 SHIDLOVSKI/ISTOCK/GETTY IMAGES PLUS
SHIDLOVSKI/ISTOCK/GETTY IMAGES PLUS
Estrogen and Temporomandibular Disorders
Hormonal fluctuations may be a contributing risk factor for TMD-related pain.
This course was published in the January 2020 issue and expires January 2023. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Define and describe temporomandibular disorders (TMD).
- Discuss the significance of estrogen and TMD-related pain.
- Provide oral health professionals with recommendations on caring for patients with TMD.
Affecting the quality of life for more than 10 million Americans, temporomandibular disorders (TMDs) are musculoskeletal conditions associated with pain and dysfunction of the temporomandibular joint (TMJ) and muscles of mastication.1–3 The pain and dysfunction associated with TMDs are more prevalent among women during reproductive years, suggesting estrogen plays a role in TMD pathophysiology.1 Studies describe the potential role of hormonal fluctuations as a contributing risk factor for TMD-related pain.1,2 Furthermore, evidence suggests estrogen is a prominent hormone, influencing both inflammatory and pain processes.1,2
The pathogenesis of TMD, however, is not well understood. Known risk factors are occlusal abnormalities, macrotrauma to the TMJ, parafunctions (eg, clenching and bruxism), and psychological factors (eg, stress and anxiety).4 Commonly reported TMD-related symptoms include headaches, orofacial pain, toothaches, difficulty chewing, locking of the TMJ, and/or pain associated with talking.4,5 Dental radiographs, arthroscopy, and advanced imaging, such as computerized tomography scans and magnetic resonance imaging, are tools used in the diagnostic testing for TMDs. The Research Diagnostic Criteria for Temporomandibular Disorders (RDC/TMD) is a reliable algorithm-based classification system for TMDs.6
The presence and extent of TMD-related pain, which negatively impacts quality of life, can complicate caring for patients comprehensively.7 This article aims to describe the contemporary significance of TMDs and potential role of estrogen receptors on TMD-related pain, as well as provide oral health professionals with recommendations and limitations for caring for patients with TMDs.4
ESTROGEN’S MECHANISMS OF ACTION
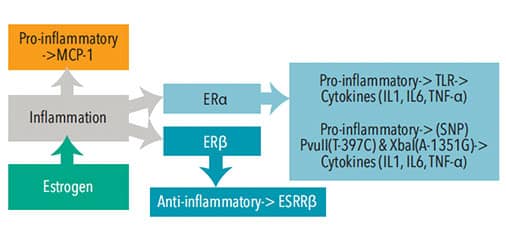
Estrogen can produce inflammation through various mechanisms of action including stimulation of toll-like receptors (TLR) in the immune system, upregulation of voltage-gated sodium channels, expression of estrogen receptors, or due to genetic variations called polymorphism.1,8–10 Figure 1 illustrates estrogen’s influence on the systemic inflammatory process.
Stimulation of TLR promotes inflammation by signaling leukocytes (monocytes and macrophages) and glial cells (immune cells in the central nervous system) to release pro-inflammatory messenger molecules known as cytokines.1,8,11 In 2009, Deshmane et al12 described how specialized cytokines, called chemokines, direct the migration of monocytes and macrophages to inflamed sites and suggest monocyte chemoattractive protein-1 is the primary chemokine that contributes to the initiation, progression, and inflammation in the TMJ. The involvement of TLR in the central nervous system suggests the presence of inflammation, demonstrating the potential for increased chronic pain.11 Specifically, estrogen receptors are present in the dorsal root ganglion and the trigeminal nerve nucleus.13 The levels of estrogen in these areas may alter function of the opioid systems, thereby increasing pain perception.8
Courtesy of Tran M. Luu, RDH, BSDH
In 2017, Bi et al10 investigated the correlation between estrogen and upregulation of voltage-gated sodium channels as a source of pain and inflammation with TMD. In particular, sodium channel 1.7 was theorized to trigger complete loss of pain if disrupted. Researchers found estrogen elevates sodium channel plasma, contributing to increased nociception and hyperalgesia, suggesting that the presence of estrogen may lead to TMD-related pain.10
Estrogen acts by binding two types of steroidal estrogen receptors: estrogen receptor alpha (ERα) and estrogen receptor beta (ERβ). Found in both the peripheral nervous system and central nervous system, these receptors are present in TMJ muscles.8,13 Research shows that higher levels of ERα expression could indicate more inflammation, and that lower levels of ERβ expression may also lead to increased inflammation.1 Within the synovium of the TMJ, estrogen acts on the central nervous system to regulate the inflammatory process.1,8 Inflammation of the synovium may lead to inadequate lubrication and nourishment of the cartilage and disc.2 ERα has a pro-inflammatory effect on monocytes as opposed to ERβ, which has anti-inflammatory effects.1 Evidence suggests estrogen is involved in the inflammatory process within the TMJ, particularly in the modification of pain signals.13
Known as single nucleotide polymorphisms, genetic variations on the ERβ increase the risk for TMDs by altering chondrocyte synthesis and releasing interleukin 1 (IL1), interleukin 6 (IL6), and tumor necrosis factor-a (TNF-α).8,9 Therefore, polymorphism offers insight into why estrogen levels affect women differently in terms of TMDs and chronic joint pain. Overall, further research is needed to better understand estrogen’s role in the process of cytokines, particularly IL6, which may exacerbate the inflammation process, and the specific estrogen-induced responses on TMD-related pain.
