
A Closer Look at Gingival Recession
While not every case of recession requires treatment, evaluating etiology and precipitating factors will help clinicians determine the need for a therapeutic solution.
This course was published in the July 2017 issue and expires July 2020. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Discuss the percentage of patients presenting with gingival recession and explain the importance of determining etiology.
- Describe systems for categorizing various factors associated with gingival recession.
- Explain why patients seek treatment for gingival recession and name management strategies and possible interventions.
Gingival recession is associated with oral exposure of the root surface due to a displacement of the gingival margin apical to the cementoenamel junction.1 This is a fairly common clinical condition, and research indicates it presents in at least one or more tooth surfaces in 23% of United States adults between the ages of 30 and 90.2 According to the classification system developed by the American Academy of Periodontology (AAP), mucogingival deformities and conditions around teeth and edentulous ridges include gingival/mucosal tissue recession, lack of keratinized gingiva, decreased vestibular depth, aberrant frenal pull/muscle position, gingival excess, and abnormal color.3 While this article will focus on key aspects of gingival recession, it will not discuss decreased vestibular depth, gingival excess, or abnormal color.
Successful correction of mucogingival conditions requires a thorough understanding of the etiology of gingival recession, because treating this condition without addressing the underlying cause may compromise outcomes.
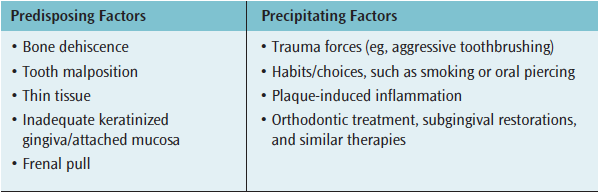
The etiology of gingival recession is often multifactorial. Chan et al4 categorize the etiological factors of gingival recession under predisposing factors and precipitating factors (Table 1). Although predisposing factors are mainly linked to anatomical factors—such as presence of underlying bone and thickness of the gingival biotype—inflammation can also be implicated. Additional anatomical predisposing factors include frenal pull (Figure 1) and a lack of adequate keratinized gingiva.5 Studies comparing sites with insufficient attached mucosa noted that attachment loss or recession did not progress over time.6 However, in a recent meta-analysis evaluating 1,647 sites of buccal gingival recession, 78.1% experienced a progression in gingival recession at follow up (≥ 24 months).7 Pooled estimates showed increased odds of recession developing long term (odds ratio 2.43; p=0.03) or number of sites with gingival recession (odds ratio 2.16; p=0.0005). The authors concluded that untreated gingival recession has a high probability of progressing, even in the presence of optimal self-care.7 Figure 2 demonstrates the progression of gingival recession without treatment.

PRECIPITATING FACTORS
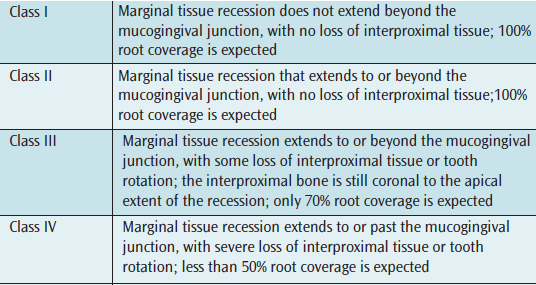
Although lack of oral hygiene and subsequent inflammation are precipitating factors in gingival recession, overzealous oral hygiene can also negatively impact gingiva. The results of traumatic toothbrushing most commonly present as recession on the facial of teeth prominent in the arch.4 Figure 3 illustrates gingival recession as a result of aggressive brushing. Recession is noted primarily on the left maxillary canine and premolars, as well as the mandibular canines. In evaluating the effects of brushing, the factors that positively correlated with gingival recession include frequency, duration, using a horizontal or scrub method, bristle hardness, and frequency of changing a toothbrush.8 Generalized remodeling of the gingival tissue as a result of periodontitis and/or tooth extraction is also a factor. Other precipitating factors include tobacco chewing and oral piercing. Orthodontic therapy has long been debated as a precipitating factor, but a systematic review suggests incidence of gingival recession is < 10% in patients undergoing orthodontic treatment.9 When gingival recession is noted with orthodontic therapy, it tends to be treatable if identified early.4
INDICATIONS FOR TREATMENT
While there are several indications for treatment of gingival recession, esthetics are a primary indication, according to Cairo et al.10 In a recent literature review, Chan et al4 analyzed search results and identified factors that influence the decision to treat gingival recession. The following is a description of these factors, along with other considerations that affect treatment planning:

