
Achieve Success in Esthetic and Functional Crown Lengthening
A clear grasp of the biology of the periodontal/restorative interface improves the outcomes of crown lengthening procedures.
This course was published in the March 2022 issue and expires March 2025. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Explain indications for crown lengthening and the clinical benefits of these procedures.
- Describe etiologies and conditions that may lead to recommendations for crown lengthening, as well as tooth proportions and similar determinants affecting treatment.
- Discuss treatment planning and other considerations related to crown lengthening surgery.
Complex restorative situations often require an interdisciplinary approach to diagnosis and treatment. The predictability of tooth-borne restorations is based on a healthy, biologic foundation. The relationship of the hard and soft tissues must be upheld to preserve the dimensions of tissue and epithelial attachments around teeth; namely, the supracrestal attached tissues (formerly biologic width).1 Crown lengthening procedures can provide both functional and esthetic benefits to natural and restored teeth, and help create facial harmony. The surgical workflow largely depends on the appropriate diagnosis and restorative plan. Otherwise, the original gingival apparatus simply reestablishes itself—or, worse, breaks down in light of supracrestal attached tissue impingement. Learning to properly identify and treat crown lengthening cases can improve long-term health and patient outcomes.
During active eruption, the tooth emerges into the oral cavity and coronally advances until it meets its antagonist. Then, passive eruption begins, as the secondary epithelial attachment splits and recedes apically to establish a new dentogingival junction.2 Ideally, the supracrestal tissue attachment includes 1.07 mm of connective tissue, and 0.97 mm of junctional epithelium, with a sulcus depth of 0.69 mm.3
However, tooth eruption does not always create the right biologic dimensions, leading to the appearance of thick, fibrotic gingiva and short clinical crowns. The failure of the free gingival margin to migrate past the cervical convexity of the crown is known as altered passive eruption (APE). Occlusal interferences during active eruption, thick, flat phenotypes, genetic predisposition, and orthodontic and endodontic trauma have been proposed etiologies.2 Clinically, APE presents in 12% of the population. There is a statistically significant association between gingival phenotype and prevalence of APE, with a greater prevalence in those with a thick, flat gingival phenotype.4 The anatomical difference can predispose the sulcus to anaerobic bacteria and limit hygienic and restorative access.5
These processes can also affect tooth proportions. The widest and longest crowns are typically the central incisors, measuring from 9.10 mm to 9.24 mm and 11.69 mm, respectively, with width-to-length ratios of 78%. Lateral incisors and canines have similar findings at about 73%. These ratios vary significantly between worn and unworn teeth and also by gender.6 Furthermore, when viewed from the front, the central-to-lateral incisor width and lateral incisor-to-canine width should both be around 62%. This is desirable for facial esthetics and symmetry.7 It is important to measure tooth length as part of the initial workup. The appearance of short clinical crowns could also be a result of dentoalveolar extrusion or wear, lending to a more complex interdisciplinary approach to treatment.

Periodontal phenotype is an important determinant in the treatment of excessive gingival display. It is the combination of gingival thickness, keratinized tissue width, and thickness of the buccal plate.8 A thin phenotype is classified when the periodontal probe can be visualized through the facial gingival sulcus. Thin, scalloped phenotypes are often the most difficult to treat, as they can present as risk factors for marginal recession.9 A quick assessment of a patient’s phenotype can help anticipate challenges in long-term maintenance.

Treatment Planning
Indications for crown lengthening include caries or tooth fracture at or below the gingival margin, teeth with excessive occlusal loss, teeth with insufficient interocclusal space for a required restorative procedure, and APE. The treatment plan is predicated on the diagnosis and goals of definitive therapy.10
Esthetic crown lengthening or anatomical crown exposure aims to provide the correct dentogingival relationship in cases of APE or gingival enlargement. Such procedures may or may not include osseous resection, and are usually limited to the facial surface of the teeth involved. The appearance of short clinical crowns can lead to the suspicion of APE. Clinical evaluation is performed with the aid of an explorer to identify the presence or absence of an intrasulcular cementoenamel junction (CEJ). The CEJ should be located at the level of the gingival margin or in the dental sulcus. The inability to identify the CEJ on short clinical crowns leads to a diagnosis of APE.11
Functional crown lengthening improves restorative access by exposing more tooth structure for a prosthesis. This procedure always requires osseous resection, which is usually performed circumferentially. Commonly accepted crown preparation guidelines include a minimal occlusocervical dimension of 4 mm for molars, and 3 mm for other teeth.12 The occlusocervical-to-faciolingual dimensional ratio should be at least 0.4 for the preparation to provide adequate resistance and retention form. These dimensions are used as a guideline when reestablishing the coronal tooth structure necessary to enable the restoration of a compromised tooth. When possible, a supragingival finish line is preferred, and subgingival finish lines should not extend into the epithelial attachment.12

