 KATARZYNABIALASIEWICZ/ISTOCK/GETTY IMAGES PLUS
KATARZYNABIALASIEWICZ/ISTOCK/GETTY IMAGES PLUS
Caring for Patients With Diabetes
Oral health professionals can play a role in supporting both the oral and systemic health of patients with diabetes.
This course was published in the April 2018 issue and expires January 2021. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Describe factors contributing to the incidence and prevalence of type 2 diabetes.
- Discuss the common measures of diabetes control and potential systemic and oral signs of poor diabetes control.
- Identify diabetes management strategies.
- Manage diabetes-related medical emergencies in the dental setting.
Between 90% and 95% of all diabetes cases are type 2. Further, approximately 33.9% of US adults have prediabetes, a strong risk factor for type 2 diabetes. This percentage jumps to 48.3% of adults age 65 and older.3 Other type 2 diabetes risk factors include age; family history; race/ethnicity (particularly African American, Latino, Native American, Asian American, and Pacific Islander); past history of gestational diabetes; hypertension; dyslipidemia; cardiovascular disease; polycystic ovary disease; physical inactivity; and obesity.4 Data from the 2013-2014 National Health and Nutrition Examination Survey (NHANES) estimate US obesity rates of 17% in children and adolescents and 37.8% in adults.2 Another population trend in the US is longer life expectancy, contributing to an aging population.1,2 Advancing age and a high prevalence of overweight/obesity increase risks for chronic disease, including diabetes.
DIABETES OVERVIEW
While dietary protein and fat provide energy, glucose is the primary fuel for the brain and red blood cells, making it a crucial energy source.5 Dietary carbohydrates are broken down through digestion into glucose, which travels to the liver and then the bloodstream for distribution. Elevated blood glucose stimulates the release of the hormone insulin from beta cells in the pancreas. Insulin facilitates the conversion of glucose in blood to glycogen for storage in the liver and muscle, and in adipose tissue in the form of fat. When blood glucose drops, the pancreas releases the hormone glucagon to mobilize glucose from the liver and muscle. In this dynamic manner, the body maintains a relatively narrow blood glucose range, storing and mobilizing glucose as needed for energy.6
Diabetes mellitus refers to several metabolic diseases in which the body cannot regulate glucose usage and storage, resulting in elevated blood glucose (hyperglycemia). The body may not produce any or enough insulin to clear glucose from the blood. Alternately, the pancreas may produce sufficient insulin, but cells requiring glucose for energy are resistant to insulin. As a result of any of these processes, cells are starved of energy for normal functioning, despite blood glucose levels remaining elevated.5 The body may respond to this homeostatic imbalance in several ways. Classic symptoms, particularly in type 1 diabetes, are the “three P’s:” polydipsia (increased thirst), polyuria (increased urination), and polyphagia (increased hunger). These symptoms reflect the body’s efforts to simultaneously bring in needed energy and remove excess glucose from the blood via urination. Despite increased appetite, weight loss is common, reflecting the inability to effectively metabolize dietary carbohydrates.6 Polydipsia, polyuria, polyphagia, and unintentional weight change may be reported on the medical history in the dental office and signal the need for further inquiry by the clinician and referral to a primary care provider. Classic symptoms may not be present in all diabetes cases, particularly type 2. Signs and symptoms may develop slowly, including fatigue, frequent infection, slow healing, pain in the extremities, and vision disturbances, while underlying systemic damage occurs.5Assessment and screening for at-risk individuals are crucial for timely diagnosis and management.
Prediabetes and diabetes may be diagnosed based on several blood glucose tests, including fasting plasma glucose (FPG), hemoglobin A1C (HbA1C), or 2-hour post-prandial plasma glucose. Table 1 provides specific diagnostic values. Because of its autoimmune origin, type 1 diabetes diagnosis also includes the presence of autoantibodies.4
Chronic hyperglycemia in poorly controlled diabetes has widespread systemic impact. Excess glucose can abnormally bind to proteins, altering function. Chronic inflammation develops, negatively impacting microvascular actions such as remodeling and perfusion. This microvascular disturbance can compromise immune response, impair wound oxygenation and healing, and damage organs. Low-density lipoprotein cholesterol uptake and atherosclerotic plaque formation can also increase, making diabetes a risk factor for cardiovascular disease.7,8 Nerves are similarly damaged from chronic hyperglycemia, including peripheral nerves of the extremities and autonomic nerves controlling functions. Early symptoms include numbness, tingling, and pain, particularly in the feet. Individuals experiencing neuropathy may not notice injuries or sores, and wound healing may be slow.9 Nerve damage may impact dexterity during oral self-care.

