Educate Your Patients About HPV
Dental hygienists can serve as the first line of defense in detecting and treating oral human papillomavirus.
This course was published in the January 2012 issue and expires January 2015. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Discuss the incidence and pathophysiology of human papillomavirus (HPV).
- Identify the oral manifestations of HPV infection.
- Explain the association between oral HPV and oral cancer.
- Detail the dental hygienist’s role in the early detection and treatment of oral HPV.
According to the United States Centers for Disease Control and Prevention (CDC), approximately 20 million Americans are currently infected with human papillomavirus (HPV), and another 6 million will become newly infected each year.1 Most people who become infected with HPV do not know they have it.1 Although HPV is considered a common virus, it poses a serious public health threat.
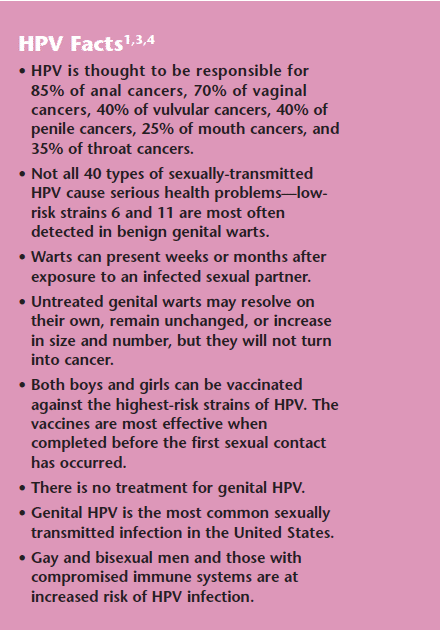
There are more than 100 strains of HPV, with approximately 60 types causing warts on areas such as the hands and feet.2,3 The other 40 types are sexually transmitted.3 Each type has a unique DNA sequence and affects the health of its host differently. Some strains are harmless, while others are more serious; for example, nearly all cervical cancers are caused by HPV.4 (See sidebar for more details about the virus.)
HPV strains are grouped into cutaneous and mucosal types based on their tissue tropism. Cutaneous types cause common warts. Mucosal HPV strains are additionally classified into low-risk and high-risk categories based on their association with cervical cancer. HPV strains 6 and 11 are low-risk and cause benign genital warts. High-risk strains include 16, 18, 31, and 45, and are all related to cervical cancer.
HPV infection can cause healthy cells to develop abnormalities. In most cases, the body fights off HPV naturally and the infected cells return to normal.1 But when the immune system is unsuccessful in eliminating HPV, visible changes will occur. HPV infection is limited to the basal cells of stratified epithelium—the only tissue in which they replicate.5 The virus cannot bind to live tissue, but instead infects epithelial tissues through micro-abrasions or other trauma that exposes segments of the basement membrane.5
Oral Considerations
HPV infection can also cause oral lesions, which may be located in any region of the ororespiratory tract, including the oral cavity, nasal passages, esophagus, and larynx.2
Dental hygienists play an important role in locating these lesions during intraoral examinations and referring patients for diagnosis. Benign oral lesions caused by HPV include: squamous papilloma, verucca vulgaris, condyloma acuminatum, and focal epithelial hyperplasia.2 These lesions may look similar clinically, but they are caused by different subtypes of HPV, and they differ histologically.2