Prior to proceeding with any crown lengthening procedure, a restorative plan should be determined. In cases involving the maxillary anterior teeth, restorative treatment plans should consider esthetic guidelines. The location of anterior teeth in space can be broken down into their vertical and horizontal position. The vertical position of anterior teeth is guided by the desired amount of tooth display at rest. Maxillary anterior tooth display at repose tends to decrease with age. The average 30- to 39-year-old shows around 1.5 mm of the maxillary central incisors, and this value decreases around 0.5 mm each decade.13 These dimensions help determine age-appropriate display of the anterior teeth. Phonetics and esthetics guide the horizontal position of these teeth. Once these positions are determined, it is clinically desirable for the incisal edges to parallel the lower lip line (also known as the smile line).7
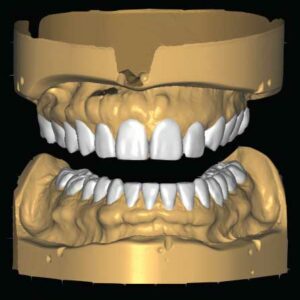
Definitive restoration contours may be modeled using an analog or digital approach. An analog approach requires maxillary and mandibular diagnostic casts mounted in either centric relation or maximum intercuspation, depending on whether the restorative treatment is conformative or rehabilitative. A digital approach requires a surface scan of the maxillary and mandibular dentition and design software. Prior to proceeding with surgical treatment, the proposed restorative contours should be modeled intraorally. This offers both the provider and patient an opportunity to make modifications to the treatment plan prior to providing care that is irreversible. The location and contours of the definitive restorations will determine the desired location of the gingival margins.
Principles of Crown Lengthening Surgery

Surgical treatment largely depends on the underlying etiology. Coslet et al14 identified multiple types and subcategories for APE based on gingival thickness and crestal bone position. Type 1 has normal keratinized tissue width, while Type 2 has a narrow, but acceptable, band of buccal attached, keratinized tissue. In the A subgroup, the osseous crest is 1.5 to 2 mm below the CEJ (normal), while in the B subgroup, the osseous crest is at the CEJ.14 The different relations of the hard and soft tissues can alter the surgical plan. For example, patients presenting with Type 1B would benefit most from gingivectomy and osseous reduction to reestablish the appropriate biologic dimensions (where there is both excess gingival tissue and bone). Conversely, caution should be taken in treating Type 2B, where flap margins should simply be apically repositioned to minimize any mucogingival defects with tissue resection.
Certain principles are universal for esthetic and functional crown lengthening procedures. For example, an average of 1 mm of bone is removed during osseous-related surgery and generally stabilizes by six months.15 During healing, 0.54 mm of bone is generally lost, with thinner bone resorbing more quickly.16 While the desired distance from the planned restorative margin to crestal bone is 3 mm, the mean distance achieved by most clinicians is 2.4 + 1.4 mm. More experienced surgeons may remove larger amounts of bone, with generally greater osseous reduction on the buccal and mesial aspects.17
Flap management can affect short- and long-term healing. Newer evidence shows that flaps replaced less than 3 mm from bone after conventional osseous surgery were stable at six months 93% of the time. There is a linear relation between final flap margin position and posttreatment tissue rebound.18 Furthermore, dentists should wait at least six months after crown lengthening in the esthetic zone to finalize the prosthesis because 12% of treated sites exhibit anywhere from 2 to 4 mm recession. Soft tissue rebound can also still occur during initial healing. Provisionalization during this healing period can therefore help guide marginal tissue stability.19

