 2015;13(11):26–29.