DIABETES AND ORAL HEALTH
Active periodontal disease is thought to impact diabetes control by increasing the body’s inflammatory burden, exacerbating insulin resistance and glucose dysregulation.8 Conversely, poorly controlled diabetes increases the risk for more severe periodontal disease by increasing inflammatory actions throughout the body, compromising immune function and wound healing.7,10 Diabetes may also predispose patients to dental caries, secondary to reduced salivary flow and increased salivary carbohydrate levels.10 Fortunately, therapeutic interventions to achieve periodontal stability can positively affect diabetes. For example, periodontal therapy can reduce both local and systemic inflammation and help improve glycemic control, in turn reducing risk and severity of periodontal disease.8Further, well-controlled diabetes does not increase the risk of periodontitis, reinforcing the oral health benefits of diabetes management.8 Timely oral health interventions and risk management, recare interval adherence, and scrupulous oral hygiene are essential for optimal outcomes.
DIABETES MANAGEMENT
Diabetes treatment includes both medical management and patient self-management. Lifestyle changes alone may restore glycemic control in prediabetes, preventing or delaying progression to type 2 diabetes.11 Physical activity promotes glucose uptake by muscle and improves insulin sensitivity, and exercise programs can improve HbA1C levels in individuals with type 2 diabetes even without significant weight loss.12 Despite various health benefits from regular physical activity, Healthy People 2020 estimates 80% of adults and adolescents do not meet physical activity recommendations for aerobic and strengthening activities.13 Individuals with diabetes should aim to engage in 150 minutes of moderate-to-vigorous intensity aerobic activity weekly with regular resistance exercise.12,13
Dietary modifications, under the guidance of a registered dietitian nutritionist (RDN), are an important part of glycemic control.12Medical nutrition therapy goals may include: weight loss if indicated; seeking high-fiber foods like fruits, vegetables, and whole grains; carbohydrate counting and self-monitoring of blood glucose; incorporating foods containing unsaturated fatty acids; and limiting sodium.12 Oral health professionals should inquire about eating patterns to determine the potential impact on caries risk. For example, small, frequent meals may stabilize blood glucose but increase the total time when teeth are exposed to an acid challenge. As changing this eating pattern may not be feasible, the RDN should determine the patient’s dietary constraints and make recommendations in order for the oral health professional to develop a compatible caries management approach, such as supplemental fluoride therapy, that minimizes the impact of fermentable carbohydrate exposure.
