
A Practical Guide to Silver Diamine Fluoride
The use of SDF provides a nonsurgical approach to arresting and managing caries, particularly among high-risk and underserved populations.
This course was issued in January 2020 and expires January 2023. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Discuss the safety and effectiveness of silver diamine fluoride (SDF).
- Identify appropriate patient populations for SDF use.
- Explain the proper technique for SDF application.
Dental caries remains a prevalent and problematic disease to manage, and it disproportionately affects the most vulnerable patient populations. Over the past three decades, conventional approaches to caries prevention and treatment have failed to improve oral health outcomes, while dental care expenditures have increased at rates exceeding inflation.1–3 Our expanding understanding of caries as a recurrent biofilm disease cycle, involving varied states of demineralization and remineralization over a patient’s life span, begs for innovation.4 Silver diamine fluoride (SDF) is an emerging nonsurgical treatment option for caries management. This topical antimicrobial and remineralizing agent is relatively inexpensive and simple to apply, providing an important addition to the caries management care plan.
Safety and Effectiveness
The use of SDF in caries management began with the product’s development in Japan in the 1960s. However, the use of silver nitrate— the precursor to SDF—to treat caries dates back to the mid-1800s. Initially cleared by the United States Food and Drug Administration (FDA) as a device to treat dentinal hypersensitivity in 2014, SDF became commercially available in 2015. In 2016, the FDA designated SDF as a “Breakthrough Therapy” for treating caries. This led to funding by the National Institutes of Health for US-based clinical trials, the outcomes of which will hopefully lead to FDA approval of SDF as a drug to treat caries. Pending these results, using SDF to treat caries is technically “off label” in the US, similar to the use of fluoride varnish, which holds the same FDA clearance. The American Academy of Pediatric Dentistry (AAPD) Council on Clinical Affairs Policy on SDF states, “Off label use for arresting caries is now permissible and appropriate for patients.”5
A 38% SDF solution is 25% silver, 8% ammonia, and 5% fluoride. While the 44,800 ppm fluoride concentration may sound high, the volume used is so small that the actual amount of fluoride is quite low in comparison to other commonly used topical fluorides. For example, one drop (0.05 ml) of SDF contains 2.24 mg of fluoride compared to a conventional 5% unit dose fluoride varnish, which contains 11.3 mg of fluoride.6 A study on the short-term serum pharmacokinetics of SDF found fluoride exposure was below the US Environmental Protection Agency oral reference dose, and while the silver exposure (4.74 mg silver in one drop) exceeded the dose for cumulative daily exposure over a lifetime, its occasional use (typically biannual application) was well below the concentrations associated with toxicity.7 One drop per 10 kg of body weight is considered safe and, depending on the size of the lesion(s), may treat as many as five teeth to six teeth.7 More than one drop can be used at a time. There are no reports of adverse outcomes or known side effects, other than the trademark black stain of active caries, transient metallic taste, and potential gingival irritation, similar to a bleach burn, which resolves on its own in a few days.
 The efficacy of 38% SDF for caries arrest has been well-established in the literature, including 30 clinical trials and 11 systematic reviews. A 2017 systematic review concluded that the use of SDF was 89% more effective in controlling/arresting caries than other treatments or placebos, and the quality of evidence was graded as high.8 A 2018 systematic review with meta-analysis concluded that early 38% SDF applications to exposed root surfaces of older adults were a simple, inexpensive, and effective way of preventing caries initiation and progression.9 The American Dental Association (ADA) and AAPD recently released their first evidence-based clinical practice guidelines, which include recommendations for SDF.10,11
The efficacy of 38% SDF for caries arrest has been well-established in the literature, including 30 clinical trials and 11 systematic reviews. A 2017 systematic review concluded that the use of SDF was 89% more effective in controlling/arresting caries than other treatments or placebos, and the quality of evidence was graded as high.8 A 2018 systematic review with meta-analysis concluded that early 38% SDF applications to exposed root surfaces of older adults were a simple, inexpensive, and effective way of preventing caries initiation and progression.9 The American Dental Association (ADA) and AAPD recently released their first evidence-based clinical practice guidelines, which include recommendations for SDF.10,11
 While SDF is safe and effective, it is not a magical cure-all for caries. SDF is effective at controlling and arresting carious lesions; however, it needs careful follow up and reapplication to maintain arrest. Further, SDF does not restore form or function. As such, SDF is not for every tooth nor for every patient, and about 20% of lesions fail to arrest with SDF treatment alone.
