
Restore Periodontal Health
Effective nonsurgical periodontal therapy is key to improving and maintaining the oral health of patients with moderate to advanced chronic periodontitis.
Nonsurgical periodontal therapy (NSPT)—sometimes called phase I or initial therapy—is key to restoring periodontal health for patients with moderate to advanced chronic periodontitis.1,2 Research indicates that treatment outcomes are more dependent on NSPT than surgical procedures.1 The current instrumentation armamentarium is filled with options to facilitate scaling and root planing for these patients. With the aid of a thorough health history, appropriate radiographs, comprehensive periodontal risk assessment, and adequate pain management, dental hygienists are well equipped to improve the end result of NSPT.
Classification
When treating patients with moderate to advanced chronic periodontitis, the severity of disease must first be determined. Moderate severity is characterized by attachment loss of 3 mm to 4 mm, and bone loss beyond the crest and up to one-third of supporting structures. Class I (incipient) furcation may be present with pocket depth up to 6 mm if the gingival contour is normal.3 Advanced periodontitis is characterized by more than 4 mm of attachment loss, and bone loss greater than one-third of the supporting structures. Furcation invasion greater than class I is usually present, in addition to mobility. When the gingival contour is normal, localized deep pockets of 6 mm or greater may also be observed.4
The careful evaluation of attachment loss as part of a comprehensive periodontal examination is key to assessing the severity of chronic periodontitis.2 Instrumentation must then be fastidious, thorough, and efficient. The clinician must strive to remove all subgingival plaque biofilm, plaque retentive factors, and calculus-embedded cementum so adjacent tissues can heal.5