Pharmacotherapy selection for diabetes depends on factors such as diabetes type, disease stability, cost, insurance coverage, and comorbid medical conditions. When lifestyle modifications alone are ineffective, oral medications may be considered to manage type 2 diabetes. These act through a variety of mechanisms, including stimulating insulin release, enhancing cellular sensitivity to insulin, inhibiting carbohydrate digestion, and increasing glucose urinary excretion. The most common classes of oral medications are biguanides and sulfonylureas. Biguanides reduce the liver’s glucose production and heighten muscular sensitivity to insulin.14Sulfonylureas stimulate insulin production by the pancreas.14 Multiple medications may be prescribed if monotherapy is insufficient for glycemic control. Diabetes polypharmacy should alert the clinician to a potentially tenuous control status. Insulin, typically via injection, may also be needed to replace or increase pancreatic insulin production. Although type 1 diabetes requires insulin, it may not be indicated for type 2 diabetes.14 Clinicians should investigate every medication present in a health history, understand the possible dental implications of side effects, and consult with the prescribing physician as needed.15
CARE CONSIDERATIONS
Hyperglycemia drives the damaging effects of diabetes, making glycemic control critical in disease management. Understanding a patient’s glycemic control provides insight into his or her potential response to dental treatment. The level of glycemic control in diabetes is assessed through blood glucose or HbA1C. Self-monitoring of blood glucose (SMBG) informs the patient and treatment team about the status of diet, physical activity, and medication regimen. Frequent SMBG is typically prescribed for patients on insulin due to the greater risk of hypoglycemia compared with oral medications. Testing may be done multiple times per day. Studies have found that more frequent SMBG, and even SMBG among noninsulin-treated patients, has been associated with lower HbA1C levels, suggesting that attention to self-management supports improved glycemic control.16
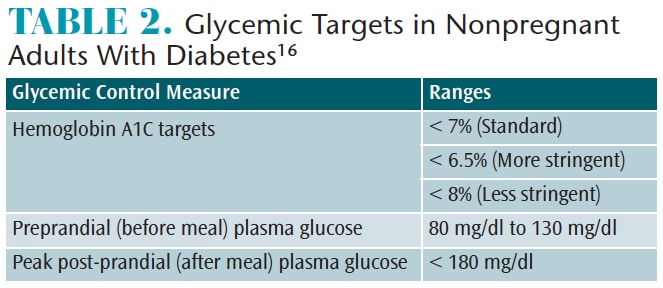
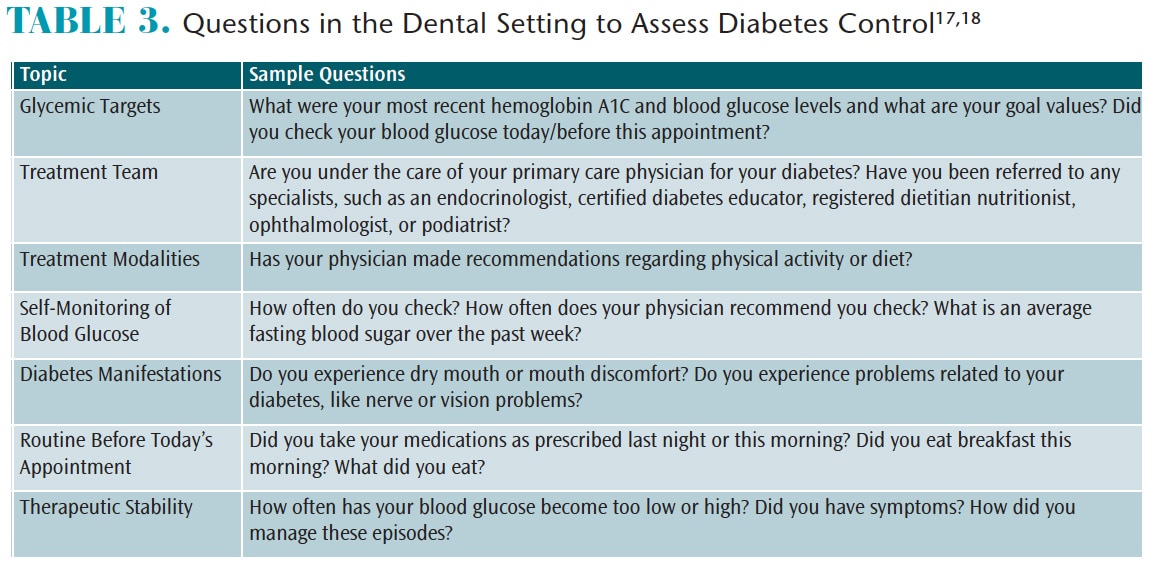
HbA1c reveals longer-term glycemic control in patients with prediabetes and diabetes.4 For nonpregnant adults, a reasonable HbA1c target is less than 7%. A more stringent goal of less than 6.5% may be feasible, such as cases managed solely with lifestyle. Likewise, a less stringent goal of less than 8% may be needed in patients with comorbid conditions or complications.16 Table 2 provides standard glycemic targets. Oral health professionals should be aware of these standards when inquiring about a patient’s glycemic control but must consider that patient targets may vary based on the care team’s determination. Poor glycemic control outside of target ranges is predictive of diabetes complications.4 As immune function and wound healing may be impaired, clinicians should communicate with patients’ physicians regarding potential contraindications to dental procedures or possible need for antibiotic prophylaxis.17,18 Table 3 provides questions clinicians should anticipate asking patients regarding diabetes management and glycemic control.