While SDF is safe and effective, it is not a magical cure-all for caries. SDF is effective at controlling and arresting carious lesions; however, it needs careful follow up and reapplication to maintain arrest. Further, SDF does not restore form or function. As such, SDF is not for every tooth nor for every patient, and about 20% of lesions fail to arrest with SDF treatment alone.
Appropriate Patient Populations
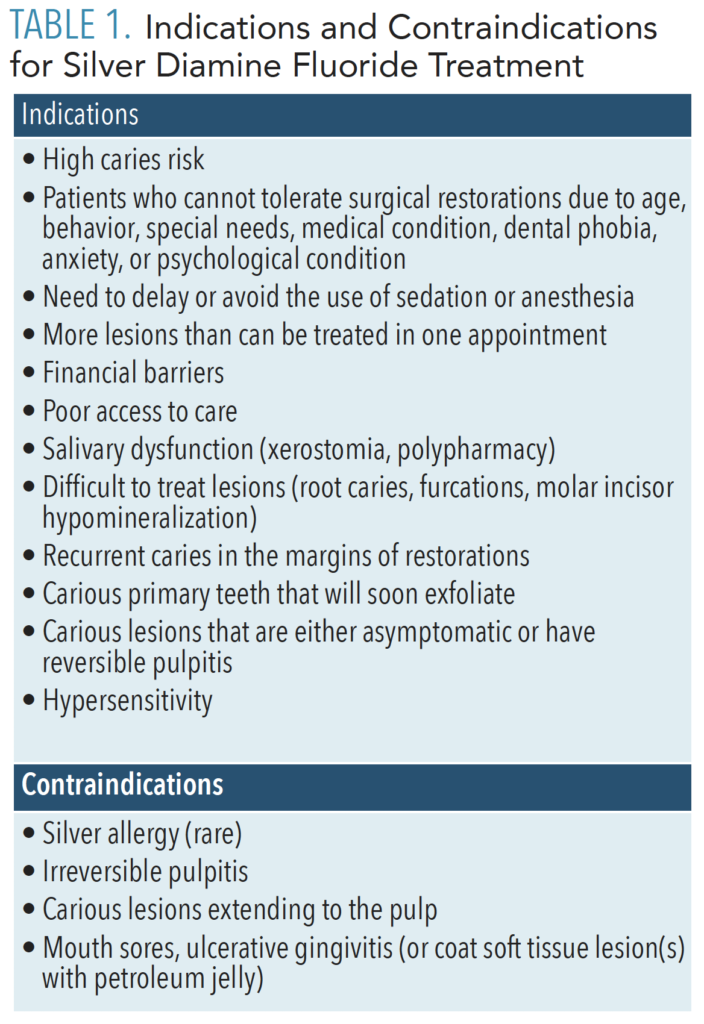
Due to its low cost, simple and painless application technique, and clinical efficacy, SDF is particularly advantageous for the most vulnerable patient populations, including children, older adults, and those covered by government-subsidized dental plans. That being said, patients of any age or health status may benefit from SDF treatment and, if clinically appropriate, should be given the option during the informed consent process. See Table 1 for indications and contraindications for SDF.
Issue of Black Stain/Poor Esthetics
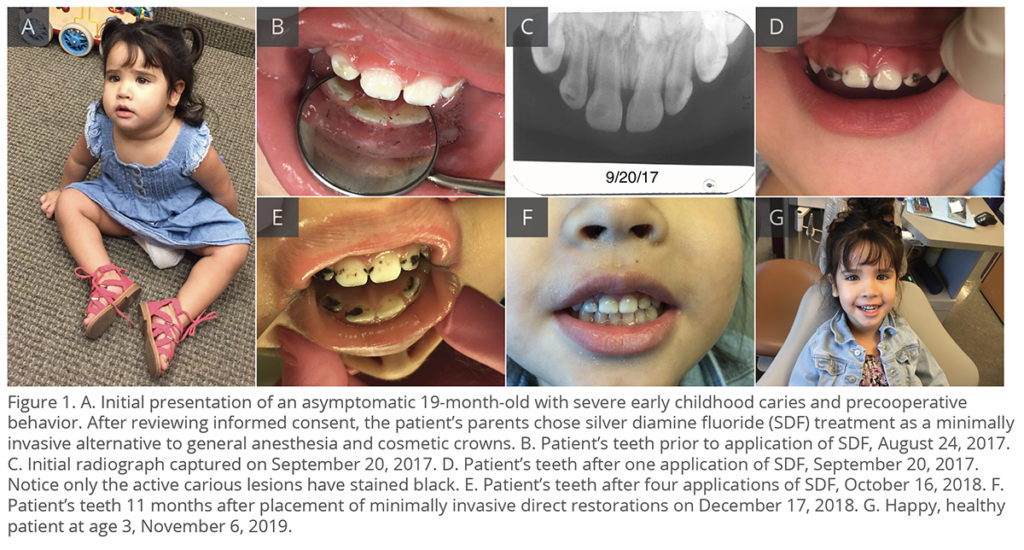
While esthetics is an important part of dentistry, oral health professionals must remember that the main goal is oral health. Due to the indications listed in Table 1, many patients and parents choose SDF, regardless of the risk of black stain.12 Parents tend to prefer SDF treatment in posterior teeth; however, 70% to 76% prefer SDF even for anterior teeth when it presents an alternative to sedation and general anesthesia (Figure 1).13
SDF can stain skin, clothing, and clinic surfaces, so it must be handled with caution. In the mouth, SDF only stains active carious lesions—healthy enamel will not stain. Detecting the activity of lesions can be difficult, therefore SDF must be applied carefully and judiciously. If a noncarious tooth is treated with SDF for sensitivity, there will be no stain.