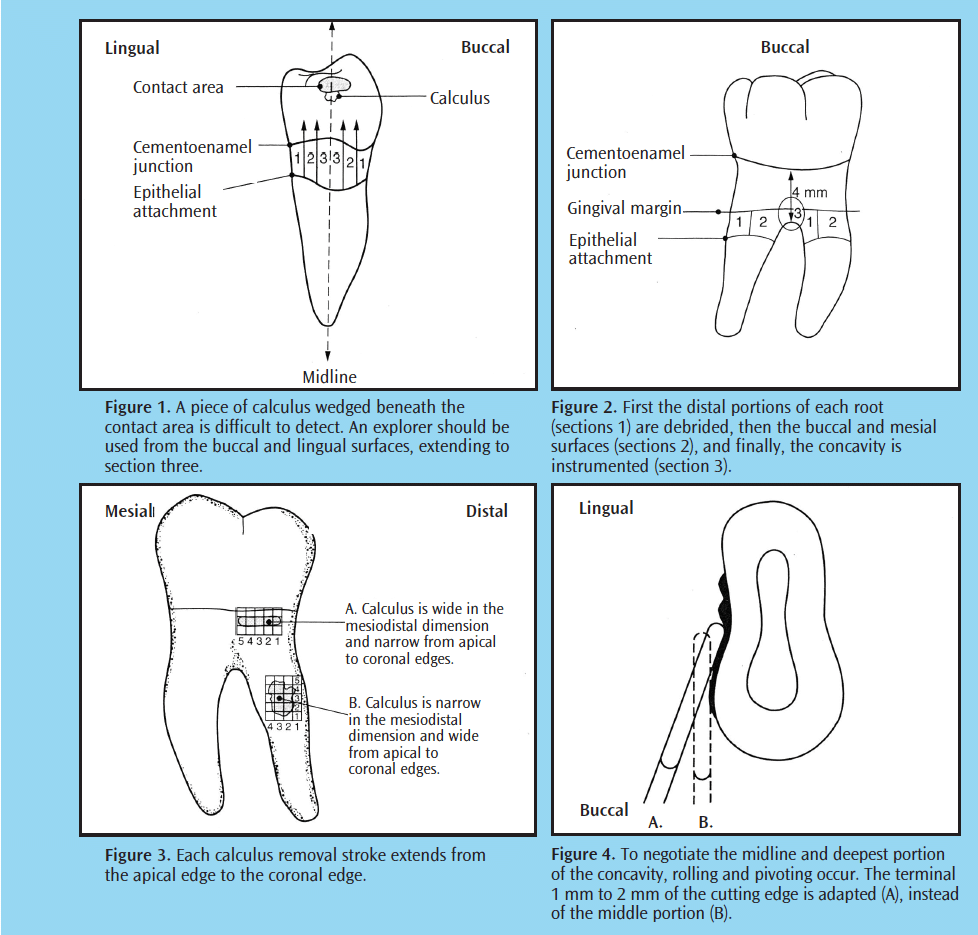 An explorer (11/12 standard or extended shank) must be used to assess the outcome after scaling and root planing is complete (Figure 1).6 Re-evaluation of inflammation and bleeding on probing, pocket depth, clinical attachment gain, and self-care efficacy should be completed at a 4-week to 6-week interval post-instrumentation during phase I therapy or at a separate visit.1,7-10
An explorer (11/12 standard or extended shank) must be used to assess the outcome after scaling and root planing is complete (Figure 1).6 Re-evaluation of inflammation and bleeding on probing, pocket depth, clinical attachment gain, and self-care efficacy should be completed at a 4-week to 6-week interval post-instrumentation during phase I therapy or at a separate visit.1,7-10
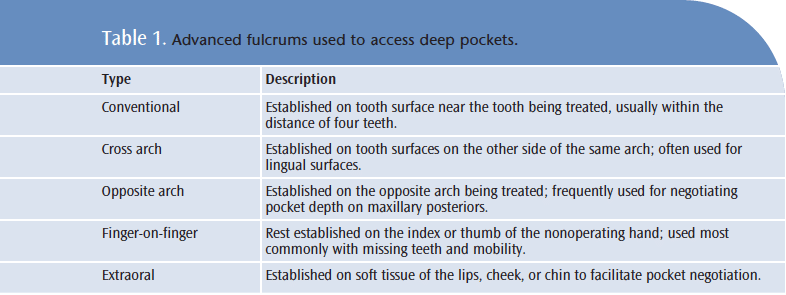
Accessing deep pockets usually requires the use of advanced fulcrums such as a cross arch, opposite arch, finger-on-finger, or extraoral (Table 1). These fulcrums aid the practitioner in negotiating the root concavities and depressions in deep pockets and furcations (Figure 2-Figure 4). The goal of alternative fulcrum use is to reach all subgingival surfaces with correct adaptation.11 The working end should be placed subgingivally prior to fulcrum placement.
Periodontal Files
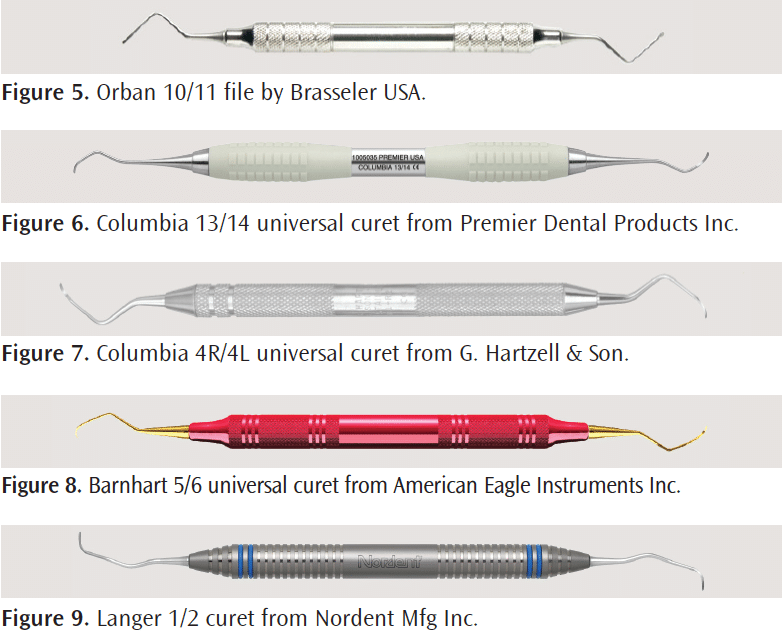
To start the instrumentation process, periodontal files are recommended for tenacious deposits, regardless of their size. Periodontal files are especially effective with burnished deposits. Each file has a head with multiple cutting edges that—when adapted parallel to calculus deposits—can cause fracture. Three common designs include the Hirschfeld series (3/7, 5/11, 9/10) with three cutting edges; Orban (10/11, 12/13, Figure 5) with six cutting edges; and Bedbug with 10 cutting edges. Hirschfeld and Orban files are used on larger tenacious deposits and overhanging amalgams with or without the aid of ultrasonic instrumentation. The Bedbug is a fine instrument used for smoothing roots and cementoenamel junctions, and finishing overhanging restorations.
