See the Signs
Oral health professionals need to be aware of the symptoms of domestic violence and understand how to effectively assist victims.
This course was published in the May 2015 issue and expires May 31, 2018. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Define the “ask, validate, document, and refer/report if required by law” model for inquiring about domestic violence.
- Identify common signs of overall abuse and abuse specific to the head and neck region.
- Discuss the role of the dental hygienist in ensuring dental appointments are as stress-free as possible.
Domestic violence is defined by the United States Centers for Disease Control and Prevention as “physical, sexual, or psychological harm by a current or former partner or spouse which can occur among heterosexual or same-sex couples and does not require sexual intimacy.”1 Domestic violence, also known as intimate partner violence, is a very serious yet preventable public health issue.
It is important for dental professionals to understand the dynamics of abuse and the purposeful tactics abusers use to gain power and control over their partners. Power is not inherently evil, and many forms of power imbalance exist in society for legitimate purposes. For example, teachers have power over students, parents over children, and police over the general public. However, some people try to gain power over others they have no right to claim, and some individuals in positions of power choose to abuse it by means of violence, threats, and coercion. Table 1 lists examples of tactics abusers use to exert control over their partners.2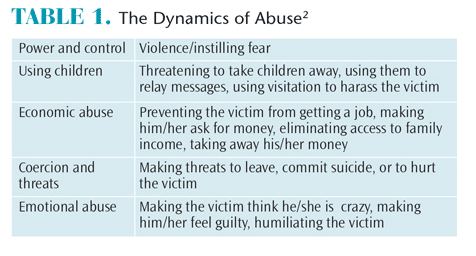
While there are many definitions of abuse, its dynamics are complex. Context is key to understanding the full story, and background questions are important to ask when performing an assessment. Just as a diagnosis would not be made in the dental operatory without a full medical, social, and physical history, conclusions cannot be drawn from a fraction of the whole picture while assessing a patient who may be a victim of domestic violence.
PUBLIC HEALTH ISSUE
There are many public health initiatives to educate people and lessen the prevalence of obesity, smoking, and other preventable issues. Domestic violence should be treated no differently. Preventing and easing the burden of domestic violence begins with creating awareness among health care providers. At least one in three women in the US has been physically or sexually assaulted by her boyfriend or husband at some point in her life.3 Domestic violence is also an important dental health issue, as 75% of injuries from family violence are sustained in the head, face, and/or mouth region.4
The lack of response in the face of this prevalent health issue is alarming. In a survey of 407 dentists, only 7% reported having suspected a case of elder abuse and only 1% filed a report.5 A second survey of 321 dentists found that 87% reported never having screened for any kind of domestic violence.5 The dental health care team is in a unique position to recognize domestic violence and offer support to victims to attain an improved quality of life and overall health. In four different studies of survivors of abuse, 70% to 81% reported that they would like their health care providers to ask them privately about intimate partner violence.6–10
THE AVDR MODEL
The “ask, validate, document, and refer/report if required by law” (AVDR) model can be used by dental health care providers to effectively inquire about and respond to domestic violence. Barbara Gerbert, PhD, director of the Center for Health Improvement and Prevention Studies, and colleagues at the University of California, San Francisco School of Dentistry developed a brief tutorial with case studies to demonstrate this intervention in action.11 It is available at: futureswithoutviolence.org.
Dental health care providers should aim to practice with a trauma-informed perspective.12 This includes recognizing that any patient who walks into the operatory may have a current or past history of abuse or trauma, regardless of whether it is disclosed or he or she appears like a victim or an abuser.12 This assumption enables clinicians to treat patients sensitively and reduces the potential for retraumatization. During the verbal and extra/intraoral screening, clinicians may pick up on subtle warning signs.
All patients should be screened for domestic violence. Patients should be informed that all of the practice’s patients are being asked about domestic violence as a part of routine screening to prevent them from feeling singled out.
