WAVEBREAKMEDIA LTD/GETTY IMAGES PLUS
WAVEBREAKMEDIA LTD/GETTY IMAGES PLUS
Ensuring Medication Safety in the Dental Setting
Dental teams can use these strategies to encourage medication adherence among patients and avoid possible adverse drug interactions.
This course was published in the December 2019 issue and expires December 2022. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Explain why a comprehensive medical and pharmacological history is an integral part of safe and effective dental treatment.
- Describe how clinicians can help manage medications to avoid possible adverse drug interactions.
- Discuss possible clinical considerations for generic drugs, and the management of patients with hypertension and/or uncontrolled diabetes.
A comprehensive medical and pharmacological history precedes any oral assessment and is an integral part of safe and effective dental treatment. It is common practice to have patients record medications and medical conditions, and for clinicians to review for red flags before providing dental assessments and services. However, the complexities of medical conditions, possible drug interactions, medication adherence, and implications for dental treatment suggest a more in-depth dialogue is required. Discrepancies in the dental record with regard to medications are not uncommon,1 and patients may not always provide a complete and accurate list of drugs, including over-the-counter (OTC) medications and herbal supplements.2
Efficient and effective care requires oral health professionals to have a structured plan to address pharmacological risks and benefits, including disclosure, and assess the patient’s knowledge and compliance. More nuanced concerns—such as generic bioequivalence, managing drug interactions, and special considerations for medically complex patients and older adults—must also be considered. Seeking additional consultation from the primary care or specialist physician and pharmacist may be indicated in complex cases. Interprofessional collaboration allows the dental team to have an impact on health behaviors, as well as help prevent and control systemic diseases with high morbidity and mortality, such as cardiovascular disease (CVD) and diabetes mellitus.3,4
PATIENT DISCLOSURE AND MEDICATION ADHERENCE
Patient disclosure begins with a dental-medical health history that should contain adequate detail and prompts for patients to list medical conditions, prescribed medications, OTC agents and supplements, as well as dosages, time of day, and frequency of administration. Appointment reminders, especially for new patients, should include a request for these particulars so patients are prepared to provide details and understand the importance of complete information.
Medication adherence can significantly affect outcomes, including decreased morbidity and mortality in chronic diseases.5,6 While drugs for hypertension and high cholesterol have high nonadherence rates, studies have shown interventions to improve adherence—for instance, by simplifying a medication administration schedule—may result in increased adherence and improved short-term outcomes.7,8 Additionally, an objective, comprehensive review by the dental professional, along with appropriate referrals, may assist the patient in assessing risks for nonadherence and possible adverse effects.
ADVERSE DRUG EVENTS AND DRUG INTERACTIONS
Adverse drug events include medication errors, drug reactions/interactions, hypersensitivity, and overdoses, and account for more than 2 million hospital visits, prolonged hospital stays, and more than 3 million outpatient visits annually.9 Recently, there has been attention to prevention of adverse drug events in outpatient settings, such as the dental office and the use of computerized prescribing and electronic databases when communicating risks to patients and making treatment decisions.9,10
Taken together, two or more drugs (prescribed or OTC) can interact in a predictable manner when the interaction is known—or an unexpected manner, when the relationship between the drugs is less known. Patients may also exhibit genetic polymorphisms, resulting in variable drug metabolism. In addition, drugs may interact with food, vitamins/minerals, and herbal supplements.10,11 There are many complex underlying mechanisms of the interaction of two or more drugs, including alterations in pharmacokinetics and pharmacodynamics.11,12
With 82% of Americans taking one medication and 29% taking five or more (ie, polypharmacy), along with differences in individual drug responses, there is an alarming low rate of only 25% to 60% effectiveness of many major drugs, as well as more than 2 million adverse drug events reported in the United States annually,9,12 resulting in approximately 100,000 deaths.9 These are possibly preventable by an alert health care provider and a careful review of the medication record. The total number of medications is not necessarily a problem when they are supported by evidence-based medicine, optimized for a specific patient’s needs, and outcomes are monitored closely. However, polypharmacy can have a negative impact when multiple medications are prescribed inappropriately.13
OLDER ADULTS: A SPECIAL POPULATION
Due to polypharmaceutical concerns, older adults with multiple systemic conditions should be assessed especially carefully. Older adults with decreased cognitive function may struggle to comply with their medication regimens. A memory decline typically coincides with a decline in oral health; however, detection of cognitive impairment can be difficult to notice when dental teams only see patients for a limited time.