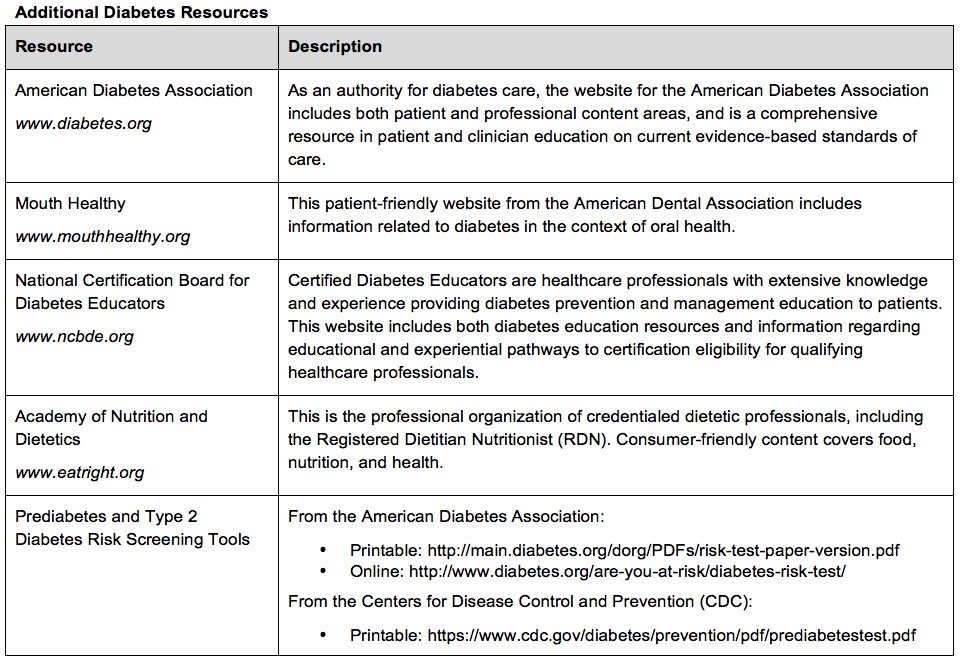
Diabetes may go unrecognized by patients or their health care teams, with subclinical damage occurring before diagnosis. Oral health professionals should be alert to symptoms, such as polydipsia, polyuria, polyphagia, weight changes, and sensation changes in the extremities.6,9 Oral signs and symptoms may also be present, such as xerostomia, candidiasis, burning mouth (secondary to neuropathy), active periodontal disease, tooth loss, and impaired wound healing.10 However, clinicians must consider diabetes risk among asymptomatic patients, as well. Simple risk assessment questionnaires are available from the American Diabetes Association and the CDC to help identify patients at risk for type 2 diabetes and prediabetes. Assessment results can be provided to patients and their primary care physicians for follow-up.19,20 Such screening in the dental office has been found to be predictive of diabetes diagnosis for patients scoring in at-risk levels, reinforcing the value of the dental setting as a screening opportunity.21
Chairside blood glucose testing can confer valuable health information, shaping treatment considerations and potentially mitigating acute medical emergencies. Further, point-of-care finger-prick HbA1C testing in the dental setting, as dictated by state practice regulations, is a 2018 addition to the American Dental Association’s Current Dental Terminology.22
EMERGENCIES
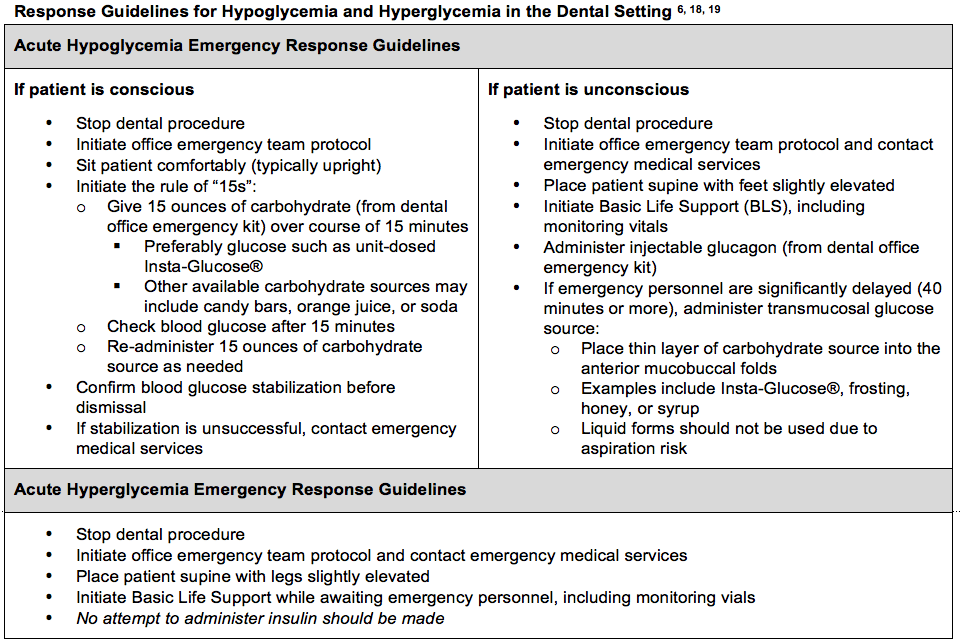
Acute medical emergencies must also be considered when patients with diabetes present for dental appointments. Hypoglycemia is more common than hyperglycemia, but clinicians should be aware of the signs and symptoms, as well as appropriate responses to both. Clinicians who are aware of patients’ diabetes control and current blood glucose measures are best prepared to prevent, mitigate, and address emergencies. The dental team should regularly review its emergency response protocol.
Hypoglycemia, generally corresponding to a blood glucose of 70 mg/dl or less, may be caused by strenuous exercise, decreased food intake, or excess medication dosing.6,17 Signs of hypoglycemia can develop rapidly, including cold sweat, shakiness, anxiety, irritability, hunger, lightheadedness, and poor motor coordination, potentially progressing to bizarre behavior, seizures, and loss of consciousness.17 While many patients recognize the onset of hypoglycemia, others may not, so clinicians must be alert to such changes and be prepared to respond. Unless there are other obvious causes, an unconscious patient with diabetes should be presumed hypoglycemic. Risk of death is much more rapid in hypoglycemia than hyperglycemia, and erroneous glucose administration to a hyperglycemic patient will not significantly impact the event.17