Prior to inquiring about domestic violence, the following precautions must be taken: patient is alone; an appropriate interpreter is present, if needed; patient is aware of limits to confidentiality; and clinician knows how to respond if abuse is disclosed.11
In addition to asking patients about domestic violence, clinicians should also look for signs of abuse. Table 2 and Table 3 provide a list of abuse manifestations.6,8,13,14 Often, the signs of abuse are subtle, so it is important to listen to the patient carefully and be extremely observant while performing extraoral and intraoral exams.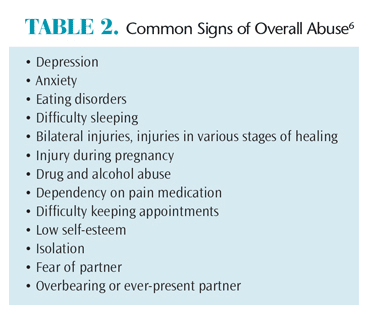
When asking direct questions about abuse, using “framing statements” may make both clinicians and patients feel more comfortable. For example:
- Clinician notes an injury and suspects it may be due to domestic violence. Clinician says, “This type of bruising often occurs when someone grabs your face really hard. Was the injury to your face accidental or did someone do this to you?”
- Clinician wants to convey concern about an observed behavior and create an opening for the patient to share more. Clinician comments, “Your partner seemed really angry when we asked him to step out. Are you afraid of him or ever feel unsafe with him? Will you feel safe leaving here with him today?”
- Oral health professionals can ask inquiry questions as part of routine screening. For example, the clinician might say, “We know that some of our patients are unsafe in their relationships, which can lead to health problems. Is anyone hurting you, controlling you, or making you afraid?”
Validating statements can facilitate conversation between the clinician and patient. It will help avoid patients feeling like they are being judged or that clinicians are jumping to conclusions. Clinicians must be careful to avoid victim blaming or extreme statements if disclosure of abuse is made. As an outsider, it may be difficult to understand why some victims stay with an abusive partner, or appear to deny or minimize the abuse. Whatever the case, clinicians do not comprehend the full picture of patients’ experiences or their reasons behind their decision making. It is not the clinician’s place to judge, but rather to respect patients’ autonomy and support them in an appropriate and individualized manner.11
Documentation of the interaction with the patient and the signs/symptoms observed is crucial for the patient’s health and legal purposes. The following tips should be considered during the documentation process: use patient’s words and/or describe demeanor; record objective clinical findings; describe (or photograph) location, size, shape, color, nature of injuries, or other conditions in detail; and record treatment plan, follow-up instructions, referrals, and reports made.11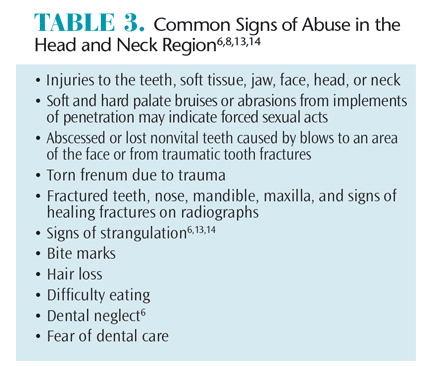
Upon asking the initial questions, if no abuse is reported, accept the patient’s response and respect his or her right to self-determination. If abuse is suspected due to injuries or other behaviors despite the lack of disclosure, concern for the patient’s safety and health should be expressed without conveying judgment of the victim or partner. The clinician should let the patient know that he or she is always welcome to seek help through the dental practice. The steps taken during the appointment should be documented in the patient’s record.11