![]() Universal Curets
Universal Curets
Universal curets frequently used in NSPT include the Columbia (13/14, 2R/2L, and 4R/4L, Figure 6 and Figure 7) and Barnhart (1/2 and 5/6, Figure 8). Their shank length is sometimes a problem in deep pockets, but their ability to negotiate line angles and facilitate multidirectional strokes, as well as their ease of use in depths of 5 mm or less, makes them a popular choice. Advanced fulcrums used with universal designs include cross arch, opposite arch, and some modified conventional fulcrums.
Langer curets are made with standard blades, extended shanks, or mini-blades (Figure 9). They have two parallel working edges and a complex functional shank—combining both universal and area-specific designs. The Langer 1/2, 3/4, and 5/6 are needed to treat the entire dentition.
Area-Specific Curets
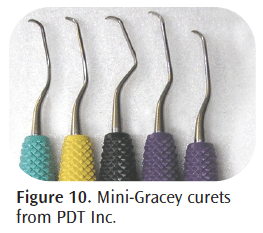
Area-specific curets are often selected for NSPT. Designs include the standard for pockets of 4 mm of less, extended shank (3 mm longer than the standard) for deep pockets (5 mm and deeper), and mini-bladed with 50% shorter and narrower working end and 3 mm longer shank than the standard (Figure 10). In addition, micro mini-bladed instruments are available with blades that are 20% thinner than mini-bladed curets to reduce tissue distention and enhance subgingival insertion. The terminal shank is elongated for deep access into pockets and the shank rigidity is increased.
Advanced fulcrum techniques, such as the opposite arch and extraoral fulcrums, are needed when using area-specific curets in deep pockets to maintain the terminal shank parallel with the root surface while gaining access to the epithelial attachment. Many clinicians use the flexible shank area-specific instruments for root planing, however, varying shank rigidity is available, including extra rigid for tenacious deposit removal. Nagy et al evaluated the effects of scaling and root planing with rigid longer shank Gracey curets and rigid standard Gracey curets and found no significant difference between the two.12
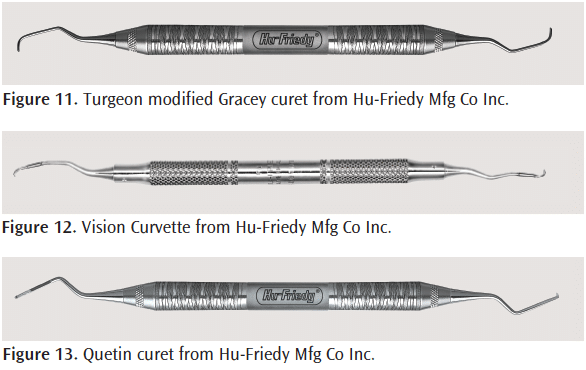
Turgeon curets feature a narrower working end that is easy to insert (Figure 11). Also, the blade is designed with a different cross section than traditional designs that is easy to sharpen. Vision Curvettes™ (Sub-zero, 1/2, 11/12, 13/14 with 5 mm and 10 mm shank markings) are mini-bladed instruments that are 50% shorter than the standard area-specific curets and feature a blade that curves upward (Figure 12). The curvature is intended to adapt closely to line angles and anterior teeth, however, there is a risk of gouging the root surfaces. In one in vitro study, subgingival deposit removal with a Sub-zero Curvette and a Gracey 1/2 on a dentoform was compared.13 Results indicated that the Curvette removed significantly more of the surface material (black enamel paint) than the curet.
Quetin curets are used to instrument furcations and root concavities/depressions. The working end is small (0.9 mm or 1.3 mm). The cutting edges and back are rounded to help prevent root gouging (Figure 13). O’Hehir debridement curets can remove light calculus from the root surface (Figure 14). The shank is extended, the working end is circular, and a push or pull stroke is used. The working end curves, making adapting to furcations, grooves, and line angles easier.