Hyperglycemia can occur when the body’s demand for insulin increases, such as from infection; illness; therapy noncompliance; secondary diseases, such as myocardial infarction; stress; corticosteroid therapy; and hyperthyroidism. Diabetic ketoacidosis (DKA) and hyperglycemic hyperosmolar state (HHS) can cause unregulated hyperglycemia, with infection being the most common precipitating factor for both.23 DKA is most common in individuals with type 1 diabetes and may develop in less than 24 hours, with symptoms including classic polydipsia, polyuria, and polyphagia, as well as headache, fatigue, abdominal pain, nausea, vomiting, blurred vision, and mental confusion.23 Clinically, the patient may present with hot, dry, flushed skin, tachycardia, hypotension, and hyperventilation. Unable to use glucose in the blood, fat is broken down and metabolized for energy. Ketones, a byproduct of this metabolism, produce a fruity, acetone scent to the breath, possibly detectable during an appointment. Symptoms of hyperglycemia and DKA may progress to a state of unconsciousness called diabetic coma.17
In patients with type 2 diabetes who produce some insulin, hyperglycemia is more likely to progress to HHS. Particularly prevalent in older adults, HHS may even present in previously undiagnosed cases. Symptoms are similar to DKA, such as polydipsia, polyuria, and polyphagia, progressing to motor impairment, altered mental state, and coma, but HHS develops over days or weeks, and ketoacidosis from fat breakdown is generally absent. Severe and potentially life-threatening dehydration occurs as the body tries to excrete glucose through urination, while blood becomes excessively concentrated.23
CONCLUSION
Oral health professionals need to be knowledgeable about diabetes and comfortable assessing patients’ diabetes control or risk through careful health history, interview, and blood glucose testing. Validated screening tools and point-of-care diabetes testing can support timely diagnosis and intervention. Poorly controlled diabetes can negatively impact outcomes and safety, so assessment of glycemic control is essential. As members of the interprofessional care team, oral health professionals are well-poised to educate patients about the relationship between oral health and diabetes to support positive health behavior and treatment compliance.
REFERENCES
- World Health Organization. Global Report on Diabetes. Available at: who.int/diabetes/global-report/en/. Accessed March 20, 2018.