Several polypharmacy reduction strategies can be implemented, including using the Beers criteria,14 an explicit list of potentially inappropriate medications that should be avoided or used with caution in older adults. There is also an increased risk of exacerbating geriatric syndromes, such as cognitive impairment, malnutrition, and incontinence.15 The Beers criteria14 help inform clinicians about medications that may cause adverse reactions due to the physiological changes of aging. Although the list is not prohibitive, it does weigh the risks and benefits for many commonly prescribed medications, with the goal of reducing polypharmacy in the geriatric population. The criteria also emphasize a team approach and the use of non-pharmacological solutions.14
Several medications in the Beers criteria would not normally be prescribed by a dentist, yet may affect oral health, such as anticholinergics that may cause xerostomia. Medications on the list within the prescribing scope of dentistry include nonsteroidal anti-inflammatory drugs (NSAIDs) that can increase the risk of gastrointestinal bleeding, and benzodiazepines, prescribed for sedation, which can cause cognitive impairment, delirium, and falls.16
A difficult question regarding medication compliance is when to switch from patient self-management to a caregiver’s responsibility—especially when a patient takes a medication with a narrow therapeutic window. Other strategies for improving compliance in patients with dementia include prescribing as few medications as possible, and developing an easier-to-follow dosing schedule. Pill packs, medication organizers, electronic reminders, and even telemonitoring can be helpful for patients with dementia, but it is equally important to assess the patient’s ability to use these devices properly before implementing them.17
GENERIC DRUGS: CLINICAL EQUIVALENCY
While generic drugs represent 84% of the total pharmaceutical volume in the US,18 their quality and effectiveness have been called into question.19,20 Generic drugs typically benefit consumers and third-party payers because of their comparatively lower price.18,21 Substituting these drugs for brand-name medications is based on the assumption of clinical equivalency, which, in turn, is based on the bioequivalence measure.19 The US Food and Drug Administration compares pharmacokinetics of the generic drugs to the brand-name counterparts, and allows for 20% variability in some pharmacokinetic parameters.19 It should be stressed, however, that bioequivalence studies involve a small number of healthy volunteers, evaluate only the drug’s pharmacokinetics, and do not compare the clinical effectiveness or safety/adverse affects in individuals with a particular disease. In essence, bioequivalence does not necessarily equal clinical equivalence.18 Moreover, a recent systematic review of published bioequivalence trials found the quality of reporting to be poor.21 These comparison studies matter particularly for drugs with narrow therapeutic indices, such as warfarin, because small changes in systemic concentration of the generic drug can lead to significant variation in its performance, resulting in insufficient efficacy or toxicity.21

For dental teams, the clinical effectiveness of agents such as antihypertensive19 and antidiabetic medications may present the most concern. Clinicians may raise the patient’s awareness about the drug’s efficacy based on the patient’s report and blood pressure or glucose monitoring. Individuals should be referred to the prescribing physician if the oral health professional suspects the medication is inadequate for maintaining the patient’s condition.
