 MALAMUS-UK/ISTOCK/GETTY IMAGES PLUS
MALAMUS-UK/ISTOCK/GETTY IMAGES PLUS
Efficacy of Hand Instrumentation vs Power Instrumentation
Research shows that both methods are equally effective in nonsurgical periodontal therapy.
Dental hygienists face many challenges as they practice during a global pandemic. The strict implementation of a variety of new infection control guidelines needed to prevent the transmission of SARS-CoV-2 has changed the way many oral health professionals practice. On June 9, 2020, the American Dental Association’s (ADA) Advisory Task Force on Dental Practice Recovery issued guidelines that included the preferred use of hand instrumentation over ultrasonic instrumentation for plaque and calculus removal to reduce aerosol production.1
As many clinicians are accustomed to using power instrumentation during periodontal therapy, this article will examine the effectiveness of hand instrumentation in the removal of soft and hard deposits compared to the combined approach of hand and power instrumentation to prevent and treat periodontal diseases.2
Reducing Transmission
SARS-CoV-2 is spread by airborne droplets.3 Studies also suggest that the virus may be transmitted by aerosols created during medical or dental treatments.4 In order to reduce possibility of transmission, changes to the provision of oral healthcare have been implemented including more frequent hand washing, patient screening, additional personal protective equipment (PPE), use of rubber dams and preprocedural mouthrinses, and reduction of aerosol production.
For dental hygienists, the recommendation to reduce the use of power instrumentation is significant. Procedures involving the use of ultrasonic scalers and air polishing are considered high risk for oral health professionals.2 However, research shows that hand and ultrasonic instrumentation are equally effective in dental biofilm and calculus removal.3
Instrumentation Methods
The main objective of nonsurgical periodontal therapy is the complete removal of elements that cause gingival inflammation.5 Nonsurgical periodontal treatment, including scaling and root planing, is considered the gold standard for the treatment of periodontal diseases. The goal of nonsurgical periodontal therapy is to create smooth root surfaces to facilitate reattachment of fibers and promote gingival healing.6 Scaling and root planing using hand instrumentation has been a standard in periodontal therapy for many years, while ultrasonic instrumentation was first introduced in the 1960s.7
In light of the new guidelines issued to protect dental professionals and their patients from the spread of COVID-19 in the dental setting, the use of ultrasonic instrumentation should be avoided or minimized because it creates aerosols.
Clinical trials evaluating the effectiveness of manual and ultrasonic subgingival instrumentation in periodontal treatment of cases with initial medium (4 mm to 6 mm) and deep (> 6 mm) pockets have been conducted.8 Findings show that hand instrumentation is more effective in pocket reduction in cases with moderate to deep pockets, as well as reducing bleeding on probing and improving clinical attachment in cases with deep pockets.8 Other studies suggest that patient outcomes are similar, regardless of the type of instrumentation used.5 However, many clinicians question the efficacy of hand instrumentation alone. Patients may also be concerned about the completeness of their treatment without the use of ultrasonic instruments.
Procedures involving the use of ultrasonic scalers and air polishing are considered high risk for oral health professionals.
Pros and Cons
A large amount of in vivo and in vitro research has compared ultrasonic and manual instruments, and few differences have been found in clinical effects, changes in microflora, and root surface characteristics. In fact, little evidence exists comparing the clinical effects of ultrasonic subgingival scaling with or without hand instrumentation.
Krishna and De Stefano9 discussed the benefits and disadvantages of hand and ultrasonic instrumentation in the treatment and management of periodontal diseases. They concluded that no significant differences exist in patient outcomes based on the use of one technique vs the other. In a study comparing root surfaces of periodontally treated roots, surfaces treated exclusively by hand instruments had smoother surfaces than roots treated with ultrasonic scalers.6 Despite the fact that root surfaces treated by curets were smoother, the study found little difference in root surface roughness, elastic modulus, and hardness. Krishna and De Stefano9 support the hypothesis that the ultrasonic instrumentation is not superior to hand instrumentation in the fight against periodontal diseases.
