
Ergonomic Best Practices
A variety of interventions is available to help clinicians reduce the risk of injury and practice more efficiently.
Long days, awkward and prolonged static posture, working stations that are difficult to negotiate, and instrument designs that lead to hand fatigue all affect clinicians’ performance, working behavior, and quality of life.1,2 As a result, they can also impact the quality of patient care and health outcomes. For example, dental hygienists who experience
discomfort from sitting in a poorly designed operator chair will not be able to treat as many patients as clinicians who are seated comfortably. Unsupported repetitive hand-arm-shoulder movements and improperly designed instruments can also compromise fine motor dexterity and tactile sensitivity.
Sartorio et al indicated that the incidence of work-related musculoskeletal disorders among dental professionals is reaching 96%.3 These occupational complications are related to ergonomics—the science of designing jobs, equipment, and the workplace environment to fit workers.2 Specific risk factors for work-related injuries defined by the Occupational Safety and Health Administration (OSHA) include: repetitive motion or awkward posture for more than 2 hours at a time, unassisted frequent manual handling (eg, scaling an area using the same strokes), and unassisted forced manual handling (eg, heavy calculus removal using hand-activated instruments).4
Dental hygienists experience these work-related risk factors on a daily basis.4 In order to prevent injury, clinicians should consider the many product solutions currently available to improve the ergonomics of practice. Decisions about which products will be most helpful need to incorporate personal considerations such as height, weight, and health conditions.
STOOLS
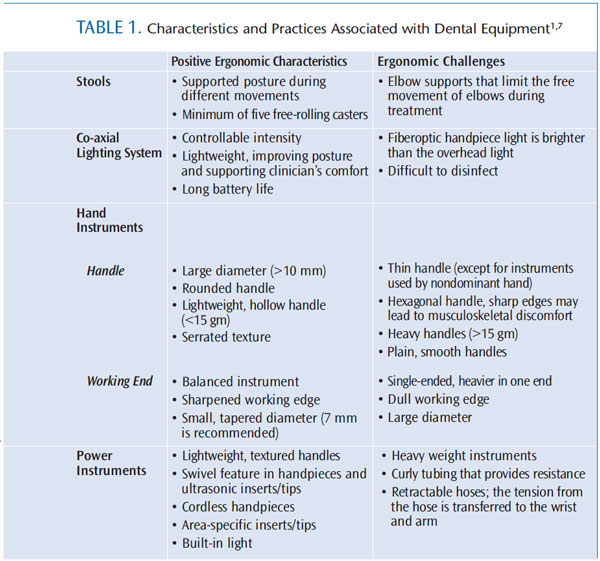
Some clinicians prefer to purchase their own stool to prevent musculoskeletal complications.5 The stool should support thighs, arms, legs, and back, as well as proper posture, circulation, and respiration. The clinician’s weight should be evenly distributed on the stool, and the need to twist or bend should be minimized.5,6 The ergonomic factors related to stools appear in Table 1.
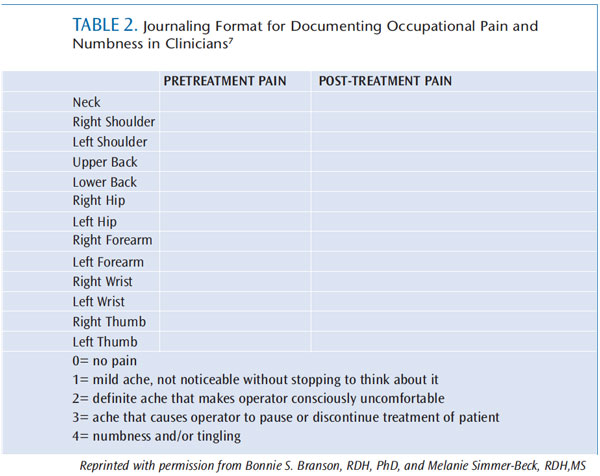
Before choosing a stool, dental hygienists should assess their posture using a tool, such as Branson’s Posture Assessment Instrument (BPAI).7,8 The BPAI uses validated parameters of posture, observed by an evaluator for 5-minute periods throughout a full workday. At the end of the day, observations are translated to numeric values and compared to a standard to evaluate range of posture and changes in posture over time. Changes can be evaluated according to the degree of pain felt in specific areas of the upper body (Table 2).
In addition to basic recommendations, such as standing during some procedures or stretching exercises, Cherniack et al and Valachi suggest using different stools during the working day to prevent prolonged static posture and vary body muscle function.9–12 Others advocate using a stool with an armrest to distribute lumbar pressure more evenly between the back and arms.13 However, using an armrest during patient care can stress the shoulders if the stool is not properly adjusted.13
LED DENTAL LIGHTING SYSTEMS
An ideal light source produces even, shadow-free illumination that shows accurate colors of the oral cavity.1 A light that is too bright or too dim can lead to eyestrain, reduced vision, headaches, inaccurate dental hygiene diagnosis, substandard care, and tissue trauma.1,5,8
When compared to traditional halogen lighting, the increasing popularity of light emitting diodes (LEDs) is attributed to their long life (20 years in some cases), low operating costs, and minimal heat generation.14 While most cool LEDs have a very strong blue light that will cure composite, a filter can be used to prevent premature curing of materials. The co-axial headlight design found in some dental lights provides a light source parallel to the operator’s line of vision, reduces shadows from hands and instruments, and is portable, lightweight, and easy to control.8,14 Table 1 provides additional details.