![]() Scope of Practice
Scope of Practice
SDF is available by prescription only. Delegation of its application to dental auxiliary is subject to individual state dental practice acts. Various states have existing dental practice acts allowing the application of SDF by limited access permit, expanded duties, and independent practice dental hygienists. Dental boards have ruled in favor of dental hygienists applying SDF in Washington, Oregon, Maine, New Mexico, Alaska, Florida, Colorado, New Hampshire, and Montana. Check with your local dental board to see what is permissible in your individual state.
Proper Application Technique
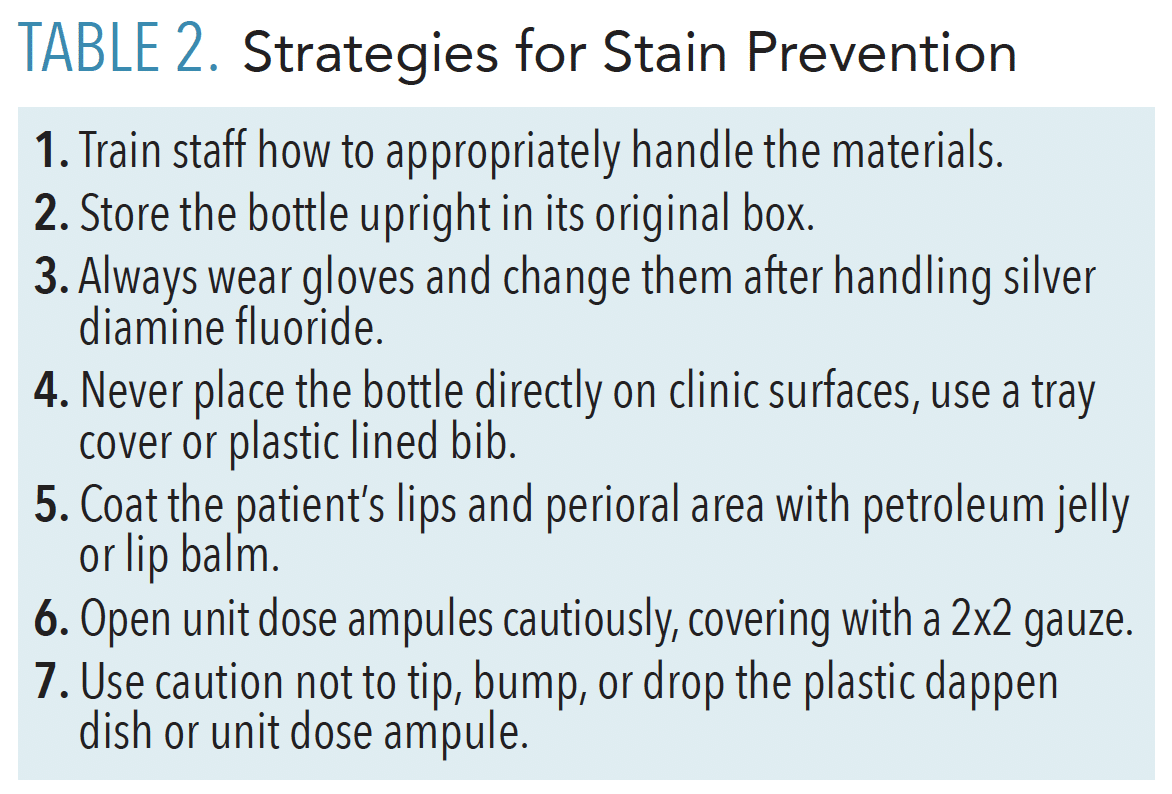
After taking a thorough patient history, including caries risk assessment, diet, and nutritional counseling, a clinical examination is performed, followed by diagnosis, treatment planning, and an informed consent discussion. SDF application is quick and simple, but good technique is integral to achieving favorable outcomes. Table 2 provides strategies for stain prevention.