Diamond-coated files (Nabers-shaped and mesial/ distal) are used with endoscopic evaluation of furcations and root depressions (Figure 15). Unlike periodontal working files, they are finishing instruments coated with a very fine diamond surface around the working end, therefore, light pressure must be used to avoid gouging. Overinstrumentation may occur if they are not placed directly on the deposit, too much pressure is used, they are adapted incorrectly, or they are used too long in one place.14
Ultrasonic Options
Ultrasonic instruments—either magnetostrictive or piezoelectric—offer a wide variety of inserts or tips to remove large as well as fine deposits. There are many ultrasonic insert/tip (UIT) designs, such as universal (Figure 16 and Figure 17); right, left, and straight slim precision (Figure 18 and Figure 19); and furcation UITs (Figure 20). Standard universal designs are used for removing larger deposits, which are followed by slim UITs for pocket negotiation. A slim straight UIT is ideal for deep narrow pockets and anterior teeth. The slim right and left designs adapt well to root surface concavities and depressions. The left, right, and straight furcation UITs have a 0.8 mm ball end that is placed within the furcation, concavities, and grooves (Figure 20). One in vitro study comparing this design to a straight ultrasonic UIT and Gracey curet concluded that the ball-ended furcation UIT was more effective.15 Diamond-coated UITs are also available (Figure 21 and Figure 22). They may produce a rougher surface than plain UITs and curets, but they can be effective in root planing—allowing for a quicker finish than with plain UITs and curets.16-19 However, all diamond-coated UITs must be used with extreme caution and only when parallel to the root surface on low power.
Deep Pockets, Furcations, and Mobility
Initial therapy for patients with moderate to advanced chronic periodontitis often presents three challenges: deep periodontal pockets, furcation involvement, and mobility. Knowledge of root surface morphology is key in instrument selection and effectiveness. One of the most common problems with root adaptation is missing the proximal concavities of surfaces. To correct this problem, adequate pivoting and rolling of the instrument should be used to meet the needs of the root anatomy (Figure 4). Another consideration is activation. Stroke direction must be varied. In addition to vertical and oblique strokes, horizontal strokes are needed to adequately cover the root surface and prevent striations caused by only working in one or two directions.
Self-evaluation of channeling is also critical. Removing the deposit “piece by piece” is accomplished with short, powerful, controlled wrist rocks while pivoting and rolling to keep the terminal end adapted. On the proximal surfaces, the goal is to channel calculus by advancing to the contact in a constant upward movement while maintaining proper adaptation (Figure 3). The best channeling approach depends on the width and length of calculus.
When treating multirooted teeth, consider addressing each root as a separate tooth with a combination of strokes. First the distal surfaces are treated, and then the buccal/lingual and mesial surfaces, applying overlapping strokes on the surface where the roots meet. Lastly, concentrate on the concavity coronal to the furcation entrance (Figure 2). If gingiva occludes the furcation, the periodontal pocket is shallow, or the furcation entrance is barely detectable, this method may not be feasible. In this case, treatment with a combination of strokes is essential. Often the furcation entrance is smaller than the diameter of a conventional curet,20 therefore, precision thin UITs, mini-bladed instruments, and furcation curets are recommended. Otero-Cagide and Long concluded that curets were significantly more efficient than UITs in removing paint (in vitro) from mandibular first molar root trunks and entrances.21 These authors also evaluated closed root debridement in vitro with modified-bladed curets and slim UITs. They concluded that there is potential value in using small-bladed curets for furcations during initial and supportive therapy.22 Both studies cited the need for corroboration of results through additional clinical studies.
Instrumentation of mobile teeth is sometimes needed in NSPT. The clinician’s mirror hand is used to stabilize the tooth. If only slightly mobile, stabilization occurs on the occlusal or incisal edge. If significant mobility exists, stability is needed from the surface opposite or adjacent to the one being treated. For example, if the facial surface of a mobile mandibular anterior is present, the index finger of the mirror hand is placed on the lingual surface near the incisal edge. Mobile teeth may interfere with optimal fulcrum placement, therefore, alternative fulcrums are needed when the tooth chosen for the finger rest is mobile.
Ultrasonic instrumentation differs from hand in that a modified pen grasp is used, an extraoral fulcrum is recommended, light featherlike pressure is all that is needed, and removal of larger deposits occurs coronally to apically. Similarities in ultrasonic and hand instrumentation include the stroke directions needed, the use of alternative fulcrums for access, and the desired outcomes of NSPT.
![]() Summary
Summary
Evidence-based research is limited on the effectiveness of instruments designed for deep pockets and furcations, which is affected by host response to therapy, clinician ability, and patient’s health status. Research has concluded that both hand and ultrasonic instruments produce similar results in long-term clinical outcomes.23-25 In practice, many oral health practitioners use a blended approach for patients with moderate or advanced chronic periodontitis during initial therapy. This approach could provide root surfaces free of the smear layer and dentin tubules that are partially occluded, thus enhancing healing.26 Clinicians should expand their hand and ultrasonic instrument armamentariums to provide the most effective patient-centered care.