Classification of Recession Defect. Miller11 classified gingival recession based on severity (Table 2). A Miller’s class I or II recession has good predictability in terms of root coverage, whereas minimal coverage is expected in the case of a Miller’s class III or IV defect. Soft-tissue grafting in areas with a Miller’s class III or IV recession is mainly intended to increase the zone of keratinized gingiva and/or increase the thickness of the gingiva. Figure 4 through Figure 7 illustrate various Miller classifications.

Patient Concerns. Unsatisfactory esthetics is a major reason why patients with gingival recession seek treatment. Hypersensitivity is another chief concern, and it has been shown to be significantly reduced following root coverage procedures.4,12 In some cases, however, a complete resolution of root sensitivity may require additional treatment, such as a Class V restoration. In areas of root sensitivity with minimal gingival recession, nonsurgical treatment should be explored before surgical root coverage is presented as an option. Figure 8 illustrates generalized gingival recession in a patient who presented with esthetics as a chief complaint.
Progression of Defect. Recession that shows progression without surgical intervention usually requires surgical treatment to regain lost attachment and halt further progression. As previously noted, 78.1% of sites with untreated buccal gingival recession demonstrated progression.7
Restorative or Orthodontic Needs. Evidence suggests that maintaining a band of keratinized gingiva around restorations with intracrevicular margins results in healthier tissue.13 While appropriately applied orthodontic forces do not cause permanent damage to the periodontium, the risk for recession is high with facial or lingual tooth movement in a periodontium with a thin gingival biotype. As a result, gingival augmentation is often recommended in areas of thin gingival biotype or when orthodontic therapy is likely to move the tooth outside the alveolar housing.13 Patients undergoing orthodontic therapy should be closely monitored for signs of recession, and may need surgical intervention before, during, or after treatment. The risk of recession in these cases is higher if other risk factors are present, such as a high plaque score or thin gingival biotype.


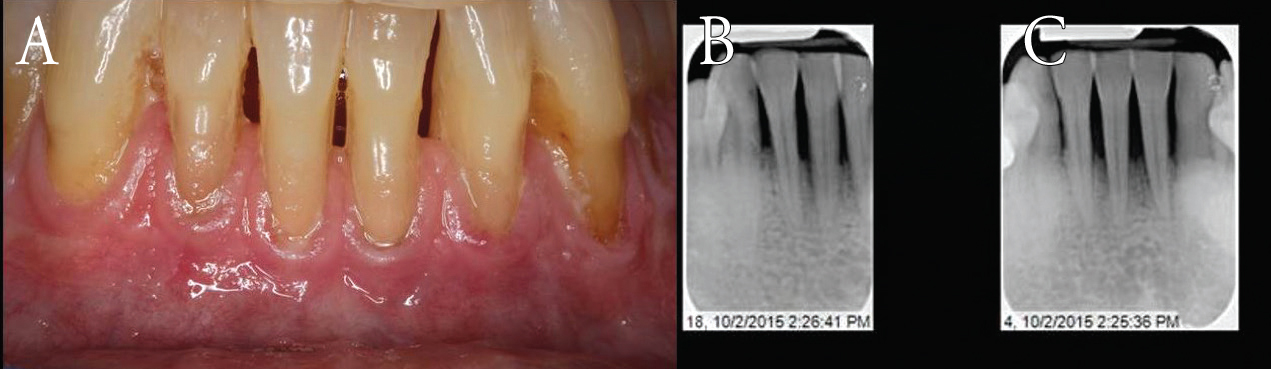
Areas featuring a lack of keratinized gingiva can be difficult to clean, leading to biofilm accumulation.5,13 Such accumulation promotes inflammation that could potentially cause the recession to progress. Oral health professionals should educate patients about the need for optimal oral hygiene, and consider treatment to increase the zone of keratinized gingiva. Figure 9 illustrates significant gingival inflammation in the area of teeth #24 and #25 as a result of biofilm accumulation. The area lacks keratinized gingiva, which made oral self-care challenging.

