 SVITLANA HULKO / ISTOCK / GETTY IMAGES PLUS
SVITLANA HULKO / ISTOCK / GETTY IMAGES PLUS
Effective Approaches to Addressing Xerostomia
Collaboration is key when managing this common oral heath condition.
This course was published in the December 2022 issue and expires December 2025. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
AGD Subject Code: 149
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Describe considerations related to behavioral health that contribute to xerostomia.
- Identify the role of medications in xerostomia.
- Explain recommended actions a dental hygienist can take to manage medically complex
patients with xerostomia.
Affecting upwards of 29% of patients, xerostomia, or the subjective feeling of dry mouth, is associated with a variety of etiologies.1–3 Dental hygienists are at the forefront of care for patients with xerostomia and must be knowledgeable of common signs, symptoms, and management. While oral health professionals play a key role in identifying and treating xerostomia, nondental factors may also be related. An interprofessional approach can optimize care and address the potential behavioral and systemic components related to xerostomia. Table 1 presents a case about the fictitious patient, Wanda Bradsher. The case explores her oral health-related factors, assessment findings, and her medical and social histories in support of a holistic approach to care.
Behavioral Effects
Behavioral health factors, such as stress, depression, and anxiety, play a significant role in xerostomia, specifically through the decrease of salivary flow rate and increase of subjective oral dryness.4,5 Approximately 50 million Americans experienced a mental illness prior to the COVID-19 pandemic.6 Mood disorders directly impact subjective feelings of dry mouth by stimulation of anticholinergic mechanisms and by impacting the autonomic nervous system.2,7 Additionally, high stress levels increase salivary cortisol levels, creating changes in the actual composition of saliva.7 Patients with psychiatric disorders also show higher rates of xerostomia when compared to the general population.8
Patients with xerostomia and high stress levels and/or mental health conditions face additional challenges when working with oral health professionals to identify the most appropriate treatment plan. Many patients find that though psychotropic medications are effective treatments for mental health conditions, they contribute to subjective dry mouth and decreased salivary flow rates.5 The rates of mental health conditions and stress co-occurring with substance misuse continue to grow.9 Substance use at any level is strongly associated with xerostomia, including drug, alcohol, and tobacco use.10–15 Though e-cigarettes are growing in popularity, there is no current evidence suggesting an association with xerostomia.11
Associations between behavioral health factors and xerostomia underscore the importance of consistently addressing a patient’s oral health in a person-centered way in order to identify all factors impacting oral health. This process should include the use of screening questions at every visit to assess for stress, mental health conditions, and substance use. Gathering a comprehensive understanding of a patient’s medical and social history is essential to providing appropriate patient care. Table 2 provides signs and symptoms to look for in patients, as well as questions to consider asking in order to initiate conversations around behavioral health concerns.16,17
Pharmacological Effects
A significant factor to consider in xerostomia is the patient’s medication usage.3 Older adults tend to experience xerostomia at greater frequency due to the higher likelihood of taking multiple medications.18,19 Various measures are available to evaluate instances in which a patient experiences dry mouth (eg, eating a meal, swallowing) and to determine salivary flow rate.20–22 A thorough assessment is necessary to determine the degree to which a patient experiences xerostomia.