References
- Perry DP, Takei HH. Phase I periodontal therapy. In: Newman MG, Takei HH, Klokkevold PR, Carranza FA, eds. Carranza’s Clinical Periodontology. 11th ed. St. Louis: Elsevier Saunders; 2012:448-451.
- American Academy of Periodontology. Comprehensive periodontal therapy: a statement by the American Academy of Periodontology. J Periodontol. 2011;82:943-949.
- American Academy of Periodontology. Parameter on chronic periodontitis with slight to moderate loss of periodontal support. J Periodontol. 2000;71: 853-855.
- American Academy of Periodontology. Parameter on chronic periodontitis with advanced loss of periodontal support. J Periodontol. 2000;71:856-858.
- Bowen DM. Introduction to nonsurgical periodontal therapy. In: Hodges KO. Concepts in Nonsurgical Periodontal Therapy. Albany, NY: Delmar; 1998.
- Hodges KO. Hand-activated instrumentation. Concepts in Nonsurgical Periodontal Therapy. Albany, NY: Delmar; 1998.
- Klokkevold HH, Takei HH, Cararanza FA. General principles of periodontal surgery. In: Carranza’s Clinical Periodontology. 11th ed. St. Louis: Elsevier Saunders; 2012:525.
- Willmann D, Nield-Gehrig JS. Nonsurgical periodontal therapy. In: Foundations of Periodontics for the Dental Hygienist. Philadelphia: Lippincott Williams & Wilkins. 2011:407-408.
- Lautar CH. Periodontal diagnosis and care planning. In: Hodges KO. Concepts in Nonsurgical Periodontal Therapy. Albany, NY: Delmar; 1998: 158-159.
- Cobb CM. Microbes, inflammation, scaling and root planing, and the periodontal condition. J Dent Hyg. 2008;83:4-8
- Pattison AM, Pattison GL. Periodontal Instrumentation. 2nd ed. Norwalk, Conn: Appleton and Lange; 1992.
- Nagy RJ, Otomo-Corgel J, Stambaugh R. The effectiveness of scaling and root planing with curets designed for deep pockets. J Periodontol. 1992; 63:954-959.
- Singer DL, Long BA, Lozanoff S, Senthilselvan A. Evaluation of a new periodontal curet: An in vitro study. J Clin Periodontol. 1992:19;549-552.
- Pattison AM, Pattison GL. Scaling and root planing. In: Newman MG, Takei HH, Klokkevold PR, Carranza FA, eds. Carranza’s Clinical Periodontology. 11th ed. St. Louis: Elsevier Saunders; 2012:471.
- Oda S, Ishikawa I. In vitro effectiveness of newly designed ultrasonic scaler tip for furcation areas. J Periodontol. 1989;60:634-639.
- Vastardis S, Yukna RA, Rice DA, Mercante D. Root surface removal and resultant surface texture with diamond-coated ultrasonic inserts: an in vitro and SEM study. J Clin Periodontol. 2005;32:467-473.
- Lavespere JE, Yukna RA, Rice DA, LeBlanc DM. Root surface removal with diamond-coated ultrasonic instruments: an in vitro and SEM study. J Periodontol. 1996;67:1281-1287.
- Yukna RA, Vastardis S, Mayer ET. Calculus removal with diamond-coated ultrasonic inserts in vitro. J Periodontol. 2007;78:122-1266.
- Yukna RA, Scott JB, Aichelmann-Reidy ME, LeBlanc DM, Mayer ET. Clinical evaluation of the speed and effectiveness of subgingival calculus removal on single-rooted teeth with diamond-coated ultrasonic tips. J Periodontol. 1997;68:436-442.
- Dos Santos KM, Pinto SC, Pochapski MT, Wambler DS, Pilatti GL, Santos FA. Molar furcation entrance and its relation to the width of curette blades used in periodontal mechanical therapy. Int J Dent Hyg. 2009;7:263-269.
- Otero-Cagide FJ, Long BA. Comparative in vitro effectiveness of closed root debridement with fine instruments on specific areas of mandibular molar furcations. I. Root trunk and furcation entrance. J Periodontol. 1997;68: 1093-1097.