If upon asking the initial question, the patient discloses past or current abuse, the clinician should listen, acknowledge, and validate the patient’s concerns. The key message that clinicians need to impart is that they understand the patient is in a difficult and scary situation that is not his or her fault, the patient is not alone, and they want to help him or her in any way possible.15 Clinicians should explore how the abuse is impacting the patient’s dental situation and how he or she has coped thus far. The patient can be asked if he or she has someone to talk to and whether he or she has any concerns about safety. This discussion should be documented in the patient’s record. Table 4 includes additional tips for assisting victims of domestic violence.13,16,17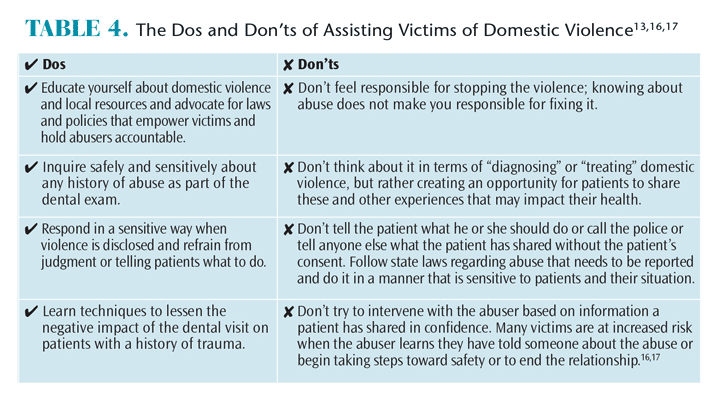
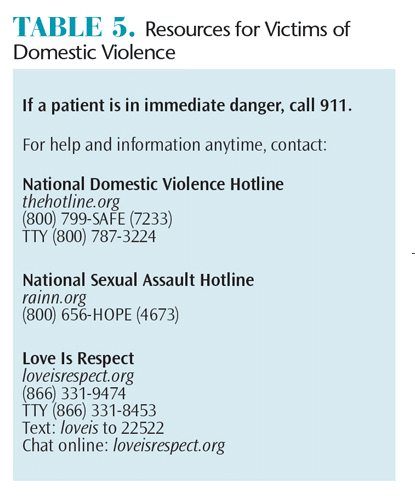
Dental practices should have a plan of action in case patients disclose abuse. First and foremost, safety concerns should be immediately addressed. Concern should be expressed and assistance offered with contacting authorities or an abuse hotline. There are national and local resources available to help victims (Table 5).18
Appropriate referral information should be provided in writing or verbally if it is unsafe for the patient to take or write down numbers. Keep in mind that risks are complex and different for every victim. If an abuser perceives a loss of control, which often happens if he/she learns that the victim is seeking help, the risk for the victim may increase. When a patient is provided with resources, such as a domestic violence hotline number or other handouts, keep in mind it may be unsafe for him or her to take it. Clinicians should be creative about giving information discretely, such as providing a generic business card or resource list that includes hotline numbers.
Clinicians should report the abuse to appropriate authorities if required by law. Each state has different regulations regarding the reporting of abuse depending on a victim’s age and other factors. Clinicians need to be aware of the laws in the state they practice in.19
![Resources for Victims of Domestic Violence]() DENTAL HYGIENIST’S ROLE
DENTAL HYGIENIST’S ROLE
Patients who have been victims of domestic violence can find dental appointments highly stressful. From their point of view, it is a situation where they once again feel they have no control and may feel frightened, helpless, or as if they are experiencing a past incident of abuse. Before the exam begins, patients should be asked about their anxiety level and what can be done to make them more comfortable. Clinicians should explain procedures and apprise patients of what’s to come. Keeping patients informed can help make dental appointments less traumatic.
CURRICULUM IN ACTION
Tufts University School of Dental Medicine (TUSDM) provides its students with a 4-year comprehensive curriculum that includes both didactic and clinical aspects of domestic violence education. During years 1, 2, and 3, lectures on domestic violence given by local experts are integrated into the coursework. During years 3 and 4, students treat patients who are or have been victims of domestic violence through the Dental Outreach to Survivors (DOTS) program. When the students receive their patients in the clinic, they are required to do a domestic violence assessment for each new patient. This helps regulate a screening process and run a trauma-informed practice. It also assists the future dental health care providers in becoming more comfortable assessing domestic violence. The AVDR model is followed under the supervision of faculty and staff.
The DOTS program was founded in 2003 to provide safe and confidential care to victims of violence by giving them free dental care and de-identifying the patients in the electronic medical/dental record system to keep them anonymous from their perpetrators. This umbrella of care under the DOTS program is open to any victim regardless of gender or sexual orientation.