In evaluating a patient’s medication list, the mechanisms by which certain classes of medications may impact saliva production should be reviewed. The known mechanisms primarily impact the autonomic nervous system (ANS) that stimulates salivary glands, but mechanisms can also be due to medications or conditions that impact the central nervous system (CNS).18,19,23–25 The two main mechanisms in the ANS are blocking stimulation of the parasympathetic nerves and mimicking stimulation of the sympathetic nervous system. Both lead to reduced fluid volume and increased viscosity of saliva. Medication classes that block parasympathetic nerve stimulation are anticholinergics, antidepressants, antiemetics, antihistamines, antihypertensives, antimigraine, antiparkinsonian drugs, antipsychotics, anti-epileptics, antispasmodics, muscle relaxants, sedatives, and anxiolytics. Amphetamines, appetite suppressants, bronchodilators, and decongestants are common sympathomimetics.18,19,23–25
Medications that have mechanisms in the CNS impact neural effects on adrenoreceptors, inhibiting salivary nuclei (eg, opioids). In addition, some medications produce symptoms of dryness without decreasing salivary flow, including inhalers and antihypertensives (specifically diuretics). Lastly, other medications have unique xerostomia-related mechanisms, such as anti-infective agents, antineoplastic/cytotoxic agents, narcotic analgesics, and proton-pump inhibitors.19,23–25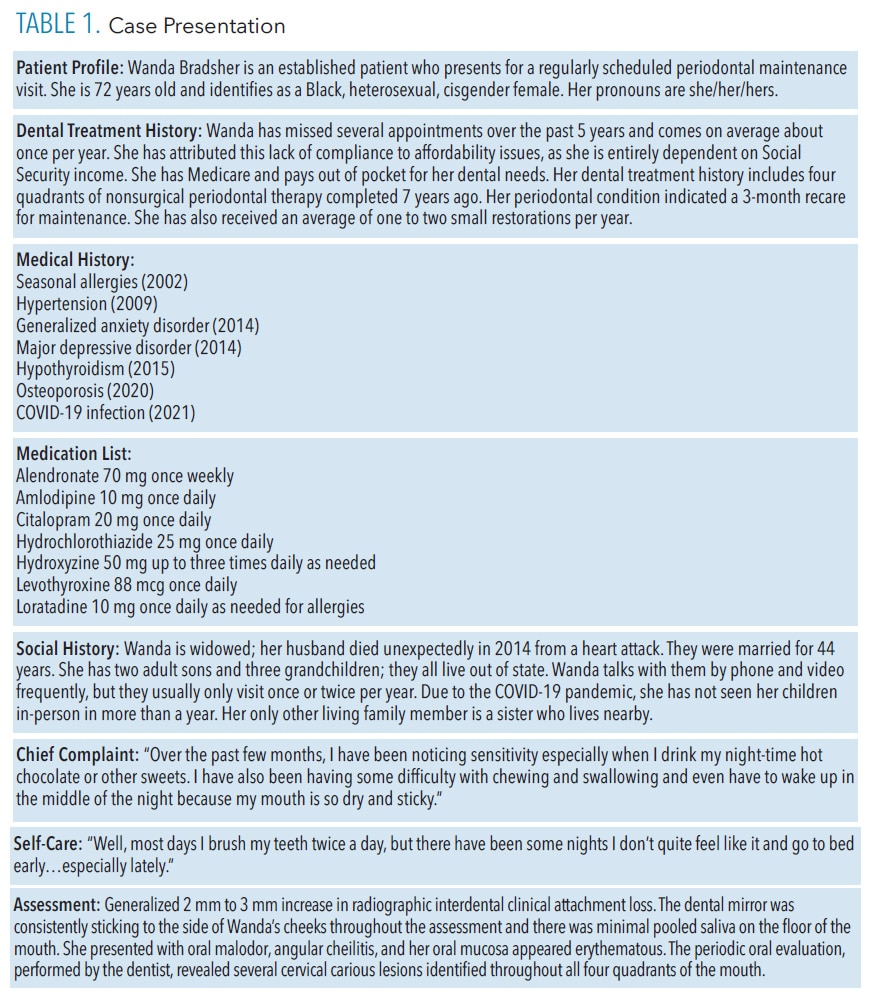
Treatment of xerostomia includes evaluating the medications causing or exacerbating xerostomia, determining the risk-to-benefit ratio, and providing treatment recommendations to soothe symptoms.19,22,26 Interprofessional collaboration of dental professionals working with their patients’ medical providers and pharmacists is essential to address chronic dryness. Table 2 indicates ways in which to ask patients specific questions about their medical conditions and medications that may impact oral health along with strategies to address xerostomia. Sometimes patients may be switched to an alternative medication that reduces dry mouth symptoms or reduces the additive impact of medications contributing to xerostomia. Even if alternative medications are not possible, adjunctive treatments may help ease the symptoms. Mechanical stimulation methods, saliva substitutes/oral lubricants, and prescription medications (pilocarpine and cevimeline) are available.19,26,27
Review of Case Presentation
In reviewing the patient’s case, several oral health considerations associated with xerostomia are noted. These are evident in her history of periodontal diseases and her chief complaint of sensitivity to sweets, difficulty with chewing and swallowing, and the feeling of dryness and stickiness at nighttime.
Dental hygienists are often attuned to the oral health manifestations of xerostomia but the nondental aspects of the case need to be considered. Clinicians may use a checklist of questions to evaluate patients from an oral health, behavioral health, and systemic health perspective. Using a checklist can further identify opportunities for connecting with other healthcare professionals.
From a behavioral health perspective, multiple psychosocial factors that could contribute to the patient’s symptoms of dry mouth are present. Most notably, the patient has a history of generalized anxiety disorder and major depressive disorder for which she was diagnosed following the death of her husband 8 years ago. She has also experienced a recent increase in social isolation due to the COVID-19 pandemic and lives on a fixed income. She is underinsured for dental needs and needs to pay out of pocket for her dental treatments. She reports that she has been going to bed early more frequently and when doing so, neglecting her typical oral health routine. Considering the correlation of xerostomia with stress, depression, and anxiety, this should be an area of emphasis during the patient history-taking.5 Additionally, an important part of this patient’s xerostomia management would be to explore how the patient manages these various psychosocial factors and connect her with community support to help decrease her stress, anxiety, and depression.