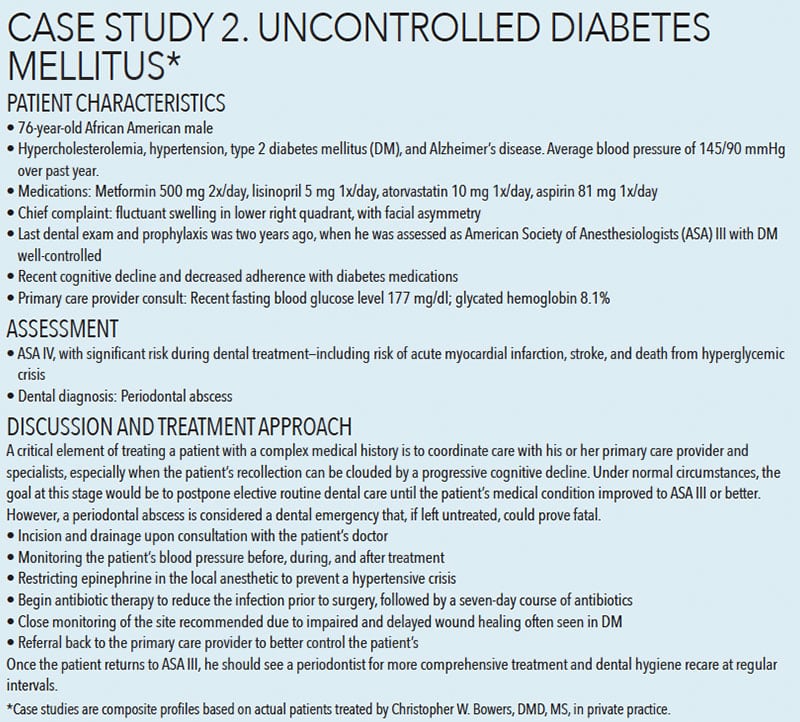
COMPLEXITIES OF HYPERTENSION
Revised in 2017, blood pressure guidelines22 now set a lower limit for high blood pressure (Table 1). This was done in recognition of the risk for cardiovascular complications at lower numbers, and to stress the need for early intervention via lifestyle changes and/or the use of antihypertensive medication. According to the new numbers, about half of Americans have hypertension; however, there should only be a small increase in patients requiring antihypertensive therapies, as most cases of Stage 1 hypertension can be managed with lifestyle modifications.22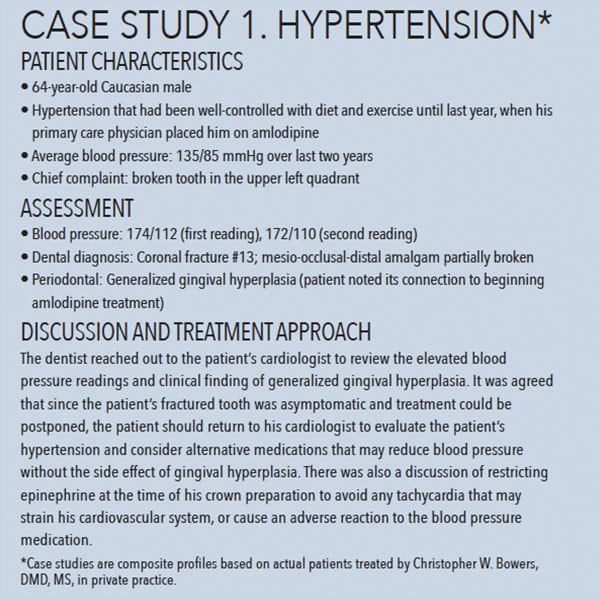
As a complex disease with many risk factors and comorbidities, managing hypertension often requires multiple medications from different pharmacological categories. Unfortunately, multidrug therapies can lead to low adherence,8 which, in turn, can contribute to persistent hypertension due to development of drug resistance. It is also associated with occasional toxicity, which can cause discontinuation of treatment.8 It is important to identify the reasons for poor adherence and offer appropriate solutions. Even simple strategies, such as moving dosing time from evening to morning (when not contraindicated by drug interactions), can improve adherence.7 Provider-patient communication is an important factor, and dental teams can help improve compliance by assessing adherence during medical history intake/update, stressing its importance, and referring patients for specialist evaluation when necessary (Case Study 1).