THE CONNECTION
Bueno et al14 proposed that women, compared with men, are more predisposed to TMDs, which suggests that gender disparities may play a role in the pathophysiology of this condition. Researchers have found estrogen may influence pain receptors, which may highlight the differences between male-female TMD-related pain.14 Fluctuation of estrogen levels occur before puberty, during menstruation, and after menopause, all of which may impact a woman’s pain threshold.1 Subsequently, pain onset occurs after puberty and peaks in reproductive years, but tapers after menopause.15 Evidence suggests that estrogen inhibits inflammatory processes associated with TMD-related pain.1 During periods of high estrogen concentration levels, the inflammatory process is inhibited and TMD-related pain decreases.2 Contrastingly, during the menstrual cycle, post-menopause, and following an ovariectomy, low levels of estrogen occur; consequently, lower levels of estrogen induce pro-inflammatory effects within the TMJ, resulting in higher pain levels.1
A preliminary study by Landi et al16 investigated the relationship between estrogen and TMDs. Results showed significantly higher serum estrogen levels in patients affected by TMDs, compared to their counterparts. Increased serum levels were found in both men (p < 0.01) and in the luteal phase of the menstrual cycle in women (p < 0.05). Evidence suggests that high serum estrogen levels might play an important role in the physiopathology of TMDs.16
Conversely, other studies report conflicting results which put into question the extent of correlation between estrogen and TMD.17,18 For example, in 2005, LeResche et al17 explored the effect of hormonal fluctuations in relation to musculoskeletal pain in the temporomandibular region. Researchers compared pain, depression, and somatic symptoms differences between women with musculoskeletal orofacial pain (n = 19) and pain-free women (n = 16) during their pregnancy and 1 year post-partum. The baseline was established at the first trimester with the use of the RDC/TMD. Study participants completed a self-reported questionnaire and provided a sample of unstimulated saliva at the first, second, and third trimester, and 1 year post-partum. Investigators found that both depression and somatic symptoms, excluding pain, changed significantly over time (P ≤ 0.05). Conversely, when assessing women with musculoskeletal orofacial pain and their respective pain-free counterparts, researchers found similar, but statistically insignificant changes (p > 0.05). Nevertheless, women with musculoskeletal orofacial pain demonstrated decreased levels of both depression and somatic symptoms 1 year post-partum compared to throughout their pregnancy (p ≤ 0.05).
In 2018, Ivković et al18 studied the fluctuation of estrogen and its effect on TMD during normal menstrual cycling, pregnancy, and surgically induced menopause. Researchers found that pregnant participants had the lowest pain intensity at the 36th week, while women in surgical menopause had significantly higher pain intensity. Even though competing evidence continues to provide an unclear resolve on the potential effects of estrogen levels on TMD-related pain, in this study, high levels of estrogen appear to lower TMD-related pain.