DENTAL IMPLANTS
Expanding on early successes in osseointegration, the focus in implantology today is shifting to more esthetic outcomes.14 Dental implants and implant restorations in the esthetic zone must mimic natural tooth characteristics and exhibit a soft-tissue profile that offers the appearance of a natural tooth exiting from the gingiva. Successful implants in the esthetic zone are made possible through preservation of the soft tissue or soft-tissue augmentation procedures.
Although Wennström and Derks15 suggest keratinized gingiva around dental implants is not obligatory, other researchers note the need for this tissue and report less inflammation in the presence of keratinized gingiva.16 Azar,14 for example, suggests that an increasing number of studies demonstrates the need for keratinized gingiva around implants.

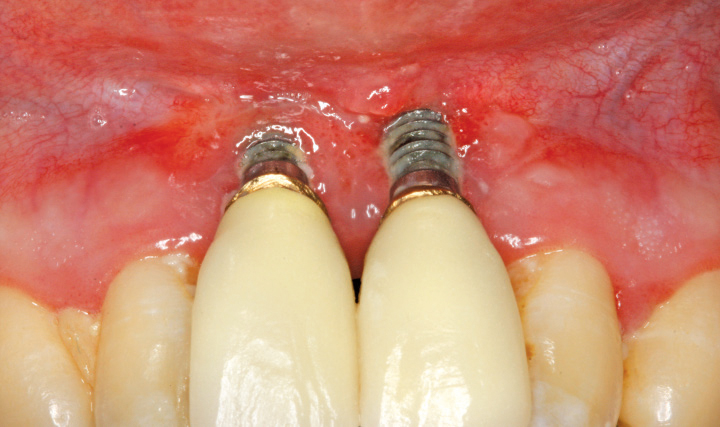
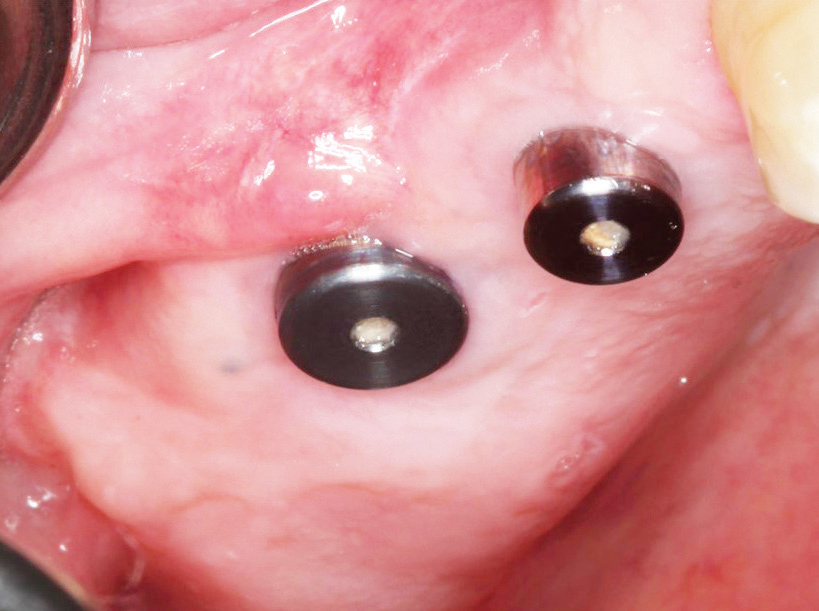
A stable peri-implant mucosa offers support to the underlying connective tissue. A successfully osseointegrated implant has collagen fibers that are oriented parallel to the implant, and the peri-implant tissue has decreased vascularity. These histological differences can significantly increase the risk for biofilm-induced inflammation around implants and subsequent bone loss.17–19 Figure 10 shows implants in the area of #8 and #9 that have gingival recession secondary to biofilm-induced inflammation. While keratinized gingiva around an implant promotes long-term health, it also provides resistance during the restorative phase. Figure 11 depicts an implant on #4 with high frenal attachment and lack of attached gingiva. Soft-tissue grafting can help address this problem.