HAND INSTRUMENTS
The absence of industry standards for ideal design, weight, and shape of hand instruments has led to the availability of a wide range of commercial options.4 For example, a specific instrument design can be found with different handle sizes, diameters, and surface textures. Some instruments are ergonomically adjusted for control, adaptation, and degree and distance of applied pressure15 (eg, instrument handles with gripping pads). Instruments held by the nondominant hand require ergonomic designs because the hand stays steady for extended periods.2 Therefore, dental hygienists need to be selective in purchasing ergonomically sound instruments (Table 1).
MECHANIZED INSTRUMENTS
Mechanized instruments include high- and low-speed handpieces, lasers, and ultrasonic and sonic scaling devices (Table 1).15 Instruments should be as light as possible and balanced. Handpieces and ultrasonic inserts/tips (UITs) with swiveling features support movement and rotation of the handle during treatment.6 The use of lighted handpieces and UITs may facilitate vision.1 Using “cruise control” foot switches that continue working with a single touch, instead of requiring constant contact with the clinician’s foot, prevents prolonged static leg posture.16 Also, the use of foot- or voice-activated devices supports an ergonomic environment and promotes accurate documentation, such as voice- and foot controlled periodontal charting systems.17
MAGNIFICATION DEVICES
Magnification in dental hygiene practice can improve quality of assessment, diagnosis, treatment, and clinician posture.4,18 Magnification systems include dental endoscopes, microscopes, and dental loupes. Dental endoscopy gives the clinician direct, real-time visualization and magnification of the subgingival root surface to detect calculus and assess periodontal status. Using the endoscope during dental hygiene treatment can improve calculus detection, scaling, and the determination of clinical and therapeutic endpoints in the process of care, when compared to relying on tactile sensitivity alone.19
Loupes are preferred among dental hygienists, and they can be instrumental in improving posture.19 Using the wrong type of loupes or improperly adjusted loupes, however, can have significant musculoskeletal consequences and lead to eye strain. Generally, loupes should be lightweight and comfortable to wear. Most intraoral dental hygiene procedures require a magnification strength of no greater than 2.5x.18–20
Working distance, depth of field, and declination angle should also be considered. Working distance is the measurement from the eyes to the worksite while the operator is in an ergonomically ideal position. The best working distance is typically the midpoint of the loupes’ working range.20 Depth of field is the loupes’ ability to focus both near and far without necessitating head movement. With higher levels of magnification, there is less depth of field.21 The declination angle refers to the angle between the neutral eye position and the line of sight to the work area.18–20 Too much of an angle will lead to eyestrain as the dental hygienist is forced to look down, while too small of an angle leads to head and neck flexion as the dental hygienist strains forward.20
Three types of loupes are used by dental hygienists: fixed through the lens, which are mounted to eyeglass lenses; front-lens mounted (FLM) without vertical adjustment, which provide adjustment to the interpupillary distance between users but do not allow adjustment of the declination angle; and FLM with vertical adjustment, which allow adjustment to the declination angle.19,20 Like any innovation, a learning curve is expected while dental hygienists adjust to using loupes.4,18 Keeping a personal assessment journal on how the loupes feel and affect practice supports a healthy working style (Table 3).7
GLOVES
Surgical glove–induced injury is a type of musculoskeletal disorder caused by wearing poor-fitting gloves (eg, too tight or too loose).21 Gloves that are too loose decrease instrument control, leading to deficient treatment quality and possible patient tissue trauma.23 In contrast, tight gloves impede blood circulation and cause muscle fatigue and discomfort.22 Ambidextrous gloves are designed for short medical examinations, not for long dental hygiene appointments.10 Thus, proper glove size supports musculoskeletal health.1 Kreismann recommends textured gloves to enhance instrument grasp and reduce grasping pressure in the clinician.22 Right and left-handed gloves can decrease muscle effort due to their special design, and well-fitted palm and wrist areas prevent tightness during treatment.23
ENVIRONMENT
Working environment temperature (eg, room, air, and water temperature) influences muscle tension and pain.22 Exposing fingers to low temperature can affect dexterity and grip strength.1 No standards exist for safe finger temperatures, but recommendations suggest that the operator’s fingers should be kept above 25° C or 77° F.1 There are no published recommendations on the ideal room temperature in the dental setting. However, clinicians should be comfortable.1,22 The treatment area should be designed so dental hygienists can move and reach the instruments, equipment, and supplies without bending, twisting, or rotating the torso during patient’s care.13 Dental hygienists should be able to maintain the neutral position and move freely while practicing (eg, left-handed hygienists should find enough space to maintain 1 o’clock, 3 o’clock, and 5 o’clock positions).1,13
Rarely used equipment should be kept away from working areas.24 Frequently used equipment (eg, hand instruments and ultrasonic scalers) should be within 14 inches to 16 inches from the elbow.24 To determine proper placement for reachability, the clinician can sweep the forearm in a horizontal arc, keeping the elbow relaxed at the side. Less-used equipment should be within 25 inches from the shoulder when the elbow is extended.24 Organizing the working area depends on the operator’s personal preferences, ergonomic recommendations, and available workspace.
