
Current Evidence on the Efficacy of SDF
Silver diamine fluoride provides a variety of benefits in arresting dental caries, yet remains underutilized.
Childhood dental caries continues to be a major public health problem in the United States.1 More than 50% of children and adolescents have experienced tooth decay in primary and permanent teeth.2 Untreated childhood caries can lead to poor quality of life, decrease in social/personal interactions, and long-term oral health effects.2 Those with low socioeconomic status, children who do not receive regular dental care, and those without dental insurance are at increased risk for caries.3
Untreated pediatric caries can progress into the dental pulp chamber, causing infection and discomfort. If left untreated, the infection can expand systemically, increasing the likelihood of delayed growth and development as well as negative effects on general health.4
Receiving dental care can be challenging for children, especially those with special needs, anxiety, attention deficit disorders, attention deficit hyperactivity disorders, and dental phobia.5 Clinicians often make accommodations in the operatory while using behavioral management strategies to meet the special healthcare needs of these patient populations.
Silver diamine fluoride (SDF) can be an effective treatment option for young children and children with special dental management considerations.6 Evidence suggests that the application is painless, simple, and can be ideal for these identified populations.7 Parents/caregivers, patients, and clinicians strive for the most effective, low-stress, and cost-efficient treatment to improve the overall dental care experience, and SDF can be a viable option. However, despite the evidence regarding the efficacy of SDF for dental caries, the translation into practice has yet to be routinely incorporated among dental providers.8
New Addition to the Caries Armamentarium
Despite prevention recommendations, such as fluoride, limiting sugary foods, self-care, and obtaining preventive dental care twice a year, the global prevalence of children developing carious lesions is 46.2% for primary dentition and 53.8% for permanent dentition.8
SDF — a mixture of ionic silver, fluoride, and ammonia — halts the advancement of caries and inhibits the expansion of potential decay.9 It is an appropriate treatment option for patients who may not be good candidates for traditional dental treatments.6 SDF’s ability to arrest caries enables children to mature or improve their health prior to beginning comprehensive restorative therapy.
In 2017, the American Academy of Pediatric Dentistry released evidence-based guidelines for SDF application as well as a chairside guide on case selection, clinical applications, and follow-up care (Figure 1).10 The guidelines recommend the application of 38% SDF once annually and application on high caries-risk patients with active carious lesions. The treatment is also suggested for individuals with special healthcare needs and/or medical conditions that create a challenge for other treatments, patients with numerous carious lesions that cannot be treated in one appointment, individuals with barriers to care, and those who have caries without any pulpal involvement.6
Benefits and Disadvantages
Evidence shows that SDF is equally effective as traditional restorative therapies. A meta-analysis by Ruff et al11 included studies in which SDF was used as a singular treatment or in combination with other nonsurgical therapies (eg, fluoride varnish, atraumatic restorative treatments) and measured the outcome of oral health-related quality of life (OHRQoL), as it relates to functional and emotional well-being and dental treatment satisfaction. The meta-analysis revealed that SDF treatment completed on children was not significantly different than traditional restoration methods. Results across all treatments indicated no differences in OHRQoL when compared to SDF.
Another systematic review and meta-analysis conducted by Wakhloo et al12 compared the clinical efficacy of SDF and atraumatic restorative treatment (ART) in arresting caries found in the primary dentition and first permanent molars of children. The systematic review included five randomized control trials that applied SDF concentrations of 10%, 30%, and 38% annually. However, one study included a bi-annual application, with follow-up evaluations ranging from 12 to 30 months. The review indicated a lack of solid evidence comparing SDF with ART for arresting active dental caries, especially in the first permanent molars. No statistically significant difference was noted with caries arrest between the SDF and ART therapies; however, the number of arrested caries was higher in the SDF group (168/⯰) when compared to the ART group (102/⯎).
Similarly, a systematic review by Jabin et al13 evaluated the effectiveness of SDF in caries arrest in the primary dentition. The cumulative results of the four randomized controlled trials showed that SDF application of 38% concentration is both safe and efficacious for the arrest of dental caries in primary teeth in comparison to lower concentrations (5%, 12%) of SDF.