The best way dental health care providers can eliminate domestic violence is to become educated. It is crucial to have an understanding of what domestic violence is, how it manifests, and how to recognize and help its victims.
REFERENCES
- Centers for Disease Control and Prevention. Intimate Partner Violence: Definitions. Available at: cdc.gov/ViolencePrevention/intimatepartnerviolence/ definition.html. Accessed February 22, 2015.
- Domestic Abuse Intervention Programs. Wheel Gallery. Available at: theduluthmodel.org/training/ wheels.html. Accessed February 22, 2015.
- Collins KS, Schoen C, Joseph S, Duchon L, Simantov E, Yellowitz M. Health Concerns Across a Woman’s Lifespan. The Commonwealth Fund 1998 Survey of Women’s Health. Available at: commonwealthfund.org/~/media/files/publications/f undreport/1999/may/ health-concerns-across-awomans- lifespan–the-commonwealth-fund-1998- survey-of-womenshealth/healthconcerns__ surveyreport-pdf.pdf. Accessed February 22, 2015.
- Sweet D. Recognizing and intervening in domestic violence: proactive role for dentistry. Medscape Womens Health.1996;1:3.
- Gironda M, Lefever K, Anderson E. Dental students’ knowledge about elder abuse and neglect and the reporting responsibilities of dentists. J Dent Educ. 2010;74:824–829.
- Futures Without Violence. Enhancing Dental Professionals’ Response to Domestic Violence. Available at: futureswithoutviolence.org/userfiles/file/HealthCare/ dental.pdf. Accessed February 22, 2015.
- Caralis PV, Musialowski R. Women’s experiences with domestic violence and their attitudes and expectations regarding medical care of abuse victims. South Med J. 1997;90:1075–1080.
- McCauley J, Yurk R, Jenckes M, Ford D. Inside “Pandora’s Box:” abused women’s experiences with clinicians and health services. J Gen Intern Med. 1998;13:549–555.
- Friedman L, Samet J, Roberts M, Hudlin M, Hans P. Inquiry about victimization experiences: a survey of patient preferences and physician practices. Arch Intern Med. 1992;152:1186–1190.
- Rodriguez M, Quiroga SS, Bauer H. Breaking the silence: battered women’s perspectives on medical care. Arch Fam Med. 1996;5:153–158.
- Futures Without Violence. The Ask, Validate, Document, Refer (AVDR) Tutorial for Dentists. Available at: futureswithoutviolence.org/the-askvalidate- document-refer-avdr-tutorial-for-dentists. Accessed February 22, 2015.
- National Association of State Mental Health Program Directors. Then National Center for Trauma Informed Care. Available at: nasmhpd.org/TA/ nctic.aspx. Accessed February 22, 2015.
- McClane GE, Shanel-Hogan KA, Strack GB. Never Let a Victim Die in Vain. San Diego City Attorney’s Office; 2001.
- Gwinn C, McClane GE, Shanel-Hogan KA, Strack GB. Domestic violence: No place for a smile. J Calif Dent Assoc. 2004;32:399–409.
- Shanel-Hogan, KA. Dental Professionals Against Violence. Available at: vdh.virginia.gov/ofhs/ prevention/dsvp/projectradarva/documents/older/pd f/dentalmanual.pdf. Accessed February 22, 2015.
- Browne A. When Battered Women Kill. New York: The Free Press; 1987.
- Sonkin D, Martin D, Walker LEA. The Male Batterer: A Treatment Approach. New York: Springer; 1985.
- Futures Without Violence. Get Help. Available at: futureswithoutviolence.org/resources-events/get-help. Accessed February 22, 2015.
- Family Violence Prevention Fund. Compendium of State Statutes and Policies on Domestic Violence and Health Care. Available at: futureswithoutviolence. org/userfiles/file/HealthCare/Compendium%20Final. pdf. Accessed February 22, 2015.
From Dimensions of Dental Hygiene. March 2015;13(3):48–51.


 DENTAL HYGIENIST’S ROLE
DENTAL HYGIENIST’S ROLE