Case Report
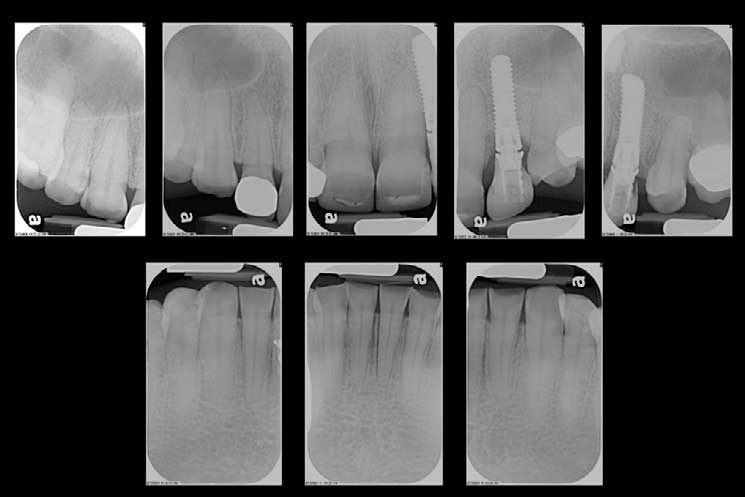
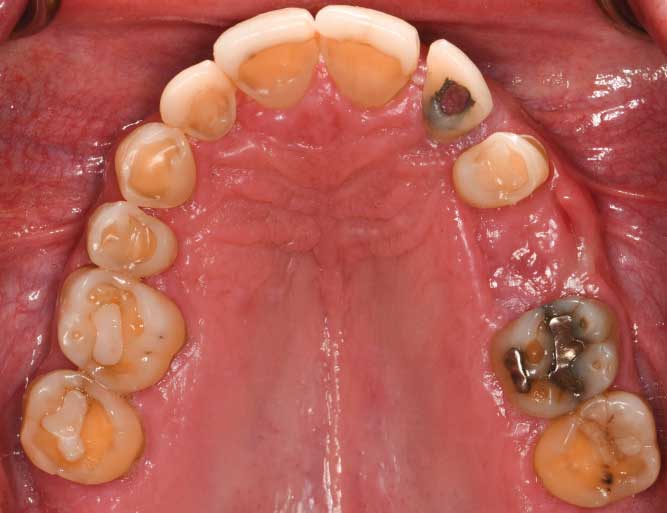
The following case illustrates crown lengthening treatment of the maxillary and mandibular dentition (Figure 1, beginning on page 42, through Figure 12). A 52-year-old man presented to the graduate prosthodontics clinic at the University of Texas Health Science Center at San Antonio School of Dentistry interested in an implant- and tooth-supported full-mouth rehabilitation. He had a medical history of hypertension, type 2 diabetes mellitus, hypercholesterolemia, and anxiety. He presented with severe erosion of the palatal surfaces of the maxillary dentition, localized severe attrition, and localized moderate abrasion. The patient was classified as a Turner Category 3 (ie, excessive wear without loss of occlusal vertical dimension, with limited restorative space). He had excessive gingival display at full animation secondary to a hyperactive upper lip.
After a thorough examination, a comprehensive treatment plan was developed, and the patient was referred to the graduate periodontics clinic. Surgical procedures were performed using intravenous conscious sedation. The treatment plan included:
- Virtual wax-up of the definitive contours of the maxillary and mandibular teeth
- Maxillary and mandibular functional crown lengthening, with extractions of retained primary tooth #J and 19, and site development for future implant placement
- Delayed implant placement at sites #13 and 19
- Implant- and tooth-supported prostheses for the maxillary and mandibular dentition

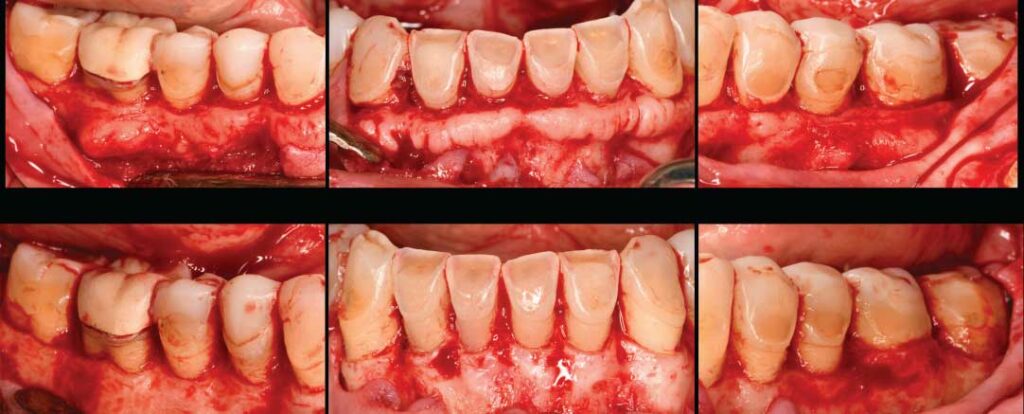
Surgical therapy was performed to establish the coronal tooth structure required to restore worn dentition with full-coverage restorations. A surgical guide delineating the desired final position of the gingival margins was provided by the restorative dentist and used intraoperatively. Functional crown lengthening was performed in all four quadrants to achieve proper tooth dimensions for the provisional and definitive prostheses. Teeth #J and 19 were extracted, and ridge preservation was performed to prepare for future implant placement.