A clinical trial published in the Journal of Clinical Periodontology investigated the use of hand instrumentation and power instrumentation on healing at 3-month and 6-month benchmarks.10 Bleeding on probing, pocket depths, plaque index, clinical attachment loss, and number of pockets were recorded at the start of the study. Treatment was provided in randomly assigned quadrants using various techniques, such as hand scaling, ultrasonic scaling, combination of hand and ultrasonic scaling, and other power instruments. The study found power instruments to be as effective as conventional therapy, as similar improvement in clinical parameters was noted in all quadrants.10
Additionally, a systematic review evaluated various subgingival instrumentation techniques.11 Results of the review concluded that all types of nonsurgical periodontal therapy were equally as effective in achieving a reduction in inflammation associated with periodontitis regardless of the type of instrument used.
Laleman et al7 also supported the hypothesis that hand and power instrumentation are equally effective, but they noted that the main differences are in the use of water with ultrasonic instruments, citing the reduction in frictional overheating, in addition to ease of use and a supposed reduction in time spent on periodontal debridement.
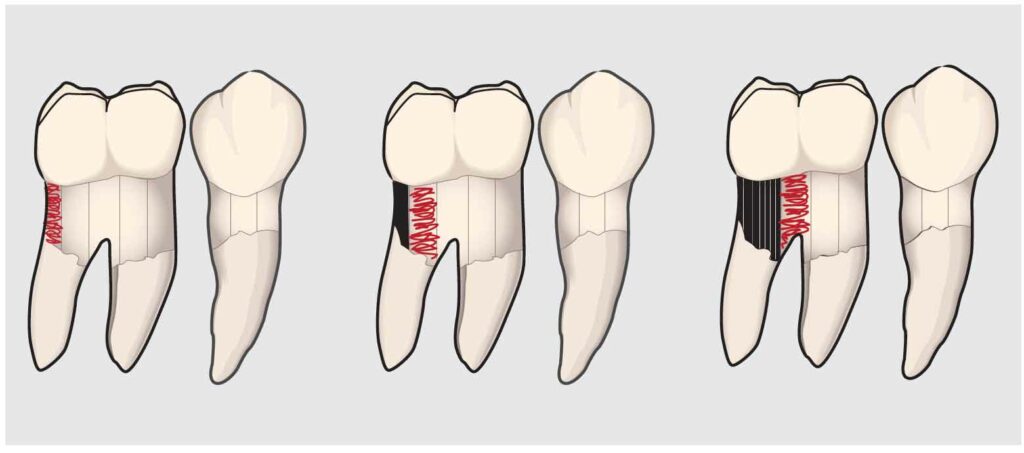
Kim et al12 suggest that the water lavage in ultrasonic instrumentation is important to calculus removal and mechanical chipping action of the oscillating insert/tip. However, the same study also warned of potential damage to the compromised enamel surfaces, early caries lesions, and composite restorations caused by oscillating effects of the ultrasonic instruments. Johnston13 states that inflammatory response to both types of instrumentation is similar, but noted that clinician ergonomics is improved and clinician fatigue is decreased with ultrasonic instrumentation. However, ultrasonic instrumentation requires precise technique, not haphazard movement, and when performed correctly, should not take a much shorter time than hand instrumentation (Figure 1).14 Oral health professionals frequently implement long, quick strokes that do not fully remove calculus deposits when using power instrumentation. Ultrasonic instruments can also burnish calculus deposits onto the root surface—inciting inflammation—if not used with the correct technique.15
Practical Application
According to a British survey, more than 50% of dental hygienists are willing to comply with current guidelines and limit their instrument selection to hand instrumentation only.2 To ensure effective instrumentation and reduce treatment time and operator fatigue, a variety of hand instruments should be used.16 Depending on the type of deposits and periodontal case, use of area-specific instruments, instruments with rigid shank for heavy tenacious deposits, longer shank for pockets deeper than 5 mm, and instruments with smaller working ends are recommended. The British survey also found that fewer than 50% of United Kingdom dental hygienists felt they had enough variety of hand instruments available.2
Ultrasonic instrumentation requires precise technique, not haphazard movement.