The most significant disadvantage of using SDF is the black staining that presents on the carious lesion post-application.14 The staining may decrease parental acceptance due to its impact on esthetics. However, a previously discussed systematic review found that the discoloration effects of SDF did not appear to affect OHRQoL outcome findings.11 A systematic review by Roberts et al15 that included six studies tested the possibility of applying potassium iodide (KI) with the SDF application to reduce black staining. The review concluded that although some studies reported a positive effect, inadequate evidence exists supporting a substantial clinical benefit of SDF + KI treatment on tooth staining, mainly due to methodological variations within the current literature. Future studies may help to find a stronger clinical significance.
Parent/Caregiver Acceptance
Many studies have investigated the parent/caregiver acceptance of SDF usage. A meta-analysis by Sabbagh et al16 assessed parent/caregiver acceptance of SDF application and their response to the esthetic outcome of children’s primary dentition. The study evaluated factors that might influence parent/caregiver acceptance of the treatment such as tooth location and child cooperation. Eight studies were chosen after determining inclusion criteria. Statistically significant differences were noted between parent/caregiver acceptance for SDF usage on posterior teeth compared to anterior teeth, and for SDF usage on anterior teeth of uncooperative vs cooperative children. The study also found that the level of parent/caregiver acceptance increased with the incorporation of education and follow-up visits postapplication.
A descriptive, cross-sectional study by Almarwan et al17 assessed parents/caregivers (n=212) of children with special healthcare needs and found increased acceptance of SDF staining when the caries lesion was associated with pain or inflammation. The acceptance was irrespective of tooth location or whether it was a primary or permanent tooth.
Psychological Trauma
Evidence shows a significant difference in emotion-induced trauma in children receiving restorative dental therapies compared to SDF.18 Because the SDF application minimizes pain and treatment time, emotional trauma decreases. Shrivastava et al18 conducted a clinical trial to investigate the effectiveness of SDF (38%) in arresting active carious lesions in primary teeth and to assess parent/caregiver perception regarding SDF application. The perception was related to ease of application, associated discoloration, and SDF taste. A total of 30 children ranging in age from 2 to 10 with active dental caries in primary teeth were treated with one or two topical applications of SDF. Lesions were reevaluated at 1 week and 3 months. Results indicated 80% of dental caries were arrested at first recare and 93.3% after 3 months. No occurrence of pain was documented. Additionally, the study found that most parents had a positive perception of the application process, taste, and esthetics.
Another systematic review conducted by Gao et al7 included eight studies that used 38% SDF to arrest caries in primary teeth. The overall percentage of active caries arrested due to SDF application was 81%. Apart from permanently staining the arrested lesion black, no significant complication of its use among children was reported. The study concluded that the application of SDF is painless and simple and can be used for young children, especially those with special dental care needs.
Application Time
Time is a crucial factor when providing care for pediatric patients. A randomized controlled trial conducted by Vollú et al19 investigated the efficacy of SDF in arresting active caries lesions on the occlusal surface of primary molars among children ages 2 to 5. The 68 participants were randomly allocated into the SDF group or the control group, which received ART. Results showed that the mean difference of arrested lesions between the groups after 12 months was equal, but the time required to treat with SDF was significantly lower than ART.