CLINICAL IMPLICATIONS
Treatment modalities for patients experiencing TMD-related pain include self-regulated strategies, anti-inflammatory medications, hormone therapy, botulinum toxin injections, acupuncture, occlusal splint therapy, and surgical interventions used to treat both peripheral nervous system and central nervous system components of TMD-related pain. Relaxation and biofeedback therapies are commonly used self-regulated strategies for patients with TMD-related pain. However, these therapies are still considered controversial. Multiple drugs may also be used for the management of TMD pain, such as nonsteroidal anti-inflammatory drugs (NSAIDs), corticosteroids, analgesics, muscle relaxants, anxiolytics, opiates, tricyclic antidepressants, gabapentin, and lidocaine patches. The risk of polypharmacy and/or patient dependency, however, must be considered. The use of NSAIDs, often used as a long-term treatment option, only alleviate the symptoms rather than effectively treating the TMD. Topical ointments or creams may be used as an alternative to oral medications that may cause adverse systemic effects.5
Although TMD pain varies throughout the menstrual cycle, it is the highest immediately before menses, due to low estrogen levels.19 Low levels of estrogen are also present in post-menopausal women, which coincides with an increase in TMD-related pain.1 In 2018, Farzin et al20 found that the prevalence and severity of TMD-related pain in menopausal women was higher compared to nonmenopausal women. Specifically, pain in the TMJ and pain during mandibular movements were more common for menopausal women. Research suggests women with lower estrogen levels benefit from hormone therapy including the use of continuous oral contraception therapy (COCT).19 However, not all patients with TMD-related pain benefit from this therapy. COCT is more likely to be effective for women experiencing biological pain rather than mechanical pain, such as clenching and bruxism.19
The use of hormone replacement therapy (HRT) in menopausal women and its relationship on TMD-related care has previously been studied. In 1997, LeResche et al21 studied the prevalence of TMD-related pain among women who used exogenous forms of hormone replacement. They found that increases in the dosages of estrogen positively correlated with the number of women seeking referral for TMD-related care. Results suggested that women using a 185 mg annual cumulative estrogen dosage exhibited a 36% increased probability for receiving a referral for TMD-related care. Interestingly, the probability for receiving a referral for TMD-related care escalated to 84% likelihood among women using a 220 mg annual cumulative estrogen dosage.
Conversely, some recent studies suggest the opposite effect.22,23 In 2008, Nekora-Azak et al22 compared the presence of TMD-related signs and symptoms among women using and not using HRT. They found no significant differences between both groups, suggesting there is limited evidence to support an increased prevalence of TMD-related pain in post-menopausal women alone. In 2016, Lora et al23 retrospectively examined the experience of TMD-related pain among post-menopausal women, including those who underwent and did not undergo HRT. Lora et al23 again found that there was no significant difference between the use of HRT and TMD-related pain (p < 0.01).
More recent research, such as Stinson et al,24 support that future studies should center on the methods of hormone replacement administration. They suggested that differences in results, particularly when it comes to HRT, could be traceable to a change in drug concentration. Research suggests that a rise in estrogen can lead to protective effects and a decrease in estrogen seems to exacerbate the pain responses.24 Further study is needed on HRT and TMD in order to better understand this complex relationship.
