Revisit OSHA Compliance
To ensure the safety of both patients and clinicians, dental practices must adhere to occupational safety and health administration standards.
Recently, an oral surgeon agreed to have his license suspended after being cited by the Oklahoma Board of Dentistry for numerous infection control violations and failure to comply with Occupational Safety and Health Administration (OSHA) standards. The breaches and violations included using rusted and pitted instruments that were incapable of sterilization, lack of spore testing, reuse of single-use disposable medication vials, allowing untrained and unlicensed staff to administer intravenous medications, poor record keeping, inadequately trained staff, and the absence of written infection control policies.1 A full hearing on this case will occur at the next Oklahoma Board of Dentistry meeting on August 16, 2013.1 Breaches like these are quite disturbing, but they serve as strong reminders to all dental team members that regular review of the policies and procedures related to infection control is critical to safe practice.
WHAT IS THE OCCUPATIONAL SAFETY AND HEALTH ADMINISTRATION?
Part of the United States Department of Labor,2 OSHA creates standards to protect the safety of workers. Employers must comply with these standards or face enforcement penalties. Oral health care providers perform tasks regulated by OSHA standards every day. The possible exposure to blood and other potentially infectious materials (OPIM) falls under the OSHA Bloodborne Pathogens Standard.3
Bloodborne pathogens are disease-causing microorganisms transmitted through blood such as hepatitis B, hepatitis C, and human immunodeficiency virus. The Bloodborne Pathogens Standard outlines specific measures employers must comply with, including ensuring the availability of the hepatitis B vaccination, providing appropriate personal protective equipment, supplying safety devices, promoting safe techniques to avoid exposure incident, and implementing a postexposure protocol if an exposure to blood or OPIM occurs.3 Employers, in collaboration with users, also need to evaluate the potential utilization of engineered safety devices.4
EXPOSURE CONTROL PLAN
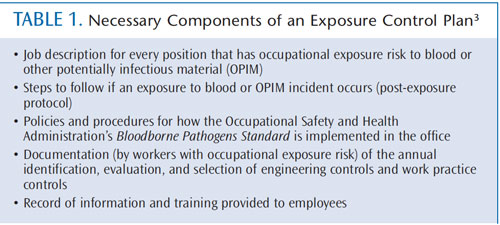
Employers are responsible for maintaining written policies and procedures that demonstrate compliance with OSHA standards, and they must be accessible to employees at all times.3 These policies make up what is known as an exposure control plan (ECP), which outlines how various procedures will be performed safely.3 Table 1 lists the key components of an ECP.3 Some offices may call this document the “OSHA manual” or “infection control manual” if it is combined with infection control policies and procedures. The first step in providing a safe environment for workers and patients is to have an open and honest discussion about OSHA standards, the US Centers for Disease Control and Prevention (CDC) guidelines, and infection control policies and procedures with all dental team members. Gaps in policies and practices should be addressed.
The ECP must be reviewed annually with all at-risk workers, when new employees are hired, and when an employee takes on any new tasks that involve risk for occupational exposure. Whenever new policies, products, or procedures are implemented, the ECP must be updated, with revisions communicated to all employees. Employers can create their own ECP document or use a template, many of which are available free of charge on the OSHA website.5 Templates can serve as a guide but must be tailored specifically for each office. ECP templates can also be purchased and customized through a consulting service. Visit the Organization for Safety and Prevention (OSAP) website for a listing of dental infection control consultants by state.6
ENFORCEMENT
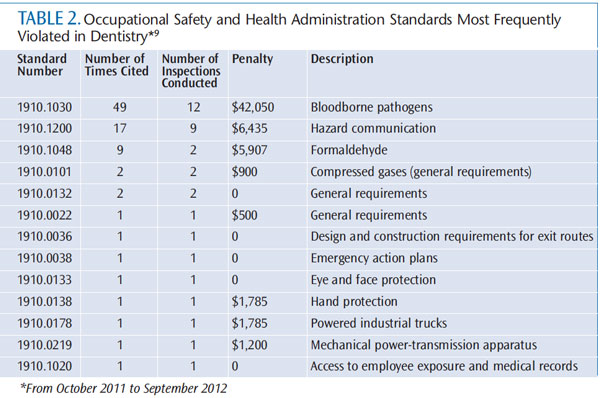
OSHA is a regulatory agency, meaning it can conduct inspections and investigations to ensure that its regulations are enforced. Fines can also be assessed by OSHA for noncompliance with standards.7,8 The two most commonly violated OSHA standards in dentistry are the Bloodborne Pathogens Standard and the Hazard Communication (Haz-Com) Standard, which account for 75% of all cited standards.9 From October 2011 to September 2012, OSHA had 182 open investigations in dentistry.10 Complaints from employees, patients, or referrals from other agencies can trigger an OSHA investigation. Occasionally, OSHA performs random inspections, but it primarily conducts planned inspections in which an office has prior notification.8 Table 2 provides a list of commonly cited OSHA standards in dentistry and associated penalties.9
CENTERS FOR DISEASE CONTROL AND PREVENTION GUIDELINES
The Guidelines for Infection Control in Dental Health-Care Settings—2003 are 10 years old, but they are still considered appropriate recommendations for infection control.11 The CDC is not a regulatory agency like OSHA, however, many regulatory agencies and state boards of dentistry seek guidance from the CDC and defer to these comprehensive guidelines when making decisions related to safety. Many states have adopted the CDC guidelines as law, which then carries regulatory enforcement.