MANAGING DIABETES MELLITUS
Managing diabetes mellitus requires vigilance in the regulation of glucose homeostasis utilizing oral hypoglycemic agents, insulin, or both. Comprehensive diabetes care may involve other pharmacotherapies to minimize acute adverse events, such as hypoglycemia, and long-term risks, such as retinopathy, neuropathy, kidney disease, and cardiovascular complications.11 The dental team’s assessment and discussion of the patient’s glucose control and self-monitoring efforts should support these goals, thus ensuring safe treatment and preventing emergencies. Adherence to oral/parenteral diabetes medication protocols has been shown to vary greatly,23 and clinician-led interventions may have a lasting impact on compliance.7,24
Substantial evidence of a bidirectional relationship between diabetes and periodontal disease necessitates the evaluation of the patient’s medication adherence, including timing of administration and last meal, blood glucose levels, and most recent glycated hemoglobin (HbA1c) results. This may include point-of-care blood glucose and HbA1c screening where allowable, or referral for screening as warranted. The latter is important, as it is estimated that of the 30 million Americans living with diabetes, more than 7 million are undiagnosed, and diabetes remains the seventh leading cause of death in the US.25,26
Values for glycemic control for screening purposes and for patients with diagnosed diabetes are shown in Table 2 and Table 3. Importantly, the ideal values for any patient with diagnosed diabetes may be based on more individualized targets; this will reduce overtreatment and subsequent adverse events, most frequently hypoglycemia.24 Left untreated, hypoglycemia can lead to injury or death—and one of the risk factors is drug interactions. Of the drugs prescribed in the dental setting, antibiotics, such as clarithromycin, may alter the effect of oral antidiabetic agents, and most NSAIDs increase the risk of hypoglycemia, particularly with sulfonylureas. Drugs with major/moderate interaction may require medical consultation for a dose adjustment of the antidiabetic agent.

Uncontrolled diabetes increases risk for associated complications, including oral concerns, such as xerostomia, candidiasis, and periodontitis, with a positive correlation between incidence/severity and levels of hyperglycemia.27 Patients exhibiting periodontitis disproportionate to local factors, or progressing rapidly, may warrant chairside glucose/HbA1c screening and medical referral. The decision to treat includes assessing the risk for hyperglycemic crisis based on these values, history of glycemic control, and presenting oral disease, as severe infection is a precipitating factor.28
![Case Study 2]() CONCLUSION
CONCLUSION
A candid and comprehensive dialogue with patients during the medical and drug history intake opens the door to effective patient-provider communication, which facilitates evaluation of possible drug interactions, medication adherence, and possible implications for planned dental procedures. Efficacy of prescribed and OTC agents, including generics, can spell the difference between safe dental/dental hygiene treatment and, conversely, a range of negative outcomes, from rescheduling the patient to an emergency situation. While older adults and medically compromised individuals are especially at risk, every patient deserves a detailed evaluation of all findings. Dental professionals can offer a unique perspective to the interprofessional team on oral-systemic health in ensuring patient safety and positive treatment outcomes.
REFERENCES
- Choi HJ, Stewart AL, Tu C. Medication discrepancies in the dental record and impact of pharmacist-led intervention. Int Dent J. 2017;67:318–325.
- Johnson KL, Franco J, Harris-Vieyra LE. A survey of dental patient attitudes on the likelihood and perceived importance of disclosing daily medications. J Dent Educ. 2018;82:839–847.
- Heron M. Deaths: Leading Causes for 2016. Natl Vital Stat Rep. 2018:67:1–77.
- Wilder RS, Bell KP, Phillips C, Paquette DW, Offenbacher S. Dentists’ practice behaviors and perceived barriers regarding oral-systemic evidence: Implications for education. J Dent Educ. 2014;78:1252–1262.
- Schneider AP, Gaedke MÂ, Garcez A, Barcellos NT, Paniz VM. Effect of characteristics of pharmacotherapy on non-adherence in chronic cardiovascular disease: A systematic review and meta-analysis of observational studies. Int J Clin Pract. 2018;72(1).
- Hunt KJ, Gebregziabher M, Lynch CP, Echols C, Mauldin PD, Egede LE. Impact of diabetes control on mortality by race in a national cohort of veterans. Ann Epidemiol. 2013;23:74–79.
- Jung SH, Lee OS, Kim HS, et al. Medication adherence improvement by using Administration Timing Simplification Protocol (ATSP) in cardiovascular disease patients. J Atheroscler Thromb. 2017;24:841–852.