From a pharmacological perspective, the most notable factors include her diagnosis of generalized anxiety disorder and major depressive disorder for which she is prescribed citalopram and hydroxyzine. Both are antidepressant and anti-anxiety medications that contribute to xerostomia. Additionally, she has hypertension and her thiazide diuretic, hydrochlorothiazide, may impact her fluid status. She takes an antihistamine that contributes to xerostomia. Lastly, she has hypothyroidism. While the thyroid hormone supplement does not directly cause xerostomia, if it is not optimized, she could have uncontrolled hypothyroidism that contributes to symptoms of dryness and xerostomia.23 An important part of her medication management would be to explore how well the current medications are benefitting her, provide recommendations on supplemental products for managing her xerostomia symptoms, and encourage follow-up with her medical provider(s) to explore alternative agents as appropriate.
Interprofessional factors should be considered when providing care to patients with xerostomia. Collaboration with other healthcare team members can improve the signs and symptoms of xerostomia related to oral health and considers whole-person-centered care.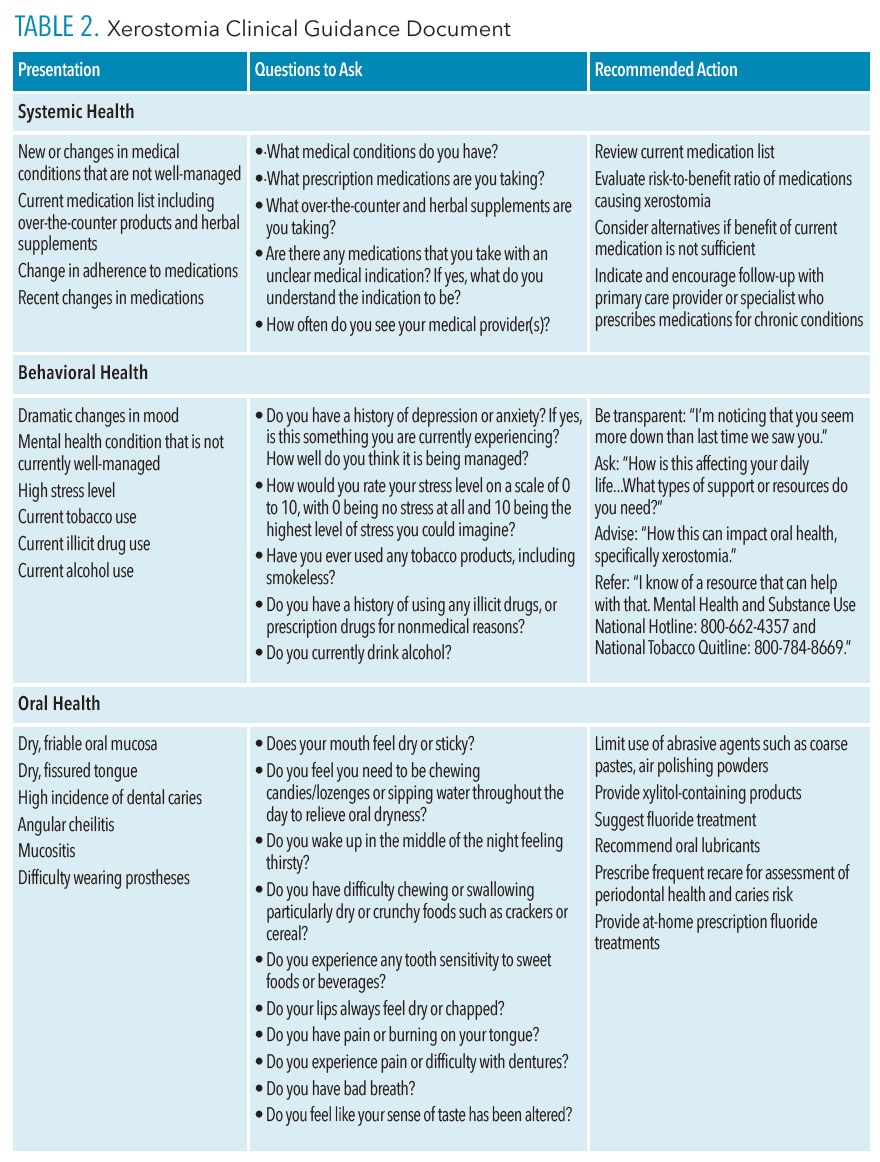
References
- American Dental Association. Xerostomia. Available at: ada.org/en/member-center/oral-health-topics/xerostomia. Accessed October 17, 2022.
- Plemons JM, Al-Hashimi I, Marek CL. Managing xerostomia and salivary gland hypofunction: a report of the ADA Council on Scientific Affairs. J Am Dent Assoc. 2014;145:867–873.