Recent research indicates that HPV infection may be an important risk factor for head and neck cancers—particularly squamous-cell carcinomas that arise from the lingual and palatine tonsils.6,7 HPV is involved in approximately 50% of tonsillar cancer cases, and 28% to 35% of oropharyngeal cancers.8 Tobacco and alcohol use are the traditional risk factors for cancers of the head and neck, but data now suggest there are two pathways in which oropharyngeal cancer develops.8 One pathway is directly related to tobacco or alcohol use, and the other is related to HPV infection.8
Although HPV 16 is the most frequent strain associated with oral cancer, types 6, 7, 33, 35, and 39 have also been found in oral cancer lesions.2 HPV-positive tumors are more prevalent among younger patients than tumors related to tobacco and alcohol use.9 Patients with HPV-positive tumors tend to have a lower risk of cancer death than those with HPV-negative tumors.10 A case control study found that oral HPV infection is strongly associated with oropharyngeal cancer, regardless of tobacco and alcohol use.11 This study also found that tobacco and alcohol were important risk factors for oropharyngeal cancer, but they did not seem to have a synergistic effect in HPV-mediated carcinogenesis, (ie, the combined exposure to HPV and heavy tobacco and alcohol use was not additive).11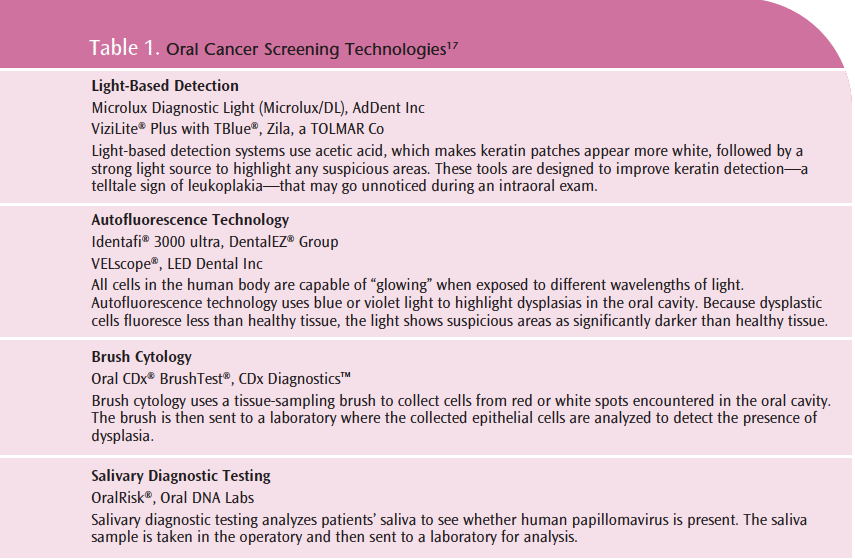
Oropharyngeal cancers are a significant cause of morbidity and mortality worldwide—there are approximately 560,000 cases and 300,000 deaths annually.6 Most oral cancers are asymptomatic, thus they often remain undiagnosed until later stages. Oral cancers that are diagnosed early have a 80% to 90% cure rate, but when discovered later, the cure rate drops to 45% at 5 years post-diagnosis.9
Oral HPV infection is sexually acquired via oral-genital contact.9 The greatest risk factor for oral HPV infection is the practice of oral sex. Other risk factors include: young age at first intercourse, a history of sexually transmitted infection, engagement in casual sex, infrequent use of condoms, and high number of sexual partners—particularly oral sexual partners.10-12
The incidence of tonsillar and base-of-tongue cancers in the US has increased annually since 1973; this increased incidence may be due to changes in sexual practices, eg, the increased popularity of oral sex. HPV DNA was detectable in 23% of tonsillar cancers in the 1970s, compared to 93% in 2006.12 This trend is a major public health concern, and dental hygienists are in a unique position to discuss HPV prevention with their patients.
Detection and Treatment
Dental hygienists can recognize potential HPV lesions in the oral cavity, and knowing what to look for is vital to early detection. Oral HPV can take on many appearances.2 Clinically, HPV lesions can be the same color as the surrounding tissues or appear white—depending on the keratin present.2 HPV can present as a papilloma with a bumpy surface or finger-like projections attached by a stalklike base or a flat base, as verruca or wart-like lesions, or as multiple papillimatous nodules.2 A thorough, systematic approach to the extraoral and intraoral exam and meticulous documentation are necessary for effective detection. Any suspicious lesion should be evaluated by the dentist.