Conclusion
With the ADA strongly recommending the use of hand scaling during the COVID-19 pandemic, dental hygienists should be prepared to provide the most effective nonsurgical periodontal therapy with hand instrumentation. The literature shows that hand scaling and ultrasonic instrumentation are both equally effective for biofilm and calculus removal. There is no difference between the response of the systemic inflammatory response after a full debridement using hand or ultrasonic instruments.13 While the preferred technique in prepandemic times was the blended approach of both power and hand instrumentation, dental hygienists must remain flexible in their ability to provide high-quality care while also reducing the risk of viral transmission.
References
- American Dental Association. Return to Work Interim Guidance Toolkit. Available at: actx.edu/dent_l_hy/files/filecabinet/folder3/DHYG_1319.pdf. Accessed April 21, 2021.
- Wadia R, D’Cruz, L, Baker L. COVID-19: working as a hygienist or therapist. BDJ Team. 2020;7:22–23.
- Baghizadeh Fini M. What dentists need to know about COVID-19. Oral Oncol. 2020;105:104–741.
- Jamal M, Shah M, Almarzooqi SH, et al. Overview of transnational recommendations for COVID-19 transmission control in dental care settings. Oral Dis. 2021;27(Suppl 3):655–664.
- Yue Y, Yalin Z, Xian’e W, Jianxia H. Clinical evaluation of ultrasonic subgingival debridement versus ultrasonic subgingival scaling combined with manual root planing in the treatment of periodontitis: study protocol for a randomized controlled trial. Trials. 2020;21:1–7.
- Zafar M. Comparing the effects of manual and ultrasonic instrumentation on root surface mechanical properties. Eur J Dent. 2016;4:517.
- Laleman I, Cortellini S, De Winter S, et al. Subgingival debridement: end point, methods and how often? Periodontol. 2017;75:189–204.
- Zhang X, Hu Z, Zhu X. et al. Treating periodontitis-a systematic review and meta-analysis comparing ultrasonic and manual subgingival scaling at different probing pocket depths. BMC Oral Health. 2020;20:176.
- Krishna R, De Stefano JA. Ultrasonic vs. hand instrumentation in periodontal therapy: clinical outcomes. Periodontol 2000. 2016;71:113–127.
- Ranjitha K, Jamie ADS. Ultrasonic vs. hand instrumentation in periodontal therapy: clinical outcomes. Periodontol 2000. 2016;71(1):113-127.
- Suvan J, Leira Y, Moreno Sancho FM, et al. Subgingival instrumentation for treatment of periodontitis. A systematic review. J Clin Periodontol. 2020;47:155–175.
- Kim SY, Kang MK, Kang SM, Kim HE. Effects of ultrasonic instrumentation on enamel surfaces with various defects. Int J Dent Hyg. 2018;2:219.
- Johnston W, Paterson M, Piela K, et al. The systemic inflammatory response following hand instrumentation versus ultrasonic instrumentation: a randomized controlled trial. J Clin Periodontol. 2009;36:132–141.
- Matsuda S. Decision making in ultrasonic instrumentation. Dimensions of Dental Hygiene. 2017;15(1):24–26.
- Brookman L, Smith D. The bane of burnished calculus. Dimensions of Dental Hygiene. 2017;15(2):28–31.
- Beleno Sanchez J, Nguyen M. Improve nonsurgical periodontal therapy with appropriate instrument choice. Dimensions of Dental Hygiene. 2021;19(2):16–21.
From Dimensions of Dental Hygiene. May 2021;19(5):18,21-22.

