Dangerous Deficiency
Vitamin D deficiency is widespread and has serious oral and systemic health effects.
This course was published in the December 2010 issue and expires December 2013. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Define the function of vitamin D.
- Discuss which populations are at risk of vitamin D deficiency.
- Explain how vitamin D is synthesized in the body.
- List the negative side effects of vitamin D deficiency on oral and systemic health.
Vitamin D deficiency is rampant across the globe regardless of age, gender, ethnicity, socioeconomic status, or level of health.1 The prevalence of vitamin D deficiency among certain populations may be as high as one in two people.1,2 Certain diseases substantially reduce circulating vitamin D levels including bone and muscle disorders, some cancers, chronic liver disease, fat malabsorption syndromes, Crohn’s disease, cystic fibrosis, autoimmune disorders, multiple sclerosis, and rheumatoid arthritis.3,4
The widespread deficiency of this important vitamin may have significant health consequences beyond even the traditional result of bone loss and insufficient bone development. Geography and lifestyle factors affect people’s vitamin D levels. Research shows that those who live north of 30° latitude, which in the United States is approximately north of Atlanta in the East and north of Los Angeles in the West, are at higher risk of vitamin D deficiency and face increased risk of developing certain cancers, such as colon, breast, prostate, pancreas, and leukemia.5,6 Certain medications, alcohol consumption, and tobacco use may also have a negative impact on circulating vitamin D levels. Dietary vitamin D supplements are the most efficient, economical means of raising and maintaining circulating vitamin D blood levels because receiving enough through sunlight exposure or dietary intake is difficult. As preventive specialists, dental hygienists are perfectly poised to encourage their patients to have their vitamin D levels evaluated as part of the routine blood work conducted during an annual physical.
VITAMIN D PARAMETERS
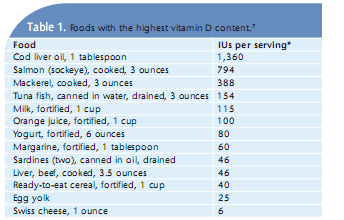
The primary function of vitamin D is to regulate calcium and phosphorus levels and bone metabolism. A unique fat-soluble nutrient, vitamin D occurs naturally in a limited number of foods and is produced in the skin after direct sun exposure. Fatty fish contain the highest amounts of vitamin D while other animal products contain low amounts (see Table 1).7
Many foods are fortified with vitamin D2 or ergocalciferol, which is derived from plants. Sun exposure produces vitamin D3, or cholecalciferol, which is also found in vitamin supplements and is the form most easily absorbed by the body. Both forms are transported to the liver through vitamin D binding protein (DBP) where they are then metabolized by the kidneys (see Figure 1). In the liver, the enzyme 25-hydroxylase converts vitamin D to circulating serum 25(OH)D, which is what is measured when determining vitamin D levels in the body. Low serum calcium stimulates the parathyroid glands to produce and secrete parathyroid hormone (PTH). This hormone conserves available calcium by increasing its resorption by the kidneys.
The biologically active form of vitamin D helps protect the body against invading bacteria. Its most important function is to aid in the absorption of calcium from the intestines to help the body maintain adequate levels of calcium to support bone health. Vitamin D also reduces inflammation, facilitates neuromuscular function, and supports healthy gene activity.
Because most people no longer spend the majority of their time outside during the day, many are at risk of vitamin D deficiency. Plus, the form of vitamin D found in foods is more difficult to absorb than the type created via sun exposure. See Table 2 for a list of populations at risk of vitamin D deficiency. People who are vitamin D deficient are at a higher risk of a myriad of chronic diseases including cancer and diabetes.
CANCER
Studies suggest that the risk of some types of cancer, including colorectal cancer, is lower in people with high levels of calcium and vitamin D. 8,9 One study showed that women who were deficient in vitamin D had a 253% increased risk of developing colorectal cancer.10 Another study found that women who consumed 1,100 international units (IUs) of vitamin D with calcium a day decreased the overall risk of developing cancer by almost 70%.11
Vitamin D intake, serum blood levels of 25(OH)D, and increased sun exposure have all shown to reduce breast cancer risk in some epidemiologic studies.12 In addition, certain vitamin D receptors may modify breast cancer susceptibility.12 Estrogen deficiencies appear to reduce vitamin D levels, which may put post-menopausal women at an increased risk of breast cancer.13 High dose vitamin D supplementation may slightly reduce the risk of developing breast cancer.10,14 Evidence supports vitamin D as a defender against prostate, colon, and breast cancer.15 Additional study in this area is needed, however.