Similarly, another randomized controlled trial by Abdellatif et al20 found that while there was no significant difference between ART and SDF in efficacy, there was a significant difference in the treatment time. The delivery time for participants (n=26) treated with ART ranged from 3 to 27 minutes with the average time being 14 minutes. The typical time for participants treated with SDF was 3.3 minutes. The shorter application of SDF can be advantageous when providing care for pediatric patients, especially those with behavioral considerations and/or special dental care needs (Figure 2).20
Chairside Application Flowchart
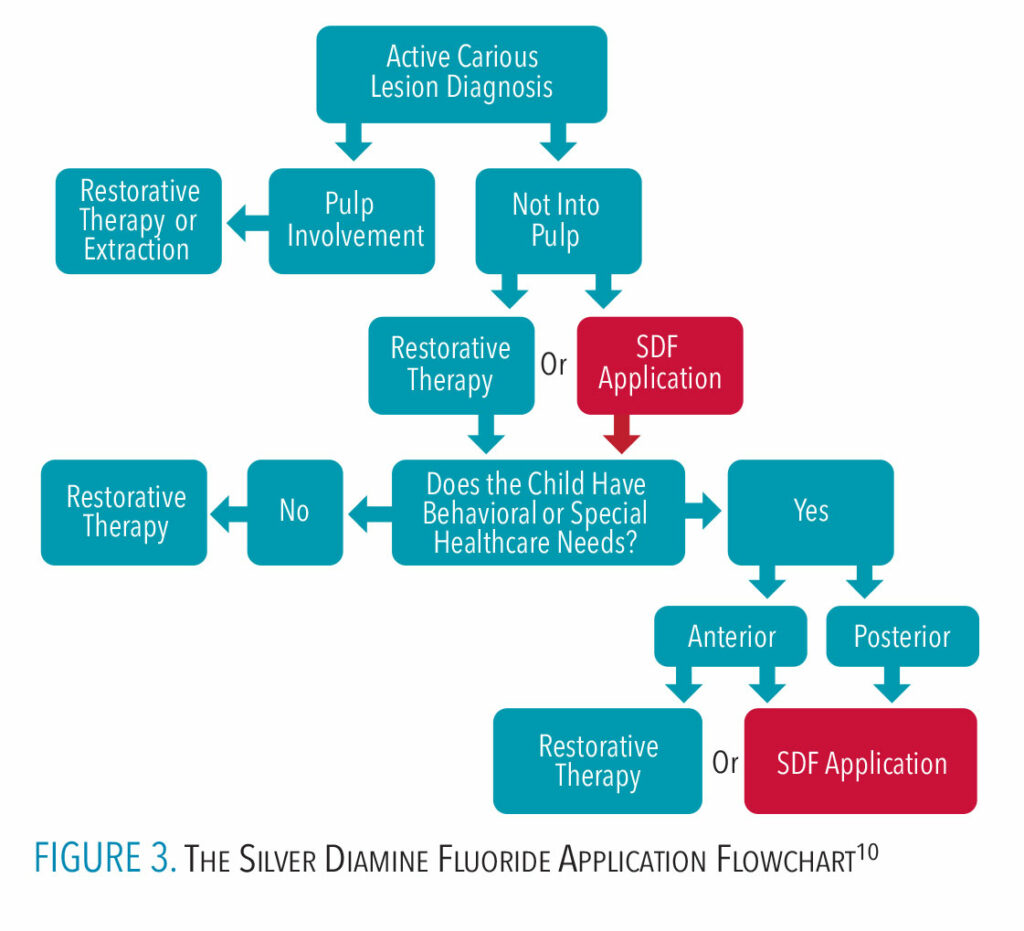 Chairside flowcharts may assist in the clinical decision-making process. The SDF Application Flowchart displays simple options for managing a carious dental lesion with either application of SDF or restorative therapy, while considering individual patient factors (Figure 3). The tool may help increase not only usage but also awareness and knowledge of an alternative therapeutic option. An SDF application flowchart, following AAPD guidelines, can guide the decision-making process during treatment planning.
Chairside flowcharts may assist in the clinical decision-making process. The SDF Application Flowchart displays simple options for managing a carious dental lesion with either application of SDF or restorative therapy, while considering individual patient factors (Figure 3). The tool may help increase not only usage but also awareness and knowledge of an alternative therapeutic option. An SDF application flowchart, following AAPD guidelines, can guide the decision-making process during treatment planning.
Conclusion
In summary, SDF is a safe, effective treatment option for pediatric patients, especially those with special dental care management needs. Evidence suggests that the application process reduces emotional trauma, takes considerably less time than other therapeutic methods, and is accepted by parents/caregivers. The addition of a chairside flowchart for SDF applications may increase SDF usage among oral health professionals thereby improving the standard of dental care for young children and those with special dental care considerations.
References
- Kotha A, Vemulapalli A, Mandapati SR, Aryal S. Prevalence, trends, and severity of early childhood caries in the United States: National Health and Nutritional Examination Survey Data 2013 to 2018. Pediatr Dent. 2022;44:261-268.
- Souza JGS, Souza SE, Noronha MDS, Ferreira EFE, Martins AME. Impact of untreated dental caries on the daily activities of childrenJ J Public Health Dent. 2018;78:197-202.