Following are tips for the basic application of SDF:
- Protective eyewear and a plastic-lined bib are placed on the patient.
- Petroleum jelly is applied to the lips and peri-oral area to prevent inadvertently staining the lips or face with SDF.
- The tooth should be clean and free from food or debris. No caries removal is necessary.
- Isolate with dry-aides and/or cotton rolls.
- Thoroughly dry the tooth with compressed air or, if air is not tolerated, gauze.
- Place one drop of SDF on a plastic dappen dish or open a unit dose vial.
- Dip a microbrush into the SDF and then apply to the tooth for 1 minute to 3 minutes. Fully saturate the lesion and then allow the SDF to absorb via capillary action. Carefully apply only to the desired tooth surface(s) to minimize risk of accidental staining of unintended surfaces. Do not allow SDF to touch the tongue or inflamed tissue, as it may elicit a burning sensation. A gingival barrier or rubber dam is generally not necessary for SDF products with a pH of 10; however, some SDF products have a pH of 13, which could cause a soft tissue burn if used without a barrier.
- DO NOT light cure, rinse, or blow compressed air onto the SDF as it is absorbing.
- After it has absorbed via capillary action for at least 1 minute to 3 minutes, blot the excess SDF with gauze and/or coat the treated site(s) with fluoride varnish. This step is optional, however, it helps improve the patient experience by masking the poor taste and preventing it from reaching other teeth (ie, less accidental stain).
- No eating or drinking restrictions.
When applying SDF to proximal lesions, place woven floss into the contact after the site has been cleaned, isolated, and dried. Using a microbrush, apply SDF to the lingual, buccal, and occlusal aspect of the contact, saturating the floss, and leave it in place for 1 minute to 3 minutes (Figure 2). The floss becomes the delivery system within the contact in lieu of the microbrush. Do not move the floss around, simply leave it in place, and use caution so that the ends do not contact the patient’s lips. After the SDF has absorbed, you may dab any excess pooling SDF with a gauze to prevent splatter. Remove the floss by grabbing both ends and pulling it out of the contact toward the occlusal surface, then cover the treated site with fluoride varnish.
The following steps will help to minimize tooth staining following SDF application.
- Carefully apply to site-specific lesions vs full-mouth application (such as with fluoride varnish)
- Use caution in the esthetic zone. SDF can stain active white spot lesions and restoration margins.
- Do not use the same brush for fluoride varnish application on other teeth that was used to apply SDF. If applying a full-mouth fluoride varnish treatment at the same appointment, consider applying varnish to the other teeth first while the SDF is absorbing, and then coat the SDF-treated site last. If you must apply varnish to the SDF treated site first, replace the contaminated brush before applying varnish to the other teeth.
- Blot the treated lesion with cotton to remove any excess SDF prior to placing varnish or restoration.
- Light-cured restorative materials placed the same day as SDF will immediately turn dark.
- Self-cured restorative materials placed the same day as SDF will eventually turn gray, like a pale amalgam, due to the presence of free silver ions.
- Potassium iodide may reduce initial discoloration, but still produces stain over time and reduces the efficacy of the SDF.14,15
- Opaque restorative materials placed at least 2 weeks after SDF application will stay white.
The following products may help to remove stain produced during SDF application: on the lips and skin, hydrogen peroxide or salt slurry; on operatory surfaces, sodium hypochlorite, Bar Keeper’s Friend, Mr. Clean Magic Eraser, or Comet; and on fabrics, potassium iodide, sodium hypochlorite, or Napisan.
Application Schedule
Clinical trials with biannual application of SDF demonstrated the highest rates of caries arrest. Therefore, at a minimum, the biannual application of SDF is recommended to maintain arrest of unrestored carious lesion. Oral health professionals should use their best clinical judgment to identify which patients would benefit from more frequent follow up and reapplication, such as those patients with extreme caries risk and xerostomia. Conversely, when SDF is applied to manage hypersensitivity, less frequent reapplication may be necessary. A single SDF treatment for hypersensitivity may last a year or beyond, and reapplication can be done on an individualized, as needed basis. Lesions restored following SDF treatment do not need reapplication of SDF, as the SDF is sealed beneath the restoration or crown.
Assessing Outcomes
Assessing the success of an SDF-treated tooth involves a combination of clinical, radiographic, and patient analysis. During the clinical assessment, lesions should appear matte black, like a charcoal briquette and firm. When touched with a sharp explorer, they may feel “sticky,” similar to the feeling of cementum. Soft dentin (the necrotic layer) is incapable of remineralizing and will remain soft.