OSTEOPOROSIS
Osteoporosis is the most common metabolic bone disease, and vitamin D deficiency is an established risk factor. 10,16 Severe deficiency causes osteomalicia, the under-mineralization of skeletal tissues due to low intestinal absorption of calcium. Combining calcium and vitamin D supplements decreases fractures and increases bone mineral density (BMD).14,16 Osteoporosis is directly related to insufficient vitamin D intake because of suppressed calcium absorption in the intestines. Low serum 25(OH)D levels are associated with decreased calcium absorption rates and hyperparathyroidism, which leads to bone loss.14 When circulating levels of 25(OH)D measure below 32 ng/mL, calcium absorption is impaired. Secondary hyperparathyroidism and poor calcium absorption due to vitamin D deficiency have harmful effects on skeletal integrity and are associated with lower BMD and increased risk of bone fractures.17 Secondary hyperparathyroidism is the main characteristic of poor nutritional status in older adults.17
PAIN

Chronic musculoskeletal pain occurs with a lack of circulating calcium (hypocalcemia) due to inadequate vitamin D, which then elevates the PTH that diminishes bone density (osteopenia) and affects bone architecture (osteoporosis). Osteomalicia, (bone metabolism dysfunction) causes persistent, generalized musculoskeletal pain and weakness.18
Increased PTH levels impair proper bone mineralization, causing a spongy matrix to form under the periosteal membrane. This matrix is gelatin-like and can absorb fluid, expand, and cause outward pressure on periosteal tissues. These tissues are highly innervated with sensory pain fibers, which cause the sensation of musculoskeletal pain. Patients with chronic pain, muscle weakness or fatigue, fibromyalgia, and chronic fatigue syndrome may benefit from high doses of vitamin D after differential diagnosis has ruled out fractures, anatomical pain, neuropathic disorders, or injury-related causes. Vitamin D has shown to alleviate pain associated with migraine headaches in post-menopausal women.19
DIABETES
Low serum levels of vitamin D may be a contributing factor to diabetes.20 Vitamin D insufficiency may also result in insulin resistance. 21 Men and women who ingest more than 800 IUs of vitamin D daily in conjunction with recommended doses of calcium reduce their risk of developing type 2 diabetes.22 There may be an association between adequate vitamin D exposure in early childhood and a reduced risk of developing diabetes.20-23 In addition, increased vitamin D may improve insulin sensitivity and promote beta-cell survival.23,24 Zipitis and Akobeng found that infants given calcitriol during the first year of life were less likely to develop type 1 diabetes than infants fed lesser amounts of vitamin D.25
Among people who have diabetes, 60% are vitamin D deficient.26 The use of cod liver oil as a source of vitamin D to reduce the incidence of type 1 diabetes may be an option.25 Chiu et al found that adults given vitamin D supplementation experienced improve insulin sensitivity.27
OLDER ADULTS
Older adults are at a significant risk of vitamin D deficiency and subsequent bone fractures. 28 Muscle weakness is also a side effect of vitamin D deficiency and compounds the risk of fractures due to falls. Up to 99% of long-term care residents are deficient in vitamin D.29
The older adult population exhibits vitamin D deficiency due to lack of exercise, reduced exposure to sunlight, and limited production/absorption of vitamin D through the skin, which deteriorates with age. Also contributing to vitamin D deficiency is poor consumption of adequate food sources containing vitamin D and calcium. One proposed solution is to supplement the diets of older adults with calcium and vitamin D, a combination that has reduced rates of nonvertebral fracture among elderly women living in retirement homes.30
ORAL HEALTH
Research shows a strong association between osteoporosis/BMD and alveolar bone and tooth loss.31-34 This may indicate that inferior bone characteristics, due to age, smoking, and vitamin D deficiencies, are risk factors for periodontal diseases.31-34 Calcium and vitamin D may benefit periodontal health, and calcium and vitamin D deficiencies may be risk factors for periodontal diseases.35
A recent National Health and Nutrition Examination Survey (NHANES) found that low serum 25(OH)D concentrations were associated with periodontal diseases and loss of alveolar attachment in men and women over the age of 50.36 In addition, research shows that vitamin D supplements decrease tooth loss significantly in those older than age 50.37 Several risk factors are shared by periodontal diseases and osteoporosis; as such, they may be biologically linked.38 Animal studies have shown that vitamin D’s anti-inflammatory properties decrease pro-inflammatory cytokines (C-reactive proteins, interleukin 6 and 12) as well as increase anti-inflammatory cytokines (interleukin-10).39-42 More research is needed to explore expanded uses of vitamin D in conjunction with traditional periodontal therapies. With the risks of vitamin D deficiency so high and its prevalence so widespread, dental professionals should advise their patients to have their levels of vitamin D tested. Part two of this series will focus on the best way to measure vitamin D levels in the blood and supplementation recommendations.