The use of botulinum toxin-a, a biological exotoxin produced by Clostridium botulinum, has been suggested as a viable treatment for myogenous TMDs.25,26 Research suggests that regardless of type, number of injections, and dosage, botulinum toxin-a appears to be effective for TMJ-related muscle disorders.26 In 2019, Sipahi-Calis et al27 studied the efficacy of botulinum toxin injections for the treatment of TMD-related pain. Results show that 36% (n = 25) of study participants found beneficial effects, and no side effects, at the 6-month follow-up. Even though these results look encouraging, it also demonstrates that this treatment may not be effective for everyone.
Splint therapy and acupuncture are comparable in providing pain relief. These two therapies are more beneficial for myogenous TMDs affecting the muscles, rather than arthogenous TMDs that affect the joints.28 Splint therapy is also frequently used with TMDs associated with clenching or bruxism, to help correct occlusion and biting forces.5 Acupuncture can also serve as an alternative to managing chronic pain frequently associated with TMD. Acupuncture relieves pain by using needles at the appropriate acupuncture points. The therapeutic effects of acupuncture, such as needle placement and how deep the needle is inserted, can vary among therapists, and the probability of success may not be the same for all patients with TMDs.28
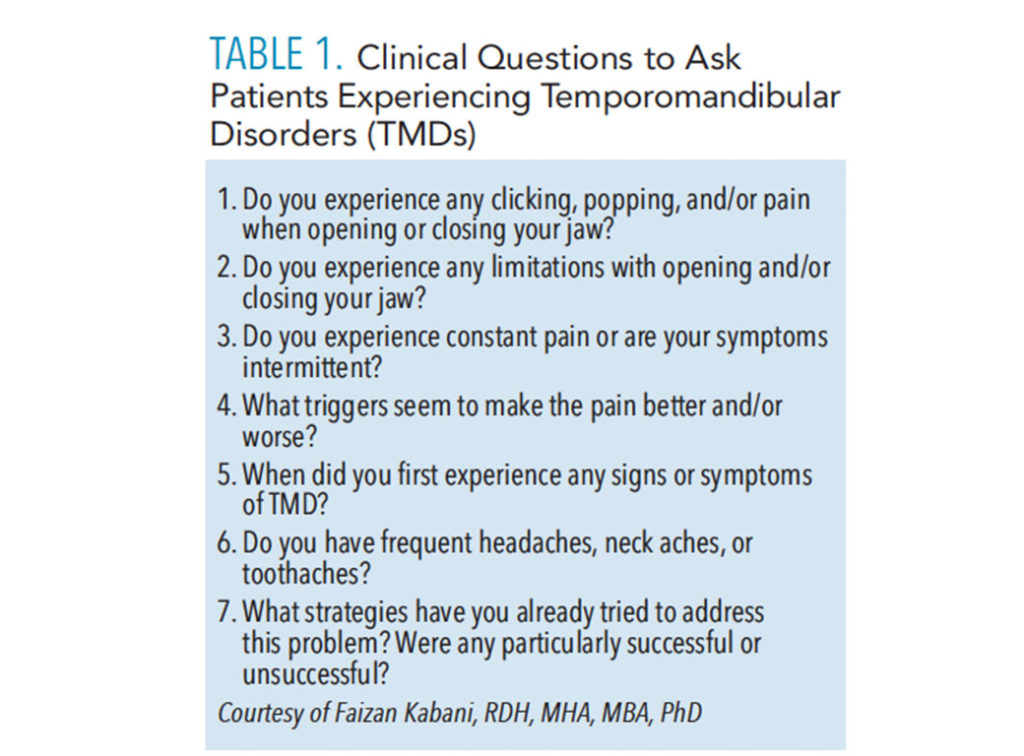
The efficacy of all therapeutic options for patients with TMDs is subjective and should be recommended on a case-by-case basis.28 Advanced surgical interventions, such as arthrocentesis and arthroscopy, modified condylotomy, and open-joint surgery, are available but should only be considered after conservative measures are deemed ineffective. Conservative forms of medical management and rehabilitation are generally recommended over surgical interventions.5 Table 1 lists clinical questions oral health professionals can ask patients regarding the impact of TMDs on quality of life.
![]() CONCLUSION
CONCLUSION
Despite scientific advancements, TMDs continue to be complex conditions affecting patients worldwide.1,12,19 TMDs have the potential to complicate diagnosis and treatment planning. Hormonal fluctuations play a significant role in reducing TMD-related pain. Despite mixed evidence on the potential role of estrogen receptors on TMD-related pain, oral health professionals should continue to evaluate patients with TMDs systemically for other potential contributing factors as part of a comprehensive care strategy.
To date, there is no universally agreed upon gold standard intervention for treating patients with TMD-related pain. A variety of conservative and surgical treatment modalities exist; however, evidence-based oral health professionals are advised to provide treatment based on the unique needs of each individual patient.5 Current therapies for managing TMD-related pain focuses on alleviating symptoms, rather than addressing the root causes of TMDs.5,27,28 Future research should investigate the origin of TMD-related pain and determine the role estrogen receptors plays in targeting inflammation, including how estrogen may be integrated to alleviate pain associated with TMDs.
Acknowledgements: The authors would like to acknowledge Alfredo Rodriguez, RDH, BSDH, and Amy Heim, RDH, BSDH, for their assistance with this manuscript.
REFERENCES
- Ribeiro-Dasilva MC, Fillingim RB, Wallet SM. Estrogen-induced monocytic response correlates with temporomandibular disorder pain: a case control study. J Dent Res. 2017;96:285–291.
- Furquim BD, Flamengui LM, Conti PC. TMD and chronic pain: a current view. Dental Press J Orthod. 2015;20:127–133.
- National Institute of Dental and Craniofacial Research. TMJ (Temporomandibular Joint and Muscle Disorders). Available at: nidcr.nih.gov/health-info/tmj. Accessed December 10, 2019.
- Chisnoiu AM, Picos AM, Popa S, et al. Factors involved in the etiology of temporomandibular disorders—a literature review. Clujul Medical. 2015;88:473–476.
- Gil-Martínez A, Paris-Alemany A, López-de-Uralde-Villanueva I, et al. Management of pain in patients with temporomandibular disorder (TMD): challenges and solutions. J Pain Res. 2018;11:571–587.
- Schiffman E, Ohrbach R, Truelove E, et al. Diagnostic criteria for temporomandibular disorders (DC/TMD) for clinical and research applications: recommendations of the international RDC/TMD consortium network and orofacial pain special interest group. J Oral Facial Pain H. 2014;28:6–27.