Several oral cancer screening technologies are available to aid in early detection (Table 1). HPV can be present and communicable even when lesions are not present. Salivary diagnostic testing can detect the presence of HPV in the absence of a lesion.13 Patients who have the virus but do not present with lesions should receive frequent intraoral exams to ensure that any lesion is detected and treated early. Not everyone who has HPV present in their saliva will develop lesions, and certainly not all lesions will become malignant. All patients with suspicious lesions, however, should be referred for biopsy.14 Patients without any evidence of a lesion but who test positive on a salivary diagnostic test for HPV should be retested to look for a persistent HPV infection.15 If an HPV infection persists for longer than 1 year, the infection is chronic and may be more likely to contribute to cell changes that could result in cancer.15
Treatment for patients with suspicious lesions may include laser removal, surgical excision of the lesion, or a “watch and wait” approach, depending on the biopsy findings. If the lesion is cancerous, treatment and follow-up procedures will be based on the stage of disease progression.
Dental Hygienist’s Role
Dental hygienists play an important role in the early detection of and education about HPV. Anyone who is sexually active could be at risk of HPV. In determining the need for screening, patients should be questioned about behaviors that may put them at risk of HPV infection. Although asking questions about patients’ sexual behaviors may initially feel awkward, approaching the topic with respect and confidence will help ease the discussion. Educating patients about the prevalence of HPV and its relationship to oral cancer provides an opening for the discussion about their personal risks and the importance of oral cancer exams.
Conclusion
With the link between HPV and oral cancer becoming more clear and the rate of HPV infection increasing, dental hygienists will become vital components of the health care team that confronts this significant public health issue. Diligence in HPV education and oral cancer screening can literally save lives.
PHOTO CREDIT
HEADER IMAGE: JAMES CAVALLINI/PHOTO RESEARCHERS INC
REFERENCES
- CDC. Genital HPV Infection Fact Sheet. Available at: www.cdc.gov/std/HPV/STDFact- HPV.htm#common. Accessed December 19, 2011.
- Lukes SM, Meneses MB. The dental hygienist’s role in HPV recognition. Dimensions of Dental Hygiene. 2010;8:72–77.
- WebMD. HPV/Genital Warts Health Center. Available at: www.webmd.com/sexualconditions/hpv-genital-warts/hpv-virusinformation-about-human-papillomavirus. Accessed December 19, 2011.
- CDC. HPV-Associated Cancers Statistics. Available at: www.cdc.gov/cancer/hpv/statistics. Accessed December 19, 2011.
- Warren K. HPV knowledge among female college students and the short term effectiveness of HPV education. The Internet Journal of Academic Physician Assistants. 2010;7:1-20.
- Gillison ML. Oropharyngeal cancer: a potential consequence of concomitant HPV and HIV infection. Curr Opin Oncol. 2009;21:439-444.
- Kreimer AR, Alberg AJ, Daniel R, et al. Oral human papillomavirus infection in adults is associated with sexual behavior and HIV serostatus. J Infect Dis. 2004;189:686-698.
- Chustecka Z. Oropharyngeal cancer linked to human papillomavirus. Available at: www.medscape.com/viewarticle/556285. Accessed December 19, 2011.
- HPV-positive oral cancer. Dental Abstracts. 2010;55:216-217.
- Downs JZ, Thompson SK. Prevent HPV. Dimensions of Dental Hygiene. 2010;8:30-34.
- D’Souza G, Kreimer AR, Viscidi R, et al. Casecontrol study of human papillomavirus and oropharyngeal cancer. N Engl J Med. 2007; 356: 1944-1956.
- Schiller JT, Day PM, Kines RC. Current understanding of the mechanism of HPV infection. Gynecol Oncol. 2010;118(Suppl 1): S12-S17.
- DiMatteo A. Salivary diagnostics: The anatomy of an opportunity. Inside Dentistry. 2010;6:122-134.
- Greco NM, Greco, M. Human papillomavirus. Access. 2010;24:18-27.
- Cleveland T. Oral cancer related to HPV. Access. 2011;25:9,23.
- Varnai AD, Bollman M, Bankfalvi A, et al. The prevalence and distribution of human papillomavirus genotypes in oral epithelial hyperplasia: proposal of a concept. J Oral Pathol Med. 2009;38:181-187.
- Bouquot JE, Suarez P, Vigneswaran N. Oral precancer and early cancer detection in the dental office—review of new technologies. J Implant Adv Clin Dent. 2010;2:47-63.
From Dimensions of Dental Hygiene. January 2012; 10(1): 52-55.



