 Sakurra / iStock / Getty Images Plus
Sakurra / iStock / Getty Images Plus
Addressing Gingival Recession
A knowledge of available treatments is key to effective management of this common issue.
Gingival recession is a common patient complaint and comes with a variety of etiologies. Modern dentistry has brought a plethora of treatment options to choose from. This edition of Perio Update focuses on connective tissue grafts and growth factors.
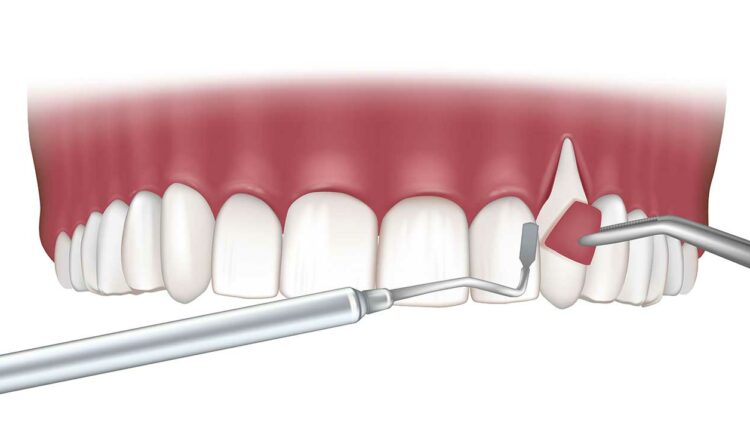
Evidence demonstrates the efficacy of connective tissue grafts in the treatment of gingival recession. The connective tissue graft is harvested from the palate in a single incision, underneath the overlying epithelium, or de-epithelialized after removal from the donor site. It is then introduced to the recipient site as part of a coronally advanced or rotated flap or tunnel (Figure 1 and Figure 2).1
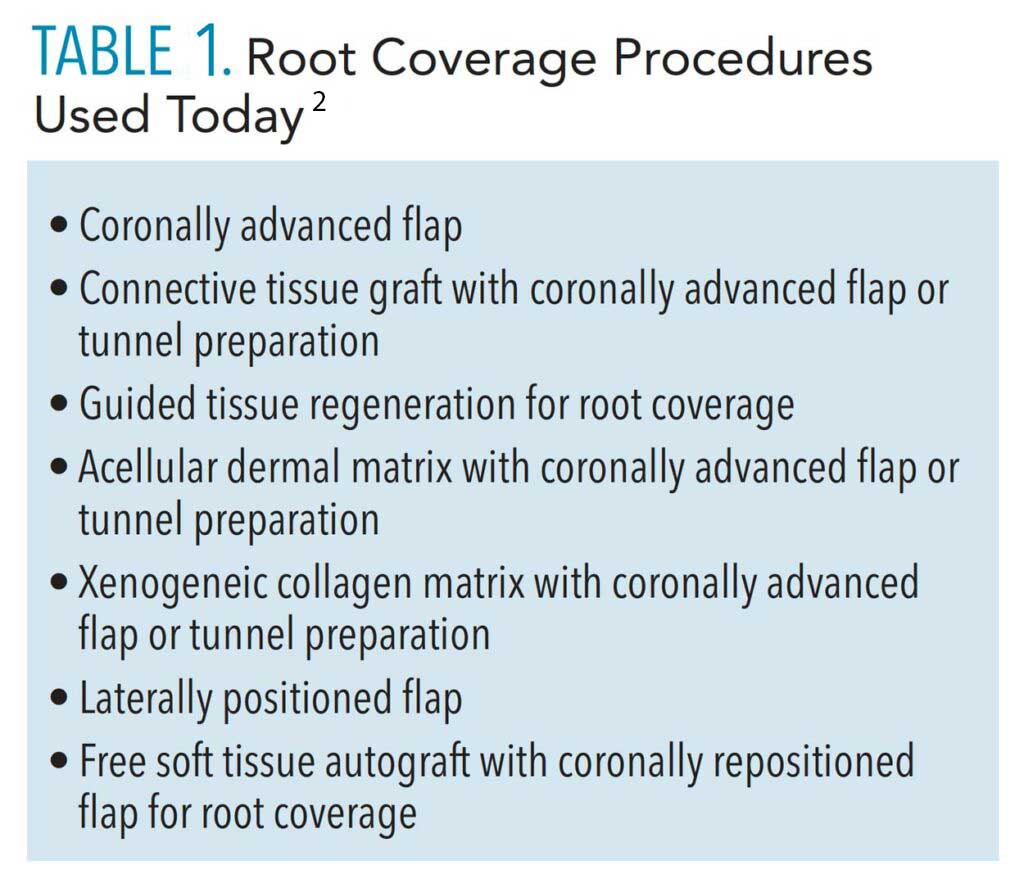
The use of nonautogenous materials, such as allografts or xenografts, provides viable alternatives to the connective tissue graft to reduce patient comorbidities.1 Table 1 includes a list of available materials and techniques.2
Role of Growth Factors
Growth factors can also be used to accelerate healing. They stimulate the chemotaxis, mitogenesis, and matrix formation of wound-healing cells.1 Another molecular mediator, enamel matrix derivative, contains different proteins and enzymes from developing pig enamel and enhances fibroblast recruitment and adhesion and angiogenesis.3 These products can hydrate grafts and matrices or directly at the recipient site.

Possible Risks
Dental caries, lesions, or cervical restorations may affect root coverage procedures. Noncarious cervical lesions (NCCLs) vary in appearance and result from abrasion, erosion, and corrosion from marginal restorations. The decision to graft or restore NCCLs is often debated. If the lesion extends more than 2 mm into the root surface, it should be restored.4
The lesion’s depth and shape, root convexity, thickness, amount of attached tissue present, and esthetic interests should all be considered.4 Root reshaping with burs or hand instruments shortens the distance cells need to travel for graft vascularization.5 NCCLs, root caries, and defective restorative margins should be diagnosed and treated before surgery.

References
- Chambrone L, Salinas Ortega MA, Sukekava F, et al. Root coverage procedures for treating localised and multiple recession-type defects. Cochrane Database Syst Rev. 2018;10:CD007161.
- Tavelli L, Barootchi S, Cairo F, Rasperini G, Shedden K, Wang HL. The effect of time on root coverage outcomes: a network meta-analysis. JDent Res. 2019;98:1195–1203.
- Gestrelius S, Lyngstadaas SP, Hammarström L. Emdogain—periodontal regeneration based on biomimicry. Clin Oral Investig. 2000;4:120–125.
- Allen EP, Winter RR. Interdisciplinary treatment of cervical lesions. Compend Contin Educ Dent. 2011;32:16–20.
- Gordon HP, Sullivan HC, Atkins JH. Free autogenous gingival grafts. II. Supplemental findings—histology of the graft site. Periodontics. 1968;6:130–133.
This information originally appeared in Saltz AE, Sirois V. The dental hygienist’s role in treating gingival recession. Dimensions of Dental Hygiene. May 2022; 20(5)32-35.