- Folayan MO, El Tantawi M, Ramos-Gomez F, Sabbah W. Country profile of the epidemiology and clinical management of early childhood caries. Front Public Health. 2020;8:141.
- Contreras V, Toro MJ, Elías-Boneta AR, Encarnación-Burgos A. Effectiveness of silver diamine fluoride in caries prevention and arrest: a systematic literature review. Gen Dent. 2017;65:22-29.
- Zafar S, Boyd D, Siddiqi A. Dental management of a child with autism spectrum disorder and attention-deficit hyperactivity disorder. Oral Health and Dental Management. 2017;16(4):1–7.
- Crystal YO, Niederman R. Evidence-based dentistry update on silver diamine fluoride. Dent Clin North Am. 2019;63:45-68.
- Gao SS, Zhao IS, Hiraishi N, et al. Clinical trials of silver diamine fluoride in arresting caries among children: a systematic review. JDR Clin Transl Res. 2016;1:201-210.
- Kazeminia M, Abdi A, Shohaimi S, et al. Dental caries in primary and permanent teeth in children’s worldwide, 1995 to 2019: a systematic review and meta-analysis. Head Face Med. 2020;16(1):22.
- Burgess JO, Vaghela PM. Silver diamine fluoride: a successful anticarious solution with limits. Adv Dent Res. 2018;29:131-134.
- Crystal YO, Marghalani AA, Ureles SD, et al. Use of silver diamine fluoride for dental caries management in children and adolescents, including those with special health care needs. Pediatr Dent. 2017;39:135-145.
- Ruff RR, Whittemore R, Grochecki M, Bateson J, Barry Godín TJ. Silver diamine fluoride and oral health-related quality of life: A review and network meta-analysis. PloS One. 2022;17:1-11.
- Wakhloo T, Reddy SG, Sharma SK, Chug A, Dixit A, Thakur K. Silver diamine fluoride versus atraumatic restorative treatment in pediatric dental caries management: a systematic review and meta-analysis. J Int Soc Prev Community Dent. 2021;11:367-375.
- Jabin Z, Vishnupriya V, Agarwal N, Nasim I, Jain M, Sharma A. Effect of 38% silver diamine fluoride on control of dental caries in primary dentition: a systematic review. J Fam Med Prim Care. 2020;9:1302-1307.
- Kyoon-Achan G, Schroth RJ, Martin H, et al. Parents’ views on silver diamine fluoride to manage early childhood caries. JDR Clin Transl Res. 2021;6:251-257.
- Roberts A, Bradley J, Merkley S, Pachal T, Gopal JV, Sharma D. Does potassium iodide application following silver diamine fluoride reduce staining of tooth? A systematic review. Aust Dent J. 2020;65:109-117.
- Sabbagh H, Othman M, Khogeer L, Al-Harbi H, Al Harthi A, Abdulgader AAY. Parental acceptance of silver diamine fluoride application on primary dentition: a systematic review and meta-analysis. BMC Oral Health. 2020;20:227.
- Almarwan M, Almawash A, AlBrekan A, Albluwi S. Parental acceptance for the use of silver diamine fluoride on their special health care-needs child’s primary and permanentteeth. Clin Cosmet Investig Dent. 2021;13:195-200.
- Shrivastava U, Barjatya K, Ak BB, et al. Effectiveness and parental perception of silver diamine fluoride toward treatment of dental caries in primary teeth. Int J Clin Pediatr Dent. 2021;14:790-794.
- Vollú AL, Rodrigues GF, Rougemount Teixeira RV, et al. Efficacy of 30% silver diamine fluoride compared to atraumatic restorative treatment on dentine caries arrestment in primary molars of preschool children: a 12-months parallel randomized controlled clinical trial. J Dent. 2019;88:103165.
- Abdellatif HM, Ali AM, Baghdady SI, ElKateb MA. Caries arrest effectiveness of silver diamine fluoride compared to alternative restorative technique: randomized clinical trial. Eur Arch Paediatr Dent. 2021;22:575-585.
From Dimensions of Dental Hygiene. Jan/Feb 2024; 22(1):18-21