REFERENCES
- Holick M. High prevalence of vitamin D inadequacy and implications for health. Mayo Clin Proc. 2006;81:353-373.
- Chapuy MC, Preziosi P, Maamer M, et al. Prevalence of vitamin D insufficiency in an adult normal population. Osteoporos Int. 1997;7:439-443.
- Mascarenhas R, Mobarhan S. Hypovitaminosis D-induced pain. Nutr Rev. 2004;62:354-359.
- Raiten DJ, Picciano MF. Vitamin D and health in the 21st century: bone and beyond. Executive summary. Am J Clin Nutr. 2004;80:1673S-1677S.
- Gorham E, Garland CF, Garland FC, et al. Vitamin D and prevention of colorectal cancer. J Steroid Biochem Mol Biol. 2005;97:179-194.
- Grant WB. Lower vitamin-D production from solar ultraviolet-B Irradiance may explain some differences in cancer survival rates. J Natl Med Assoc. 2006;98:357-364.
- United States Department of Agriculture, Agricultural Research Service. USDA Nutrient Database for Standard Reference. Available at: www.nal.usda.gov/fnic/foodcomp/search/. Accessed November 22, 2010.
- Feskanich D, Fuchs CS, Kirkner GJ, Hankinson SE, Hollis BW, Giovannucci EL. Plasma vitamin D metabolites and risk of colorectal cancer in women. Cancer Epidemiol Biomarkers Prev. 2004;13:1502-1508.
- Garland C, Shekelle RB, Barrett-Connor E, Criqui MH, Rossof AH, Paul O. Dietary vitamin D and calcium and risk of colorectal cancer: a 19 year prospective study in men. Lancet. 1985;1:307-309.
- Holick M. Vitamin D deficiency. N Engl J Med. 2007;357:266-281.
- Lappe J, Travers-Gustafson D, Davies KM, Reck?er RR, Heaney RP. Vitamin D and calcium supplementation reduces cancer risk: results of a randomized trial. Am J Clin Nutr. 2007;85:1586-1591.
- Yan C, Rohan, TE. Vitamin D, calcium, and breast cancer risk: A review. Cancer Epidemiol Biomarkers Prev. 2006;15:18.
- Chapuy MC, Arlot ME, Duboeuf F, et al. Vitamin D3 and calcium to prevent hip fractures in elderly women. N Engl J Med. 1992;327:1637-1642.
- Ooms ME, Roos JC, Bezemer PD, van der Vijgh WJ, Bouter LM, Lips P. Prevention of bone loss by vitamin D supplementation in elderly women: a randomized double-blind trial. J Clin Endocrinol Metab. 1995;80:1052-1058.
- Guyton K, Kensler TW, Posner GH. Cancer chemoprevention using natural vitamin D and synthetic analogs. Annual Annu Rev Pharmacol Toxicol. 2001;41:421-442.
- Chevalley T, Rizzoli R, Nydegger V, et al. Effects of calcium supplements on femoral bone mineral density and vertebral fracture rate in vitamin-D-replete elderly patients. Osteoporos Int. 1994;4:245-252.
- Hollis BW. Circulating 25-hydroxyvitamin D levels indicative of vitamin D sufficiency: implications for establishing a new effective dietary intake recommendation for vitamin D. J Nutr. 2005135:317-322.
- Johnson E. Vitamin D. Merck Manual Available at: www.merckmanuals.com/professional/sec01/ch004/ch004k.html?qt=vitamin%20d&alt=sh#sec01-ch004-ch004l-451. Accessed November 21, 2010.
- Thys-Jacobs S. Alleviation of migranes with therapeutic vitamin D and calcium. Headache. 1994;34:590-592.
- McKeigue P, Pierpoint, T, Ferrie, JE, MarmotMG. Relationship of glucose intolerance and hyperinsulinaemia to body fat pattern in south Asians and Europeans. Diabetologia. 1992;35:785-791.
- Baynes K, Boucher BJ, Feskens EJM, Kromhout D. Vitamin D, glucose tolerance and insulinaemia in elderly men. Diabetologia. 1997;40:344-347.