The CDC guidelines cover a wider realm of infection control policies, and they are designed especially for dental offices. For instance, the CDC guidelines provide specific parameters on dental unit waterlines, dictating that bacterial counts of outgoing dental unit water should be “as low as reasonably achievable” and must minimally meet the Environmental Protection Agency drinking water standard of <500 colony-forming units. With the well-publicized 2011 death of an elderly woman from Legionnaire’s disease due to dental unit waterline contamination, it is clear that this aspect of infection control policy and procedure is paramount to safety.12
RELATED STANDARDS
The OSHA HazCom Standard protects workers who are at risk of chemical exposure. Employers must provide training and protective equipment for employees who handle chemicals.13 A wide array of chemicals are used in the dental office such as surface disinfectants, cleaning agents, and dental materials. Every chemical on the market must contain a material safety data sheet (MSDS) that provides workers with information on safe handling, including methods for storage, disposal, and first aid instructions in case of exposure. MSDS information must be accessible to at-risk employees at all times (either in hard or electronic copy).13
Recent changes to the OSHA HazCom Standard14 have been made to more closely align it with the United Nations’ Globally Harmonized System of Classification and Labeling of Chemicals.15 One of the major changes is the requirement that manufacturers worldwide begin using a new labeling system for chemicals by 2015. The global universal system includes the use of new standardized pictorial diagrams and explanations. The second major change is the mandate that manufacturers move to a standardized format for safety data sheets (SDSs), formerly MSDSs. All employees who work with chemicals must be trained by their employers on the new labeling system and the SDS format by December 1, 2013, to be OSHA compliant.16 Free “Quickcards” are downloadable in PDF format to assist with this training.16
TRAINING REQUIREMENTS
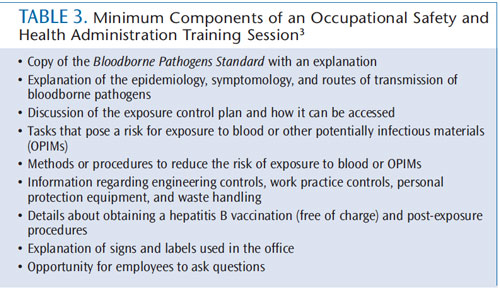
Training on the Bloodborne Pathogens Standard must be made available to employees during their regular working hours at no cost. Training must be provided upon hire before any tasks related to occupational risk are performed. It must also take place at least annually and when any new tasks or procedures are implemented. The training material must be provided in a language and at a level that the employee can understand, and the employee must be provided with an opportunity to ask questions. The person conducting the training must possess knowledge of epidemiology, symptomology, modes of transmission of bloodborne pathogens, vaccinations, and post-exposure prophylaxis.
The trainer must also review the ECP and provide site-specific information on how the OSHA and infection control procedures are implemented in the facility. Table 3 provides the minimum components of an OSHA training session.3 Dental hygienists are the most logical team members to provide OSHA training because they have an educational background in microbiology and disease transmission.17 The American Dental Association (ADA) Commission on Dental Accreditation (CODA) requires that all entry-level dental hygiene programs have course content in basic sciences, biological sciences, dental and dental hygiene sciences, microbiology, and immunology.17 Dental hygiene science course content must include infection control and hazard management, as well as instruction on how to provide oral health care to individuals with bloodborne diseases.17 Students in dental hygiene programs must comply with institutional policies related to the OSHA Bloodborne Pathogens Standard.17 Graduates of dental hygiene programs must meet basic competencies standards in infection control and bloodborne pathogens set forth by CODA in order to graduate and gain a license to practice.17
RECORDKEEPING
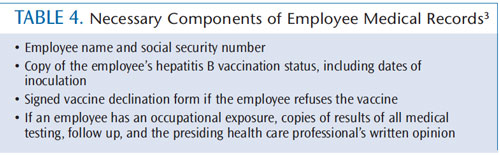
Employers must keep records of OSHA compliance and training.3 A medical record for each employee with occupational risk needs to be kept on file. Table 4 lists the necessary components of employee medical records.3 Medical records should be kept confidential and not disclosed to anyone without the employee’s permission. They should be stored for the length of employment, plus an additional 30 years.2
TAKE ACTION
The time is right to review OSHA standards, the practice’s ECP, CDC guidelines, and infection control policies and procedures with all dental team members. Emphasizing compliance with OSHA standards and infection control policies and procedures is the first step to providing a safe environment for both clinicians and patients. Patients will begin asking more questions due to the abundance of news coverage regarding the Oklahoma case, so each dental team member should be able to comfortably discuss infection control policies and procedures. The ADA and OSAP have online resources, including talking points, to aid dental team members in discussing this case and infection control concerns with patients.18,19
ACKNOWLEDGEMENT
The authors would like to thank Sarah Everett and Lauren Lewis for their help in preparing this manuscript.