- Guggenheimer J, Moore PA. Xerostomia: etiology, recognition, and treatment. J Am Dent Assoc. 2003;134:61–69.
- United States Centers for Medicare and Medicaid Services. Behavioral Health. Available at: cms.gov/outreach-education/american-indianalaska-native/aian-behavioral-health. Accessed October 17, 2022.
- Borahan M, Pekiner F, Atalay T. Evaluation of effects of the psychological factors on saliva. MUSBED. 2012;2:S8–S14.
- Mental Health America. The State of Mental Health in America. Available at: mhanational.org/issues/state-mental-health-america. Accessed October 17, 2022.
- Gholami N, Hosseini Sabzvari B, Razzaghi A, Salah S. Effect of stress, anxiety and depression on unstimulated salivary flow rate and xerostomia. J Dent Res Dent Clin Dent Prospects. 2017;11:247–252.
- Veerabhadrappa S, Chandrappa P, Patil S, Roodmal S, Kumarswamy A, Chappi M. Evaluation of xerostomia in different psychological disorders: an observational study. J Clin Diagn Res. 2016;10:ZC24–ZC27.
- Iqbal MN, Levin CJ, Levin FR. Treatment for substance use disorder with co-occurring mental illness. Focus. 2019;17:88–97.
- Arora G, Freeman R. Oral health and addiction: Consequences of substance use. In: el-Guebaly N, Carrà G, Galanter M, Baldacchino AM, eds. Textbook of Addiction Treatment. New York: Springer, Cham; 2020.
- Chaffee B, Halpern-Felsher B, Cheng J. E-cigarette, cannabis and combustible tobacco use: associations with xerostomia among California adolescents. Community Dent Oral Epidemiol. 2021;10:1111.
- Cuberos M, Chatah E, Baquerizo, H. Dental management of patients with substance use disorder. Clin Dent Rev. 2020;4:1–8.
- Billings R, Proskin H, Moss M. Xerostomia and associated factors in a community-dwelling adult population. Community Dent Oral Epidemiol. 1996;24:312–316.
- Cassolato S, Turnbull R. Xerostomia: clinical aspects and treatment. Gerodontology. 2003;20:64–77.
- Dyasanoor S, Saddu SC. Association of xerostomia and assessment of salivary flow using modified schirmer test among smokers and healthy individuals: a preliminary study. J Clin Diagn Res. 2014;8:211–213.
- The Substance Abuse and Mental Health Services Administration. SAMHSA’s National Helpline. Available at: samhsa.gov/find-help/national-helpline. Accessed October 17, 2022.
- United States Centers for Disease Control and Prevention. Smoking and Tobacco Available at: cdc.gov/tobacco/quit_smoking/cessation/nqdw/index.htm. Accessed October 17, 2022.
- Thomson WM, Smith MB, Ferguson CA, Moses G. The challenge of medication-induced dry mouth in residential aged care. Pharmacy (Basel). 2021;9:162.
- Gil-Montoya JA, Silvestre FJ, Barrios R, Silvestre-Rangil J. Treatment of xerostomia and hyposalivation in the elderly: a systematic review. Med Oral Patol Oral Cir Bucal. 2016;21:e355–366.
- Thomson WM, Chalmers JM, Spencer AJ, Williams SM. The xerostomia inventory: a multi-item approach to measuring dry mouth. Community Dent Health. 1999;16:12–17.
- Thomson WM, van der Putten GJ, de Baat C, et al. Shortening the xerostomia inventory. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;112:322–327.
- Fornari CB, Bergonci D, Stein CB, Agostini BA, Rigo L. Prevalence of xerostomia and its association with systemic diseases and medications in the elderly: a cross-sectional study. Sao Paulo Med J. 2021;139:380–387.
- Tanasiewicz M, Hildebrandt T, Obersztyn I. Xerostomia of various etiologies: a review of the literature. Adv Clin Exp Med. 2016;25:199–206.
- Wolff A, Joshi RK, Ekström J, et al. A guide to medications inducing salivary gland dysfunction, xerostomia, and subjective sialorrhea: a systematic review sponsored by the World Workshop on Oral Medicine VI. Drugs R D. 2017;17:1–28.
- Spolarich AE. Medication use and xerostomia. Dimensions of Dental Hygiene. 2005;3(7):22–24.
- Turner MD. Hyposalivation and xerostomia: etiology, complications, and medical management. Dent Clin North Am. 2016;60:435–443.
- Barbe AG. Medication-induced xerostomia and hyposalivation in the elderly: culprits, complications, and management. Drugs Aging. 2018;35:877–885.
From Dimensions of Dental Hygiene. November/December 2022;20(11)42-45.