Post-operative instructions were reviewed. The patient returned for follow-up at 2 weeks, 1 month, and 2 months. The final marginal position allows for improved hygiene and restorative access. If functional crown lengthening was not successfully performed, crown preparations would lack proper retention and resistance forms and extend apically to bone, damaging the gingival complex. Future implants would have also been placed too shallow, given the tight interdental space at initial presentation. The patient will continue restorative care and yearly recare appointments at the graduate prosthodontics clinic.
Summary and Conclusions
Clinically, treatment planning predicated on a basic understanding of the biologic influences on the periodontal/restorative interface can provide lasting results. Identifying the correct, underlying etiology for the patient’s initial presentation will dictate surgical and restorative treatment. As part of this effort, the relationship of the hard and soft tissues must be respected to prevent the dentogingival complex from breaking over time. When managed successfully, esthetic and functional crown lengthening procedures can transform the smile and facial profile. As demonstrated by the clinical report presented here, an interdisciplinary team can outline proper workflows and navigate challenges in cases requiring surgical crown lengthening.

Acknowledgment: The authors thank Neda AlMojel, BDS, MS, and Brandon M. Wilburn, DMD, residents in the graduate prosthodontics program at the University of Texas Health Science Center at San Antonio School of Dentistry, for completing the initial restorative evaluation, digital wax-up of the proposed restorations, and treatment plan.
References
- Caton JG, Armitage G, Berglundh T, et al. A new classification scheme for periodontal and peri-implant diseases and conditions—Introduction and key changes from the 1999 classification. J Periodontol. 2018;89(Suppl 1):S1–S8.
- Goldman HM, Cohen DW. Periodontal Therapy. 4th ed. St. Louis: Mosby; 1968.
- Gargiulo A, Wentz FM, Orban B. Dimensions and relations of the dentogingival junction in humans. J Periodontol. 1961;32:261–267.
- Nart J, Carrio N, Valles C, et al. Prevalence of altered passive eruption in orthodontically treated and untreated patients. J Periodontol. 2014;85:e348–e353.
- Volchansky A, Cleaton-Jones PE. Delayed passive eruption. A predisposing factor to Vincent´s infection? J Dent Asso S Africa. 1974;29:291–294.
- Magne P, Gallucci GO, Belser UC. Anatomic crown width/length ratios of unworn and worn maxillary teeth in white subjects. J Prosthet Dent. 2003;89:453–461.
- Lombardi RE. The principles of visual perception and their clinical application to denture esthetics. J Prosthet Dent. 1973;29:358–382.
- Jepsen S, Caton JG, Albandar JM, et al. Periodontal manifestations of systemic disease and developmental and acquired conditions: Consensus report of workgroup 3 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Disease and Conditions. J Periodontol. 2018;89(Suppl 1):S237–S248.
- De Rouck T, Eghbali R, Collys K, De Bruyn H, Cosyn J. The gingival biotype revisited: transparency of the periodontal probe through the gingival margin as a method to discriminate thin from thick gingiva. J Clin Periodontol. 2009;36:428–433.
- Rosenberg ES, Garber DA, Evian CI. Tooth lengthening procedures. Compend Contin Educ Gen Dent. 1980;1:161–172.
- Dolt AH, Robbins JW. Altered passive eruption: an etiology of short clinical crowns. Quintessence Int. 1997;28:262–272.
- Goodacre CJ, Campagni WV, Aquilino SA. Tooth preparations for complete crowns: an art form based on scientific principles. J Prosthet Dent. 2001;85:363–376.
- Vig RG, Brundo GC. The kinetics of anterior tooth display. J Prosthet Dent. 1978;39:502–504.
- Coslet JG, Vanarsdall R, Weisgold A. Diagnosis and classification of delayed passive eruption of the dentogingival junction in the adult. Alpha Omegan. 1977;7:24–28.
- Pontoriero R, Carnevale G. Surgical crown lengthening: a 12-month clinical wound healing study. J Periodontol. 2001;72:841–848.
- Pennel BM, King KO, Wilderman MN, Barron JM. Repair of the alveolar process following osseous surgery. J Periodontol. 1967;38:426–431.
- Herrero F, Scott JB, Maropis PS, Yukna RA. Clinical comparison of desired versus actual amount of surgical crown lengthening. J Periodontol. 1995;66:568–571.
- Penner JK, Deas DE, Mills MP, et al. Post-surgical flap placement following osseous surgery: A short-term clinical evaluation. J Periodontol. 2020;91:501–507.
- Brägger U, Lauchenauer D, Lang NP. Surgical lengthening of the clinical crown. J Clin Periodontol. 1992;19:58–63.
From Dimensions of Dental Hygiene. March 2022;20(3):42-45.