REFERENCES
- Oklahoma Board of Dentistry. Available at: www.ok.gov/dentistry. AccessedMay 15, 2013.
- Occupational Safety and Health Administration. Available at: www.osha.gov/about.html. Accessed May 15, 2013.
- Occupational Safety and Health Administration. Bloodborne Pathogens Standard.Available at: www.osha.gov/ pls/oshaweb/ owadisp.show_ document?p_table=standards&p_id=10051. Accessed May 15, 2013.
- Occupational Safety and Health Administration. Appendix B (EngineeringControl Evaluation Forms). Available at: www.osha.gov/ pls/ oshaweb/owadisp.show_document?p_table=DIRECTIVES&p_id=2570#APPBeval.Accessed May 15, 2013.
- Occupational Safety and Health Administration. Model Plans and Programsfor the OSHA Bloodborne Pathogens and Hazard Communications Standard. Available at: www.osha.gov/Publications/osha3186.pdf. Accessed May 15, 2013.
- Organization for Safety and Prevention. Consultant Listing Information.Available at: www.osap.org/?page=NetworkConsultants. Accessed May 15, 2013.
- Occupational Safety and Health Administration. OSHA Enforcement.Available at: www.osha.gov/dep/index.html. Accessed May 15, 2013.
- Occupational Safety and Health Administration. OSHA Fact Sheet. Availableat: www.osha.gov/OshDoc/data_General_Facts/factsheet-inspections.pdf. Accessed May 15, 2013.
- Occupational Safety and Health Administration. 8021 Offices and Clinics ofDentists. Available at: www.osha.gov/ pls/ imis/ citedstandard.sic ?p_esize=&p_state= FEFederal&p_sic=8021. Accessed May 15, 2013.
- Occupational Health and Safety Administration. Inspections Within Industry.Available at: www.osha.gov/pls/imis/industry.html. Accessed May 15, 2013.
- Centers for Disease Control and Prevention. Guidelines for infection controlin dental healthcare settings — 2003. Available at: www.cdc.gov/ mmwr/preview/mmwrhtml/rr5217a1.htm. Accessed May 15, 2013.
- Ricci ML, Fontana S, Pinci F, et al. Pneumonia associated with a dental unitwaterline. Lancet. 2012;379:684.
- Occupational Safety and Health Administration. Hazard Communication1910.1200. Available at: www.osha.gov/ pls/ oshaweb/ owadisp.show_ document?p_table=standards&p_id=10099. Accessed May 15, 2013.
- Occupational Safety and Health Administration. Hazard Communication.Available at: www.osha.gov/dsg/hazcom/index.html. Accessed May 15, 2013.
- Occupational Safety and Health Administration. Federal Register at:www.osha.gov/pls/oshaweb/owadisp.show_document?p_table=FEDERAL_REGISTER&p_id=22607. Accessed May 15, 2013.
- Occupational Safety and Health Administration. Hazard Communication.Available at: www.osha.gov/dsg/hazcom/hazcom-faq.html#22. Accessed May 15, 2013.
- American Dental Association. Accreditation Standards for Dental HygieneEducation Programs. Available at: www.ada.org/ sections/ education And Careers/pdfs/dh.pdf. Accessed May 15, 2013.
- Organization for Safety and Prevention. Oklahoma Infection ControlBreach. Available at: www.osap.org/?page=Oklahoma. Accessed May 15, 2013.
- American Dental Association. ADA Statement on Infection Control in DentalSettings. Available at: www.ada.org/8454.aspx. Accessed May 15, 2013.
From Dimensions of Dental Hygiene. June 2013; 11(6): 30, 32, 34, 36.