.jpg)
CONCLUSION
Maintaining a healthy working style is multidimensional. To maintain a long career and a healthy lifestyle, dental hygienists should create an ergonomically healthy practice, participate in equipment and product purchasing decisions, and practice a healthy lifestyle (eg, exercise). Dental hygienists should collaborate with colleagues to create and maintain a safe and healthy working environment. Alternating between less challenging and challenging cases is encouraged (ie, not scheduling two difficult patients in succession).1,13 Also, paying attention to some minor modifications can maintain an ergonomic dental hygiene practice (eg, using two finger rests and/or fourth and fifth fingers as a fulcrum instead of only the ring finger may decrease thumb and pinch forces and pressure during instrumentation).25 Dental hygienists should be discriminating in choosing ergonomically designed instruments and equipment and supplies. In summary, ergonomic principles can guide dental hygienists to work smarter rather than harder by choosing evidence-based instruments, equipment, and products to fit the needs, rather than requiring dental hygienists to fit the working environment.13
REFERENCES
- Sachdeva J, Gupta A. Ergonomics principles in dental setting. Guident.2012;5(3):81–84.
- Haddad O, Sanjari MA, Amirfazli A, Narimani R, Parnianpour M. Trapeziusmuscle activity in using ordinary and ergonomically designed dentistry chairs.Int J Occup Environ Med. 2012;3:76–83.
- Sartorio F, Vercelli S, Ferriero G, D’Angelo F, Migliario M, Franchignoni M.Work-related musculoskeletal diseases in dental professionals. 1. Prevalenceand risk factors. G Ital Med Lav Ergon. 2005;27:165–169.
- Osuna T. Ergonomics: investing in yourself. J Calif Dent Hyg Assoc.2006;21(2):18–28.
- Wilkins EM. Clinical Practice of the Dental Hygienist. 11th ed. Philadelphia:Lippincott Williams & Wilkins; 2012:91–92.
- Jordre BD, Bly J. Protect your musculoskeletal health. Dimensions of DentalHygiene. 2012;10(1):30–34.
- Branson B, Simmer-Beck M. Personal assessment. Dimensions of DentalHygiene. 2009;7(4):20–23.
- Brame JL. Seating, positioning, and lighting. Dimensions of Dental Hygiene.2008;6(9):36–37.
- Cherniack MG, Dussetschleger J, Bjor B. Musculoskeletal disease anddisability in dentists. Work. 2010,35:411–418.
- Valachi B. Creating the ‘ergonomic’ operatory: evidence-based strategiesfor dental hygienists and those who travel. Access. 2012;26(6):14–18.
- Kott K, McCombs GB. Avoid low back pain. Dimensions of Dental Hygiene.2011;9(1):36–41.
- Valachi B. Move it: physical movement is key to preventingmusculoskeletal problems. Dental Practice Report. 2006;14:52–54.
- Gupta S. Ergonomic applications to dental practice. Indian J Dent Res.2011;22:816–822.
- Walsh LJ. LED operating lights in dental practice. Australasian DentalPractice. 2009:48–54.
- Marsh L. Practicing ergonomically correct dental hygiene. Dimensions ofDental Hygiene. 2009;7(1):22–23.
- Low SB. The evolution of ultrasonic therapy. Dimensions of Dental Hygiene.2004;2(9):18–23.
- Calley KH, Hodges KO. Automate your probing process. Dimensions ofDental Hygiene. 2011;9(2):44–47.
- Shah MA, Pellegrini J. Magnification basics. Dimensions of Dental Hygiene.2010;8(11):36–38.
- Michaelides P, Stambaugh R. Zooming in on magnification. Dimensions ofDental Hygiene. 2007;5(4):16–21.
- Branson B, Simmer-Beck M. Visual acuity without injury. Dimensions ofDental Hygiene. 2009;7(9):46–49.
- Nield-Gehrig JS. Fundamentals of Periodontal Instrumentation andAdvanced Root Instrumentation. 7th ed. Philadelphia: Lippincott Williams &Wilkins; 2012:80.
- Kreismann J. The struggle for musculoskeletal health. Dimensions ofDental Hygiene. 2007;5(9):24–25.
- Stone R. The winning hand. Mentor. 2012;3(9):28–31.
- Solomon S. Healthy dental design: a thorough checklist. Ontario Dentist.2009;86(2):22–26.
- Dong H, Barr A, Loomer P, LaRoche C, Young E, Rempel D. The effects ofperiodontal instrument handle design on hand muscle load and pinch force.J sAm Dent Assoc. 2006;137:1123–1130.
From Dimensions of Dental Hygiene. April 2013; 11(4): 30–34