- Vrijens B, Antoniou S, Burnier M, de la Sierra A, Volpe M. Current situation of medication adherence in hypertension. Front Pharmacol. 2017;8:100.
- US Food and Drug Administration. Preventable Adverse Drug Reactions: A Focus on Drug Interactions. Available at: fda.gov/drugs/drug-interactions-labeling/preventable-adverse-drug-reactions-focus-drug-interactions. Accessed November 20, 2019.
- Spolarich AE. Risk management strategies for reducing oral adverse drug events. J Evid Based Dent Pract. 2014;14(suppl):87–94.
- Brunton LL, Chabner BA, Knollmann, Björn C. Goodman and Gilman’s The Pharmacological Basis of Therapeutics. 13th ed. New York: McGraw Hill; 2018.
- Wilkinson GR. Drug metabolism and variability among patients in drug response. N Engl J Med. 2005;352:2211–2221.
- Levy HB. Polypharmacy reduction strategies: Tips on incorporating American Geriatrics Society Beers and screening tool of older people’s prescriptions criteria. Clin Geriatr Med. 2017;33:177–187.
- DeRhodes KH. The dangers of ignoring the Beers criteria—The prescribing cascade. JAMA Intern Med. 2019;179:863–864.
- Shah BM, Hajjar ER. Polypharmacy, adverse drug reactions, and geriatric syndromes. Clin Geriatr Med. 2012;28:173–186.
- Skaar DD, O’connor H. Using the Beers criteria to identify potentially inappropriate medication use by older adult dental patients. J Am Dent Assoc. 2017;148:298–307.
- Arlt S, Lindner R, Rösler A, von Renteln-Kruse W. Adherence to medication in patients with dementia. Drugs Aging. 2008;25:1033–1047.
- Alter David A. When do we decide that generic and brand-name drugs are clinically equivalent? Circ Cardiovasc Qual Outcomes. 2017;10:e004158.
- Leclerc J, Blais C, Rochette L, Ferguson D, Guénette L, Poirier P. Impact of the commercialization of three generic angiotensin II receptor blockers on adverse events in Quebec, Canada. Circ Cardiovasc Qual Outcomes. 2017;10:e003891.
- Eban K. Opinion | Americans need generic drugs. But can they trust them? The New York Times. Available at: nytimes.com/2019/05/11/opinion/sunday/generic-drugs-safety.html. Accessed November 20, 2019.
- van der Meersch A, Dechartres A, Ravaud P. Quality of reporting of bioequivalence trials comparing generic to brand name drugs: a methodological systematic review. PloS One. 2011;6:e23611.
- Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71:1269–1324.
- Krass I, Schieback P, Dhippayom T. Adherence to diabetes medication: A systematic review. Diabet Med. 2015;32:725–737.
- Office of Disease Prevention and Health Promotion. Preventing Adverse Drug Events: Individualizing Glycemic Targets Using Health Literacy Strategies. Available at: https://health.gov/hcq/trainings/ade-diabetes-agents. Accessed November 20, 2019.
- Genco RJ, Schifferle RE, Dunford RG, Falkner KL, Hsu WC, Balukjian J. Screening for diabetes mellitus in dental practices: A field trial. J Am Dent Assoc. 2014;145:57–64.
- American Diabetes Association. Statistics About Diabetes. Available at: diabetes.org/diabetes-basics/statistics/. Accessed November 20, 2019.
- Kocher T, König J, Borgnakke WS, Pink C, Meisel P. Periodontal complications of hyperglycemia/diabetes mellitus: Epidemiologic complexity and clinical challenge. Periodontol 2000. 2018;78:59–97.
- Kitabchi AE, Umpierrez GE, Murphy MB, Kreisberg RA. Hyperglycemic crises in adult patients with diabetes. Diabetes Care. 2006;29:2739.
- American Diabetes Association. Standards of medical care in diabetes—2019 abridged for primary care providers. Clin Diabetes. 2019;37:11–34.
From Dimensions of Dental Hygiene. December 2019;17(11):40–43.