- Barros VM, Seraidarian PI, Cortes MI, et al. The impact of orofacial pain on the quality of life of patients with temporomandibular disorder. J Orofac Pain. 2009;23:28–37.
- Ribeiro-Dasilva MC, Peres Line SR, Leme Godoy Dos Santos MC, et al. Estrogen receptor-α polymorphisms and predisposition to TMJ disorder. J Pain. 2009;10:52–-533.
- Quinelato V, Bonato LL, Vleira AR, et al. Association between polymorphisms in the genes of estrogen receptors and the presence of temporomandibular disorders and chronic arthralgia. J Oral Maxilof Surg. 2018;76:31:e1–e9.
- Bi RY, Meng Z, Zhang P, et al. Estradiol upregulates voltage-gated sodium channel 1.7 in trigeminal ganglion contributing to hyperalgesia of inflamed TMJ. PLoS One. 2017;12:1–16.
- Nicotra L, Loram L, Watkins L, et al. Toll-like receptors in chronic pain. Expl Neurol. 2012;234:316–329.
- Deshmane SL, Kremlev S, Amini S, Sawaya BE. Monocyte chemoattractant protein-1 (MCP-1): an overview. J Interferon Cytokine Res. 2009;29:313–326.
- Berger M, Szalewski L, Bakalczuk M, et al. Association between estrogen levels and temporomandibular disorders: a systematic literature review. Prz Menopauzalny. 2015;14:260–270.
- Bueno CH, Pereira DD, Pattussi MP, et al. Gender differences in temporomandibular disorders in adult populational studies: a systematic review and meta‐analysis. J Oral Rehabil. 2018;45:720–722.
- Warren MP, Fried JL. Temporomandibular disorders and hormones in women. Cells Tissues Organs. 2001;169:187–192.
- Landi N, Lombardi I, Manfredini D, et al. Sexual hormone serum levels and temporomandibular disorders. A preliminary study. Gynecol Endocrinol. 2005;20:99–103.
- LeResche L, Sherman JJ, Huggins K, et al. Musculoskeletal orofacial pain and other signs and symptoms of temporo-mandibular disorders during pregnancy: a prospective study. J Orofac Pain. 2005;19:193–201.
- Ivković N, Racic M, Lecic R, et al. Relationship between symptoms of temporomandibular disorders and estrogen levels in women with different menstrual status. J Orofac Pain. 2018;32:151–158.
- Turner JA, Mancl L, Huggins KH, et al. Targeting temporomandibular disorder pain treatment to hormonal fluctuations: a randomized clinical trial. J Pain. 2011;152:2074–2084.
- Farzin M, Taghva M, Bambooie M. Comparison of temporomandibular disorders between menopausal and non-menopausal women. J Korean Assoc Oral Maxillofac Surg. 2018;44:232–236.
- LeResche L, Saunders K, Von-Korff MR, et al. Use of exogenous hormones and risk of temporomandibular disorder pain. Pain. 1997;69:153–160.
- Nekora-Azak A, Evlioglu G, Ceyhan A, et al. Estrogen replacement therapy among post-menopausal women and its effects on signs and symptoms of temporomandibular disorders. Cranio. 2014;26:211–215.
- Lora VR, Canales-Gde L, Goncalves LM, et al. Prevalence of temporomandibular disorders in postmenopausal women and relationship with pain and HRT. Braz Oral Res. 2016;30:100.
- Stinson C, Beliinger LL, Puri J, et al. Estrogenic effects on temporomandibular disorder and pain. J Appl Biobehav Res. 2019;24:12164.
- Bogucki ZA, Kownacka M. Clinical aspects of the use of botulinum toxin type a in the treatment of dysfunction of the masticatory system. Adv Clin Exp Med. 2016;25:569–573.
- Ataran R, Bahramian A, Jamali Z, et al. The role of botulinum toxin a in treatment of temporomandibular joint disorders: a review. J Dent (Shiraz). 2017;18:157–164.
- Sipahi-Calis A, Colakoglu Z, Gunbay S. The use of botulinum toxin-a in the treatment of muscular temporomandibular joint disorders. J Stomatol Oral Maxillofac Surg. 2019;120:322–325.
- Wu JY, Zhang C, Xu YP, et al. Acupuncture therapy in the management of the clinical outcomes for temporomandibular disorders: a prisma-compliant meta-analysis. Medicine (Baltimore). 2017;96:60–64.
From Dimensions of Dental Hygiene. January 2020;18(1):34–36,39.