During the radiographic assessment, the ADA Recommendations for Prescribing Dental Radiographs should be followed. Recare patients with clinical caries or at increased risk for caries should have posterior bitewings at 6-month to 12-month intervals if proximal surfaces cannot be examined visually or with a probe. Clinicians need to note that SDF is radiolucent. Images will demonstrate the stability of the lesion size and any reparative dentin formation. Proximal lesions confined to enamel only may appear more radiopaque over time, as the surface remineralizes.
The patient analysis should include asking him or her the following questions:
- Are the lesions asymptomatic?
- Is your hypersensitivity reduced or eliminated?
- Have contributing factors improved? (diet, hygiene)
- What further treatment needs are warranted/or tolerated at this point?
Using Silver Diamine Fluoride in Deep Carious Lesions
It is unclear whether SDF can be used in deep carious lesions, as this has not been specifically studied. Before placing SDF, the tooth should either be asymptomatic or have reversible pulpitis. Graham Craig, MDS, PhD, who introduced the concept of treating caries with silver fluoride and glass ionomer cement to Australia in the late 1970s, recommends at least 0.5 to 1mm of radiographically sound dentin before using SDF.16 One concern with using SDF in deep lesions is that the components of SDF and/or the pH may irritate the pulp. A histologic study on silver nitrate did find increased severity of inflammation as it came closer to the pulp.17 However, the same results were not found in a histologic study on silver fluoride. Both studies found silver components had reached the pulp, and the latter study hypothesized that the silver component may act on the pulp via direct inactivation/destruction of bacteria in carious dentine and mechanical sealing of carious and sound dentinal tubules when the silver fluoride was followed by atraumatic placement of a glass ionomer cement restoration.18 SDF products with a pH of 10 are equivalent to direct pulp capping materials, such as calcium hydroxide (pH of 10) and mineral trioxide aggregate (pH of 10.2 immediately after mixing, pH of 12.5 3 hours after setting).19
Bond Strength and Need for Restorations
SDF does not adversely affect bond strength of resin or glass ionomer cements or restoratives. These materials can be placed without concern for diminished retention.20–22Another recent study demonstrated increased retention of resin sealants placed on surfaces with prior SDF application.23

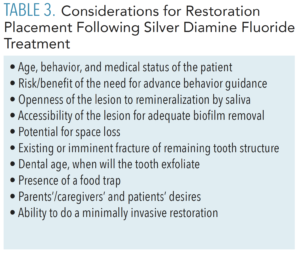
SDF does not restore form or function, it can remineralize, but it does not regenerate missing tooth structure. In order to improve the function, esthetics, and cleansability of the tooth, as well as to prevent further deterioration, fracture, or abscess, certain SDF-treated lesions should be restored, as time, behavior, and finances allow (Figure 3). That being said, not every SDF-treated tooth will need a restoration. Table 3 provides clinical considerations for placing a restoration following SDF treatment for carious lesions.
SDF-arrested lesions can be restored using the principles of minimal intervention dentistry, often without the need for local anesthetic or sedation. Hydrophilic biomimetic materials, such as glass ionomer cement, resin modified glass ionomer, and glass hybrid restoratives, can restore and further remineralize lesions by releasing fluoride and chemically sealing at the margins.24 While beyond the scope of this article, clinicians applying SDF should be knowledgeable regarding these noninvasive techniques: silver modified atraumatic restorative technique, Hall technique, atraumatic restorative treatment, interim therapeutic restoration, and protective restoration.
Coding and Billing
SDF treatment should be documented in the patient record per tooth and by surface(s) treated. The appropriate CDT code is 1354 “Interim Caries Arresting Medicament Application” per tooth. Reimbursement varies. More than 30 state Medicaid plans now cover SDF, as well as a growing number of private insurance plans. Even when not a covered benefit, many patients and parents/caregivers will pay out of pocket for this option. Submit the code to the insurance company, even when SDF is not covered, because this helps drive future coverage by demonstrating the demand. Be sure to carefully review the patient’s description of benefits for reimbursements rates, age and tooth eligibility, frequency allowances, and waiting periods for placing restorations following SDF treatment.
![]() Conclusion
Conclusion
SDF is an important addition to the caries management armamentarium, particularly among high-risk and underserved populations. Oral health professionals need to be well versed in SDF’s indications, side effects, technique, and continuum of care in order to effectively help their patients achieve and maintain oral health.
Acknowledgement
This paper was written in memory of Daisy Lynn.


 Conclusion
Conclusion