- National Center for Health Statistics. Health, United States, 2016: With Chartbook on Long-Term Trends in Health. Available at: cdc.gov/nchs/data/hus/hus16.pdf. Accessed March 20, 2018.
- United States Centers for Disease Control and Prevention. National Diabetes Statistics Report, 2017. Available at: cdc.gov/diabetes/pdfs/data/statistics/national-diabetes-statistics-report.pdf. Accessed March 20, 2018.
- American Diabetes Association. 2. Classification and diagnosis of diabetes: standards of medical care in diabetes—2018. Diabetes Care. 2018;41(Suppl 1):S13–S27.
- Sizer FS, Whitney E. Nutrition: Concepts and Controversies. 13th ed. Belmont, California: Wadsworth; 2014;113–141.
- Palmer C, Boyd L. Diet and Nutrition in Oral Health. 3rd ed. Upper Saddle River, New Jersey: Pearson Prentice Hall; 2016; 57–86.
- Kolluru GK, Bir SC, Kevil CG. Endothelial dysfunction and diabetes: Effects on angiogenesis, vascular remodeling, and wound healing. Int J Vasc Med. 2012;918267:30.
- Mealy BL, Oates TW. Diabetes mellitus and periodontal diseases. J Periodontol. 2006;77:1289–1303.
- National Institute of Diabetes and Digestive and Kidney Diseases. Nerve Damage (Diabetic Neuropathies). Available at: niddk.nih.gov/health-information/diabetes/overview/preventing-problems/nerve-damage-diabetic-neuropathies. Accessed March 20, 2018.
- Leite RS, Marlow NM, Fernandes JK. Oral health and type 2 diabetes. Am J Med Sci. 2013;345:271–273.
- American Diabetes Association. 5. Prevention or delay of type 2 diabetes: Standards of medical care in diabetes—2018. Diabetes Care. 2018;41(Suppl 1):S51–S54.
- American Diabetes Association. 4. Lifestyle management: Standards of medical care in diabetes—2018. Diabetes Care. 2018;41(Suppl 1):S38–S50.
- US Office of Disease Prevention and Health Promotion. Healthy People 2020. Available at: healthypeople.gov/2020/topics-objectives/topic/physical-activity. Accessed March 20, 2018.
- American Diabetes Association. 8. Pharmacologic approaches to glycemic treatment: standards of medical care in diabetes—2018. Diabetes Care. 2018;41(Suppl 1):S73–S85.
- Wolters Kluwer. Lexicomp Online for Dentistry. Available at: wolterskluwercdi.com/online-for-dentistry/. Accessed March 20, 2018.
- American Diabetes Association. 6. Glycemic targets: standards of medical care in diabetes—2018. Diabetes Care.2018;41(Suppl 1):S55–S64.
- Malamed S. Medical Emergencies in the Dental Office. 7th ed. St. Louis: Elsevier; 2015:261–277.
- American Dental Association. Oral Health Topics: Diabetes. Available at ada.org/en/member-center/oral-health-topics/diabetes. Accessed March 20, 2018.
- American Diabetes Association. Type 2 Diabetes Risk Test. Available at: main.diabetes.org/dorg/PDFs/risk-test-paper-version.pdf. Accessed March 20, 2018.
- US Centers for Disease Control and Prevention. CDC Prediabetes Screening Test. Available at: cdc.gov/diabetes/prevention/pdf/prediabetestest.pdf. Accessed March 20, 2018.
- Herman WH, Taylor GW, Jacobson JJ, Burke R, Brown MB. Screening for prediabetes and type 2 diabetes in dental offices. J Public Health Dent. 2015;75:175–182.
- American Dental Association. D0411—ADA Guide to Point of Care Diabetes Testing and Reporting. Available at: ada.org/~/media/ADA/Publications/Files/D0411_ADAGuidetoPointofCareDiabeteTestingandReporting_v1_2017Jul17.pdf?la=en. Accessed March 20, 2018.
- Umpierrez GE, Murphy MB, Kitabchi AE. Diabetic ketoacidosis and hyperglycemic hyperosmolar syndrome. Diabetes Spectrum. 2002;15:28–36.
From Dimensions of Dental Hygiene. April 2018;16(4):40-43.