- Pittas A, Lau J, Hu FB, Dawson-Hughes B. The role of vitamin D and calcium in type 2 diabetes. A systematic review and meta-analysis. J Clin Endocrinol Metab. 2007;92:2017-2029.
- Palomer X, Gonzalez-Clemente JM, Blanco-Vaca F. Role of vitamin D in the pathogenesis of type 2 diabetes mellitus. Diab Obes Metab. 2008;10:185-197.
- Boucher B. Inadequate vitamin D status: does it contribute to the disorders comprising syndrome ‘X’? Br J Nutr. 1998;79:315-327.
- Zipitis CS, Akobeng AK. Vitamin D supplementation in early childhood and risk of type 1 diabetes: a systematic review and meta-analysis. Arch Dis Child. 2008;93:512-517.
- Holick MF. Vitamin D: importance in prevention of cancers, type 1 diabetes, heart disease, and osteoporosis. Am J Clin Nutr. 2004;79:362-371.
- Chiu KC, Chu A, Go VLW, Saad MF. Hypo?vita?minosis D is associated with insulin resistance and {beta} cell dysfunction. Am J Clin Nutr. 2004;79:820-825.
- Bischoff-Ferrari HA, Willett WC, Wong JB, Giovannucci E, Dietrich T, Dawson-Hughes B. Fracture prevention with Vitamin D supplementation: a meta-analysis of randomized controlled trials. JAMA. 2005;293:2257-2264.
- Holick M. The vitamin D epidemic and its health consequences. J Nutr. 2005;135:2739S-2748S.
- Dawson-Hughes B, Harris SS, Krall EA, Dallal GE. Effect of calcium and vitamin D supplementation on bone density in men and women 65 years of age or older. N Engl J Med. 1997;337:670-676.
- Payne JB, Reinhardt RA, Nummikoski PV, Dunning DG, Patil KD. The association of cigarette smoking with alveolar bone loss in postmenopausal females. J Clin Periodontol. 2000;27:658-664.
- Payne JB, Reinhardt RA, Nummikoski PV, Patil KD. Longitudinal alveolar bone loss in postmeno?pausal osteoporotic/osteopenic women. Osteoporos Int. 1999;10:34-40.
- Wactawski-Wende J, Grossi SG, Trevisan M, et al. The role of osteopenia in oral bone loss and periodontal disease. J Periodontol. 1996;67:1076-1084.
- Ruttimann UE, Webber RL, Hazelrig JB. Fractal dimension from radiographs of peridental alveolar bone: A possible diagnostic indicator of osteoporosis. Oral Surg Oral Med Oral Pathol. 1992;74:98-110.
- Bischoff-Ferrari HA, Giovannucci E, Willett WC, Dietrich T, Dawson-Hughes B. Estimation of optimal serum concentrations of 25-hydroxyvitamin D for multiple health outcomes. Am J Clin Nutr. 2006;84:18-28.
- Dietrich T, Joshipura KJ, Dawson-Hughes B, Bischoff-Ferrari HA. Association between serum concentrations of 25-hydroxyvitamin D3 and periodontal disease in the US population. Am J Clin Nutr. 2004;80:108–13.
- Krall EA, Wehler C, Garcia RI, Harris SS, Dawson-Hughes B. Calcium and vitamin D supplements reduce tooth loss in the elderly. Am J Med. 2001;111:452-456.
- von Wowern N, Klausen B, Kollerup G. Osteoporosis: a risk factor in periodontal disease. J Periodontol. 1994;65:1134-1138.
- Boxer R, Dause RA, Walsh SJ. The association between vitamin D and inflammation with the 6-minute walk and frailty in patients with heart failure. J Am Geriatr Soc. 2008;56:454-461.
- D’Ambrosio D, Cippitelli M, Cocciolo MG, et al. Inhibition of IL-12 production by 1,25-dihydroxy vitamin D3. Involvement of NF-kappaB down regulation in transcriptional repression of the p40 gene. J Clin Invest. 1998;101:252-262.
- Schleithoff SS, Zittermann A, Tenderich G, Berthold HK, Stehle P, Koerfer R. Vitamin D supplementation improves cytokine profiles in patients with congestive heart failure: a double-blind, randomized, placebo-controlled trial. Am J Clin Nutr. 2006;83:754-759.
- Van den Berghe G, Van Roosbroeck D, Vanhove P, Wouters PJ, De Pourcq L, Bouillon R. Bone turnover in prolonged critical illness; effect of vitamin D. J Clin Endocrinol Metab. 2003;88:4623-4632.
From Dimensions of Dental Hygiene. December 2010; 8(12): 46-51.