- Otero-Cagide FJ, Long BA. Comparative in vitro effectiveness of closed root debridement with fine instruments on specific areas of mandibular molar furcations. II. Furcation area. J Periodontol. 1997;68:1098-1101.
- Drisko CL, Cochran DL, Blieden T, et al. Research Science and Therapy Committee, American Academy of Periodontology Position paper: Sonic and ultrasonic scalers in periodontics. J Periodontol 2000;71:1792-1801.
- D’Ercole S, Piccolomini R, Capaldo G, Catamo G, Perinetti G, Guida L. Effectiveness of ultrasonic instruments in the therapy of severe periodontitis: a comparative clinical-microbiological assessment with curettes. New Microbiol. 2006;29:101-110.
- Ioannou I, Dimitriadis N, Papadimitriou K, Sakellari D, Vouros I, Konstantinidis A. Hand instrumentation versus ultrasonic debridement in the treatment of chronic periodontitis: a randomized clinical and microbiological trial. J Clin Periodontol. 2009;36:132-141.
- Aspriello SD, Piemontese M, Levrini L, Sauro S. Ultramorphology of the root surface subsequent to hand-ultrasonic simultaneous instrumentation during non-surgical periodontal treatments: an in vitro study. J Appl Oral Sci. 2011;19:74-81.
From Dimensions of Dental Hygiene. February 2012; 10(2): 44, 46-49.

 Universal Curets
Universal Curets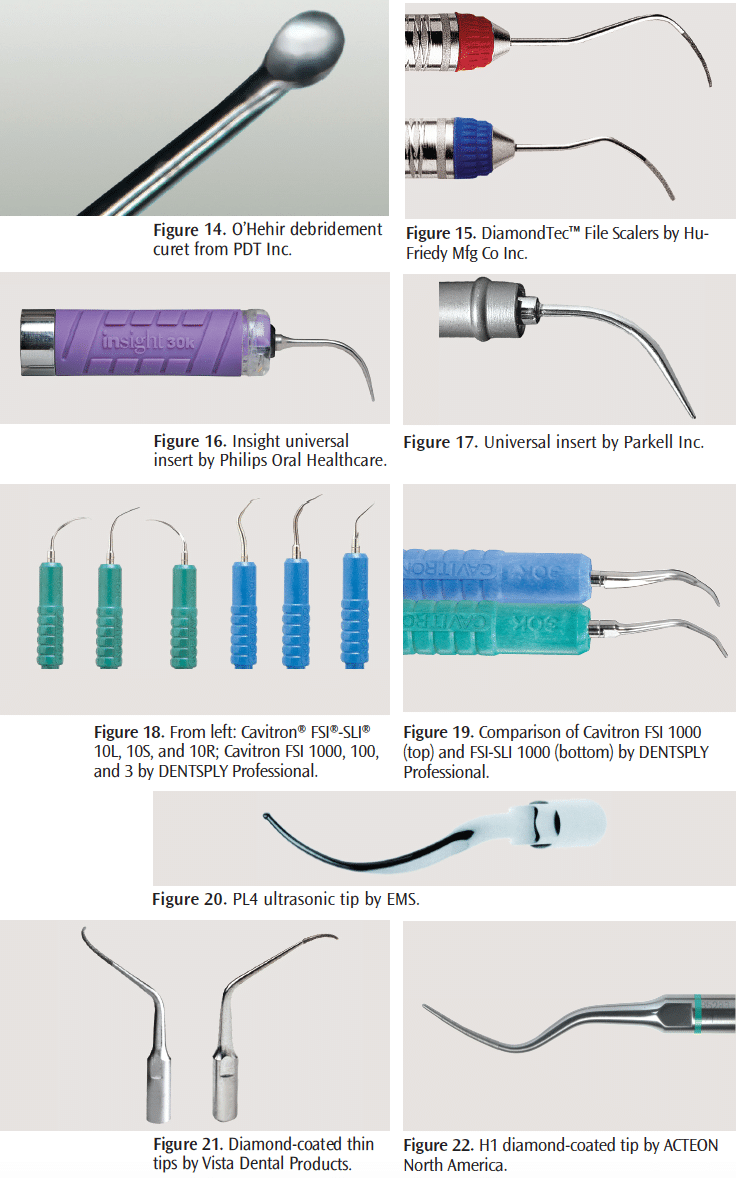 Summary
Summary