THERAPEUTIC GOALS
According to the AAP’s “Parameters on Mucogingival Conditions,”20 therapeutic goals of mucogingival therapy are defined as nonsurgical and/or surgical correction of defects in morphology, position, and/or amount of soft tissue and underlying bone. This may be accomplished through a variety of procedures—including soft-tissue grafting for root coverage or gingival augmentation using alloplasts—and by controlling etiologic factors (including iatrogenic factors).
Early diagnosis of gingival recession is critical to early intervention and successful outcomes. Although not every case of recession warrants treatment, the foregoing discussion should help clinicians evaluate etiology and factors that indicate the need for a therapeutic solution.
REFERENCES
- American Academy of Periodontology. Glossary of Periodontal Terms. Available at:184.106.75.105/sites/default/files/files/PDFs/Clinical%20Resources/GlossaryOfPeriodontalTerms2001Edition.pdf. Accessed May 10, 2017.
- Albandar JM, Kingman A. Gingival recession, gingival bleeding, and dental calculus in adults 30 years of age and older in the United States, 1988–1994. J Periodontol. 1999;70:30–43.
- Armitage GC. Development of a classification system for periodontal diseases and conditions. Ann Periodontol.1999;4:1–6.
- Chan HL, Chun YH, MacEachern M, Oates TW. Does gingival recession require surgical treatment? Dent Clin North Am. 2015;59:981–996.
- Lang NP, Löe H. The relationship between the width of keratinized gingiva and gingival health. J Periodontol.1972;43:623–627.
- Kennedy JE, Bird WC, Palcanis KG, Dorfman HS. A longitudinal evaluation of varying widths of attached gingiva. J Clin Periodontol. 1985;12:667–675.
- Chambrone L, Tatakis DN. Periodontal soft tissue root coverage procedures: a systematic review from the AAP Regeneration Workshop. J Periodontol. 2015;86(Suppl 2):S8–S51.
- Heasman PA, Holliday R, Bryant A, Preshaw PM. Evidence for the occurrence of gingival recession and non-carious cervical lesions as a consequence of toothbrushing. J Clin Periodontol. 2015;42(Suppl 16):S237–S255.
- Joss-Vassalli I, Grebenstein C, Topouzelis N, Sculean A, Kastros C. Orthodontics therapy and gingival recession: a systematic review. Orthod Craniofac Res. 2010;13:127–141.
- Cairo F, Pagliaro U, Buti J, et al. Root coverage procedures improve patient aesthetics. A systematic review and Bayesian meta-analysis. J Clin Periodontol. 2016;43:965–975.
- Miller PD Jr. Root coverage using the free soft tissue autograft following citric acid application. III. A successful and predictable procedure in areas of deep-wide recession. Int J Periodontics Restorative Dent. 1985;5:14–37.
- Douglas de Oliveira DW, Oliveira-Ferreira F, Flecha OD, Gonçalves PF. Is surgical root coverage effective for the treatment of cervical dentin hypersensitivity? A systematic review. J Periodontol. 2013;84:295–306.
- Kim DM, Neiva R. Periodontal soft tissue non-root coverage procedures: a systematic review from the AAP Regeneration Workshop. J Periodontol. 2015;86(Suppl 2):S56–S72.
- Azar DE. Dental implant uncovering techniques with emphasis on increasing keratinized mucosa. Compend Contin Educ Dent. 2015;36:290–292,294,296–297.
- Wennström JL, Derks J. Is there a need for keratinized mucosa around implants to maintain health and tissue stability? Clin Oral Implants Res. 2012;23(Suppl 6):136–146.
- Greenstein G, Cavallaro J. The clinical significance of keratinized gingiva around dental implants. Compend Contin Educ Dent. 2011;32:24–31.
- Berglundh T, Lindhe J, Jonsson K, Ericsson I. The topography of the vascular systems in the periodontal and peri-implant tissues in the dog. J Clin Periodontol. 1994;21:189–193.
- Ericsson I, Persson LG, Berglundh T, Marinello CP, Lindhe J, Klinge B. Different types of inflammatory reactions in peri-implant soft tissues. J Clin Periodontol. 1995;22:255–261.
- Berglundh T, Lindhe J, Ericsson I, Marinello CP, Liljenberg B, Thomsen P. The soft tissue barrier at implants and teeth. Clin Oral Implants Res. 1991;2:81–90.
- American Academy of Periodontology. Parameters on mucogingival conditions. J Periodontol. 2000;71(Suppl 5):861–862.
Featured photo by ELIZABETH BALDWIN, DDS
From Dimensions of Dental Hygiene. July 2017;15(7):53-56.



